— The Urinary Chapter 23 System 23-1
advertisement

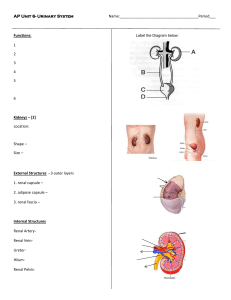
Chapter 23— The Urinary System 23-1 Ch. 23 Study Guide 1. Critically read 23.1 to right before the 23.7 (Urine Storage and Elimination) section (pp. 905-931) 2. Comprehend Terminology (those in bold) 3. Study-- Figure questions, Think About It questions, and Before You Go On (sectionending) questions 4. Do end-of-chapter questions: – Testing Your Recall— 2-10, 12-17, 19-20 – True or False– 1-9 – Testing Your Comprehension-- #1-2 2 I. Functions of the Urinary System 23-3 § Major Nitrogenous Wastes Ammonia: very toxic; from amino group in the a.a. Urea: less toxic; converted from ammonia in the __________ Uric acid: nucleic acid catabolism Creatinine creatine phosphate catabolism 23-4 § Major Nitrogenous Wastes BUN (Blood Urea Nitrogen) 1. Measure the amount of ________ in your blood 2. Why is it done? 3. Disorders: – Azotemia: an abnormally elevated BUN is called; may indicate renal insufficiency – Uremia: toxic effects as wastes (urea) accumulate in the blood; patients with renal failure • Symptoms– vomiting, diarrhea, cardiac arrhythmia etc. 23-5 • Treatment--Hemodialysis § Major kidney functions (1) 1. Eliminate wastes & foreign compounds – Major nitrogenous wastes? – Major foreign cpds? 2. Maintain blood volume and electrolyte (ion) concentration – For example, water balance during exercise – Another example, [K+] and ectopic focus 23-6 § Major kidney functions (2) 3.Produce hormones— two major ones? 4.Detoxifies free radicals and drugs 5.In times of starvation-gluconeogenesis (makes glucose from amino acids or fats) 23-7 II. Anatomy of the Kidney 23-8 § The urinary system 1. Kidneys (a pair) • Functions-- 2. The ureter (a pair) 3. The single urinary bladder • A muscular sac for _________________ 4. The urethra • Draining urine to the outside • In females vs. in males (length and external orifice) + proper toilet habits Figure 23.1 23-9 Figure 23.1b 23-10 § Gross Anatomy of Kidney 1. Renal cortex: outer 1 cm; extensions of the cortex called renal columns 2. Renal medulla: inner zone; renal columns divide the medulla into 6-10 renal pyramids (each blunt point called renal papilla) 3. The renal papilla is nestled in a cup called a minor calyx major calyx 4. Lobe of kidney: pyramid and it’s overlying cortex Fig. 23.4 + a practice figure 23-11 23-12 § Renal circulation-- Figure 23.5a C A B 23-13 Path of Blood Through Kidney • Renal artery: into segmental artery and then A--interlobar arteries (up renal columns, between lobes) B--arcuate arteries (over pyramids) C--interlobular arteries (up into cortex) afferent arterioles glomerulus (cluster of capillaries) efferent arterioles (near medulla vasa recta) peritubular capillaries interlobular veins arcuate veins interlobar veins • Renal vein 23-14 A. B. 23-15 23-16 Two kinds of Nephrons, depending upon locations 1. Cortical nephrons (85%) – short nephron loops of Henle – efferent arterioles branch off into peritubular capillaries 2. Juxtamedullary nephrons (15%) – Where? – very long nephron loops-– Vasa Recta– Efferent arterioles descend into the medulla and give rise to Vasa Recta instead of peritubular capillaries. – The capillaries of the vasa recta lead into venules that empty into the interlobular and arcuate veins 23-17 § The Nephron (1) 23-18 § The Nephron (2) 1. How many nephrons in each kidney? Answer: ___________ 2. The nephron are blood-processing units and each one of them is a functional unit of the kidneys 3. Vascular and tubular parts of the nephron • Vascular parts first--Figure 23.6, 23.7 23-19 4. Efferent arteriole 3. Glomerulus 2. Afferent arteriole 1. Interlobular Artery 6. Interlobular vein 23-20 5. Peritubular capillaries To renal pelvis Glomerular capsule & glomerulus together: Renal Corpuscle 23-21 § Vascular part of the Nephron (3) 1. The renal artery (. . . interlobular artery)– 2. Afferent arteriole – • supplies each nephron and delivers blood to the glomerulus 3. The glomerulus– cluster of capillaries (1st set of capillary in each nephron); function? 