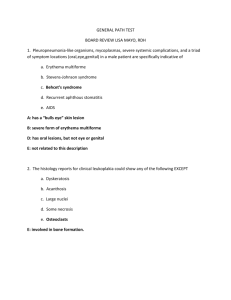
Acute Lymphoblastic Leukemia
advertisement

Acute Lymphoblastic Leukemia • Causes a wide spectrum of syndromes – From involvement of bone marrow and peripheral blood(leukemias) to those that cause masses (lymphomas) in lymphoid organs. • Arise from the HSC, the common lymphoid progenitor cell OR differentiated progenitors of the T or B cell lineage – T cell malignancies more aggressive, often involve extranodal/extramedullary sites like skin, CNS, mediastinum – Neoplastic B cells secrete monoclonal proteins( IgM, IgG, IgA) inappropriately causing increased viscosity of blood, impairing blood flow Hematologic disorders characterized by malignant neoplastic proliferation and accumulation of immature and dysfunctional hematopoietic cells in the bone marrow. Abnormality is an acquired genetic mutation within a lymphoid precursor cell that gives rise to a clone of malignant lymphocytes These “cells” proliferate in an unregulated manner and do not develop into mature cells Additionally, they have an enhanced ability to self-renew and have a resistance to cell death. • Seen in young children – Peak incidence between 2-5 years old • Onset symptoms can be insidious or abrupt – Prognosis with treatment good, if no treatment received, survival very short • Another peak seen in 60’s – Onset symptoms rapid, fatigue, infections, bruising – Prognosis not good • Symptoms are related to the replacement of normal marrow elements with leukemic lymphoblasts – Anemia, thrombocytopenia, neutropenia – Fever, weight loss, pallor, fatigue – Petechiae and eechymoses present in half of the patients – Bone pain due to expansion of bm with leukemic cells WBC variable from 0.1->50 x 109/L ◦ Usually around 10-12 x 109/L Neutropenia Lymphoblasts Normocytic, normochromic anemia Thrombocytopenia (48-52 x 109/L) Peripheral Blood Bone marrow Homogeneity of morphology of lymphoblasts Peripheral blood Bone Marrow Heterogeneous morphology of lymphoblasts Age Blood Morphology Cytochemistry ◦ AML - mainly in adults ◦ ALL - common in children ◦ AML - anemia, neutropenia, thrombocytopenia, myeloblasts and promyelocytes ◦ ALL - anemia, neutropenia, thrombocytopenia, lymphoblasts and prolymphocytes ◦ AML - blasts are medium to large with more cytoplasm which may contain granules, Auer rods, fine nuclear chromatin, distinct nucleoli ◦ ALL - blasts are small to medium with scarce cytoplasm, no granules, fine nuclear chromatin and indistinct nucleoli ◦ AML - positive peroxidase and Sudan black B, negative TdT ◦ ALL - negative peroxidase and Sudan black B, positive TdT Two subgroups ◦ B-cell neoplasms Precursor B cell Mature B cell neoplasms ◦ T-cell neoplasms Precursor T cell Mature T cell neoplasms Three phases: ◦ Induction Therapy: eradicate blast population ◦ CNS prophylactic phase: Irradiation ◦ Cytoreductive or Maintenance chemotherapy McKenzie, Shirlyn B., and J. Lynne. Williams. "Chapter 25." Introduction. Clinical Laboratory Hematology. Boston: Pearson, 2010. Print.