MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Renal Unit :Overview
MLAB 2401: Clinical Chemistry
Keri Brophy-Martinez
Renal Unit :Overview
Kidney physiology
Renal Physiology
• Three renal processes
– Glomerular filtration
– Tubular reabsorption
– Tubular secretion
Glomerular Filtration
• Glomerulus filters incoming blood
– How?
• High pressure in the glomerular capillaries sets up a pressure difference
• Semipermeable glomerular basement membrane allows small dissolved solutes, which have a positive charge to pass
• Glomerular filtrate, which is cell-free, protein free is made and can be measured by the GFR( glomerular filtration rate)
Tubular Reabsorption
• Substance movement from tubular lumen to peritubular capillary plasma for regulation of concentration
– Assists in conservation of nutrients
– Prevents electrolyte loss
– Assists in acid-base imbalance
• Occurs by Active and Passive transport
– Active Transport
• Tubular epithelial cells use energy to bind and transport substances across plasma membrane to blood
•
Transports Glucose, Amino acids, Proteins, Electrolytes
•
Maintains the sodium pump to prevent the cells from swelling up
– Passive Transport
• No energy requirement
• Substances, such as water and urea, move from higher concentrations to lower concentrations
Tubular Reabsorption
• Occurs in proximal convoluted tubule
– Receives the glomerular filtrate
– Return the bulk of substances back to blood circulation
• Proteins, glucose completely reabsorbed
• Sodium, chloride partially reabsorbed
• Creatinine no reabsorption
– Secretes products of kidney tubular metabolism, such as hydrogen ions and drug
Tubular Secretion
• Occurs in the proximal convoluted tubule
• How is this used?
– Movement of substances from peritubular capillary plasma to tubular lumen that were not previously eliminated
– Secretion of products from tubule cell cellular metabolism into filtrate, such as hydrogen
Distal Convoluted Tubule
• Most of reabsorption complete
• Function
– Make small adjustments to benefit electrolyte and acid-base balance
– Adjustments occur under control of ADH
(antidiuretic hormone) and aldosterone
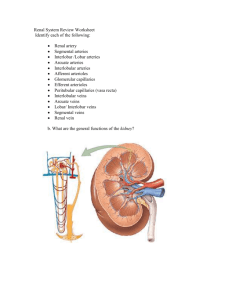
Functions of the Kidney
• Urine formation
• Fluid and electrolyte balance
• Regulation of acid-base balance
• Excretion of waste products of protein metabolism
• Excretion of drugs and toxins
• Secretion of hormones
Water Balance
• Kidney assists with water balance through water loss or water conservation
• Water balance regulated by ADH/AVP
– Secretion of ADH
• Increased plasma osmolality or decreased intravascular volume
– Action of ADH
• ADH increases the permeability of the distal convoluted tubules and collecting ducts to water
• Results in water reabsorption and concentration of urine
• Activates thirst mechanism
How does it work?
Aldosterone
• Origin
– Adrenal cortex
– Influenced by renin-angiotension system
• Secretion
– Decreased blood flow or blood pressure
– Decreased plasma sodium
• Action
– Stimulates sodium reabsorption in distal tubules and potassium and hydrogen ion secretion
– Increases water retention
– Raises blood pressure
Acid-Base Balance
• Renal system assists with constant control of overall pH
– Conserve bicarbonate ions
– Secretes H + ions attached to phosphate
– Secretes H + ions attached to ammonia
Elimination of Nonprotein Nitrogen Compounds
•
Waste products formed by degradative metabolism of proteins, amino acids and nucleic acids
• Main players are urea, creatinine and uric acid
– Urea
• 75% of the nonprotein nitrogens excreted daily
• By product of ammonia breakdown
• 40-60% reabsorbed
– Creatinine
• Formed from creatine, which is found in muscle
• Not reabsorbed by the tubules
– Uric acid
• Waste product of purine metabolism (nucleic acid)
– Ammonia
• Product of amino acid and protein catabolism
Endocrine Functions
• Produces hormones
– Renin
– Erythropoietin
– 1,25- dihydroxy vitamin D
3
– Prostaglandins
• Target for certain hormones produced by other endocrine glands
Hormones: Renin
• Released by juxtaglomerular cells
• Stimulated by decreases in fluid volume or blood pressure
• Effect of:
– Promote sodium reabsorption and water conservation
– Promotes secretion of aldosterone
• Bottom line: Increase blood pressure
Hormones: Erythropoietin
• Made by kidney
• Production regulated by blood oxygen levels (hypoxia)
• Effect of:
– Stimulate RBC production
Hormones:
1,25-Dihydroxy Vitamin D
3
• Made in the kidneys
• Active form of vitamin D
• Determines phosphate and calcium balance and bone calcification in the human body
Hormones:
Prostaglandins
• Fatty acids formed from dietary fatty acids
• Produced in the kidney
• Function
– Increase renal blood flow (vasodilator)
– Sodium and water excretion
– Antagonistic to renin release
References
• Bishop, M., Fody, E., & Schoeff, l. (2010). Clinical Chemistry:
Techniques, principles, Correlations.
Baltimore: Wolters Kluwer
Lippincott Williams & Wilkins.
• Sunheimer, R., & Graves, L. (2010). Clinical Laboratory
Chemistry.
Upper Saddle River: Pearson .
21