23-22 § Vascular part of the Nephron (4) 4.The efferent arteriole— • Where the glomerular capillaries rejoin 5.The peritubular (2nd set of) capillaries-• Impt in exchanges between blood and ______________ 6.The renal veins-• The major blood vessels leave the kidney --------------------------------------------------------------- • Tubular parts of the nephron– @Fig. 23.8 23-23 1. Bowman’s capsule 4. Distal tubule 2. Proximal tubule Glomerulus Artery Vein 5. Collecting duct Cortex Medulla 3. Loop of Henle (nephron loop) To renal pelvis 23-24 § Tubular part of the Nephron (5) • A hollow tube formed by a single layer of epithelial cells; They are, in order: 1.Bowman’s (Glomerular) capsule– • Cup-shaped; double-wall invagination • Surround each __________ 2.Proximal tubule– closest to Bowman’s capsule • Lies entirely within the cortex 23-25 § Tubular part of the Nephron (6) 3.The loop of Henle (nephron loop)– • Forms a U-shaped loop 4.The distal tubule– • most distant from the capsule; lies entirely within the ____________ 5.Collecting tubule/duct— • drains fluid from up to 8 nephrons Figure 23.8 23-26 1. Figure 23.8b 2. ID parts (1-5) of the nephron. 3. 4. 5. 23-27 Questions? Muddiest points? 23-28 III. Urine Formation 23-29 § Three urine forming processes 1.-- Glomerular filtration • From the glomerulus into Bowman’s (glomerular) capsule 2A.--Tubular reabsorption • From the tubular lumen into ___________ 2B.--Tubular secretion • From the peritubular capillaries into the __________________ 3.-- Water conservation Figure 23.9 23-30 Different names (fluid in renal tubules) in different areas: 1. Glomerular filtrate (in the capsular space) 2. Tubular fluid (proximal tubule to distal tubule) 3. Urine (collecting duct and beyond) 23-31 III. Urine Formation; 1. GLOMERULAR FILTRATION 23-32 § 1. Glomerular filtration A. Def.– filtering blood by forcing small molecules into the Bowman’s capsule B. What in the filtrate? • Small molecules can pass— • Large molecules cannot— C. Mechanism? ATP? • What is the major force? Glomerular blood hydrostatic pressure (BHP) 23-33 § 1. Glomerular filtration (cont.) D. Layers of the glomerular filtration mem. i. 1-Fenestrated endothelium of capillaries • Large pores (100x more permeable) • Molecules can pass– ii. 2-(Acellular) basement mem. • Collagen & glycoproteins • Function-- iii. 3a-Filtration slits; present in inner layer of the Bowman’s capsule-- podocytes (3b) bear many foot processes (pedicles) Figure 23.10 (a-d) 23-34 Afferent arteriole Efferent arteriole Glomerulus Bowman’s capsule Lumen of Bowman’s capsule Outer layer of Bowman’s capsule Inner layer of Bowman’s capsule (podocytes) Proximal convoluted tubule Lumen of glomerular capillary Endothelial cell Basement membrane(see Podocyte foot process next slide) 23-35 3b. Podocyte & foot process 3a.Filtration slits 2. Basement membrane 1. Capillary pore 23-36 1a. Capillary pore 1b. Endothelial cell Lumen of glomerular capillary 2. Basement membrane 3a.Filtration slit 3b. Podocyte foot process Lumen of Bowman’s capsule (capsular space) 23-37 A. Endothelial cell Lumen of glomerular capillary B. Filtration slit Lumen of Bowman’s capsule C. 23-38 § 1. Glomerular filtration (cont.) Disorders: 1.Albuminuria– also called proteinuria; presence of ________ in the urine • Criteria: >250 mg/day: pathological 2.Hematuria– presence of ______ in the urine 23-39 III. Urine Formation; 2A. TUBULAR REABSORPTION 23-40 § 2. Tubular reabsorption 1. Def. reclamation process to move molecules back into the blood 2. Goal: to move molecules from tubular lumen to the peritubular capillaries (or vasa recta) Table x & Figure y 23-41 § 2. Tubular reabsorption (cont.) Table x Substances in filtrate % of filtered substances reabsorbed % of filtered substances excreted 99 1 Sodium 99.5 0.5 Glucose 100 0 Urea 50 50 0 100 Water Phenol 42 § 2.Tubular reabsorption (cont.) 1. What are reabsorbed? • All the glucose, vitamins, and . . . 2. How efficient? • Glucose— no glucose escapes • Water— 180 L filtrate to 1-2 L of urine/day • Analogy— Clean out a cluttered drawer 23-43 III. Urine Formation; 2A. TUBULAR REABSORPTION– in the proximal convoluted T. 23-44 § 2. Tubular reabsorption (cont.) Two examples—Na+, water in proximal convoluted tubules and beyond 3.--1st example– sodium reabsorption • Where are sodium ions been reabsorbed? Most of the tubule Exception is the descending limb of the loop of Henle • Routes taken: both transcellular and paracellular routes 23-45 § 2. Tubular reabsorption (cont.) • Mechanisms of sodium reabsorption— – A--symport proteins (channels)— – B--Na+-H+ antiport— – C--Na+-K+ pumps– basal and lateral membrane – D– Paracellular route-Figures 23.16 23-46 23-47 § 2 Tubular reabsorption (cont.) 4. --2nd example– water reabsorption Locations? All the renal tubule; however, 2/3 occurs in PCT • Mechanisms— Via water channels (aquaporins) Between cells Water moves into blood plasma Figures 23.16 23-48 23-49 § Reabsorption Limit 1. Def.-- A limit to the amount of solute the renal tubule can reabsorb 2. Why? Limited no. of transport proteins 3. Tm = Transport maximum; example-– Glucose’s Tm is 320 mg/min – Glucose normally enters the renal tubule at 125 mg/min; will all of it be reabsorbed? – Threshold of glucose in the plasma– 220 mg/dL (= 220mg/100mL); begin to see glucose in the urine called glycosuria – Untreated diabetes mellitus patients– 400 mg/dL (plasma glucose) 23-50 23-50 III. Urine Formation; 2A. TUBULAR REABSORPTION– in the nephron loop 23-51 § The nephron loop (loop of Henle) • Primary function— to generate a salinity gradient that enables the collecting duct to concentrate the urine and conserve water • Mechanism— – Thick segment (ascending limb) of the loop: Impermeable to water – Tubular fluid becomes very dilute by the time it reaches the DCT Fig. 23.19 23-52 23-52 Cortex Low Increasing Osmolarity High Nephron loop Medulla 23-53 III. Urine Formation; 2A. TUBULAR REABSORPTION– in the distal convoluted tubule and collecting duct 23-54 § DCT and collecting duct (CD) • Reabsorption regulation– by several hormones including aldosterone etc. (see following slides) • Cells here in DCT and CD— A. PRINCIPAL CELLS– – more abundant; they have receptors for these hormones – Functions– involved in salt and water balance B. INTERCALATED CELLS– – fewer; functions– in acid-base balance 23-55 23-55 § Aldosterone (1) • Chemistry – peptide, steroid, or monoamine? (which one) • Secreted by – the adrenal cortex • Function-- to promote sodium retention and increase blood pressure • Triggered by – – low blood sodium concentration – a drop in blood pressure (via renin) Fig. 23.15 23-56 ReninAngiotensinAldosterone mechanism 23-57 § Aldosterone (2) • Acts on– three areas in the kidneys – the thick segment of the ascending limb of the nephron loop – The DCT – The cortical portion of the collecting duct • Physiology Effects— – Retain NaCl and water – Maintain blood volume 23-58 § Atrial Natriuretic Peptide (1) • Chemistry – • Secreted by – atrial myocardium of the heart • Triggered by – high blood pressure 23-59 § Atrial Natriuretic Peptide (2) • Physiology Effects– – Promoting sodium and water loss – Reducing blood volume and pressure • Actions— on Kidney – Dilates the afferent arteriole and constricts the efferent arteriole – Inhibits renin and aldosterone secretion – Inhibits ADH secretion and the action of ADH on the kidney – Inhibits NaCl reabsorption by the collecting duct 23-60 III. Urine Formation; 2B. TUBULAR SECRETION 23-61 § Tubular secretion 1. Process— transfer of selective molecules from the capillary blood and secrete them into the ___________ 2. Locations– PCT, nephron loop, DCT 3. Purposes— – Waste removal— • For example— – Acid-base balance– hydrogen and bicarbonate ions Fig. x 23-62 Blood pathway Fig.-- the nephron & molecule movements (demo) Glomerular capillaries Efferent arteriole Glomerular filtration Bowman’s capsule Peritubular capillaries Tubular reabsorption Filtrate pathway Venous blood Tubular secretion Tubule (from proximal tubule to collecting duct) Urine 23-63 III. Urine Formation; 3. WATER CONSERVATION The principal function left to the collecting duct is to conserve water. 23-64 § The Collecting Duct (CD) 1. Location – – Begins in the cortex and passes through the medulla 2. Mission – it reabsorbs water and concentrates the urine 3. Mechanisms— – Osmolarity of the ECF is ______ times as high in the lower medulla as it is in the cortex – Medullary portion of the CD is more permeable to _______ than to NaCl Fig. 23.19 23-65 Figure 23.17 Cortex Medulla Which portion of the renal tubule? 23-66 § Control of water loss How concentrated the urine becomes depends on the state of hydration 1. Dehydration– your urine becomes little & more concentrated: – High blood osmolarity release ADH (more/less; circle one) – renal tubule synthesize aquaporins – install them in the plasma mem. – CD reabsorbs more water 2. Well hydrated– opposite to the above 23-67 23-67 § Countercurrent Multiplier (1) 1. The ability of the collecting duct to concentrate urine depends on the salinity gradient of the renal medulla. – Mechanism behind this: The nephron loop acts as a countercurrent multiplier – Result: the nephron continues to return salts to the deep medullary tissue – Hence it is called multiplier b/c it multiplies the salinity deep in the __________ – Countercurrent? Fluid flows in opposite directions. Where? Descending limb and ascending limb of the nephron loop Fig. 23.20 23-68 23-68 1 2 PCT DCT Cortex 5 Medulla 3 4 Nephron loop 23-69 § Countercurrent Multiplier (2) 2. How countercurrent multiplier works? A. Medulla-- An environment of increasing salinity toward deeper part of medulla B. Descending limb (nephron loop)– very permeable to _______ but not to NaCl C. Ascending limb– impermeable to _____, but has pumps to transport ions – Keeps the osmolarity high in medulla – Tubular fluid: more and more diluted toward the distal tubule 23-70 § Countercurrent Multiplier (3) 3. In the lower end of collecting duct (CD)– urea helps to maintain (40%) the osmotic gradient in medulla How? – Lower end of CD is permeable to urea; urea diffuses into the ECF – Urea enters the descending thin segment; but the thick segment of the loop and DCT is NOT permeable to urea – Therefore, continual recycling of urea from the CD to the medulla and back Fig. 23.21 23-71 Next slide 23-72 § Countercurrent Exchange System 1. Vasa recta that supply the medulla recycle the salt and urea; How? – Blood flows in opposite directions in adjacent parallel capillaries called countercurrent exchange system – It flows downward– exchanges water for salt – It flows back toward the cortex– exchange salt for water – Thus, vasa recta gives the salt back and DO NOT subtract from the osmolarity of the medulla 23-73 IV. Urine and Renal Function Tests 23-74 § Urine Volume (1) 1. Normally, 1-2 liters of urine per day 2. Polyuria (or diuresis)– output in excess of 2 L/day (detail next slide) – Causes– fluid intake, some drugs, diabetes 3. Oliguria– output of less than 500 mL/day 4. Anuria– output of 0-100 mL/day – Causes– kidney disease, dehydration, etc. – Result-- Azotemia 23-75 § Urine Volume (2) 5. Polyuria (details)— A. Results from all four forms of diabetes— • Diabetes mellitus type I, type II, gestational diabetes (all three above are due to hyperglycemia), and diabetes insipidus (due to ADH hyposecretion) B. Diabetes mellitus and gestational diabetes are glycosuria but NOT in diabetes insipidus patients 23-76 § Urine Volume (3) 6. Diuretics— def. chemicals that increase urine volume – Mechanisms– A. increasing glomerular filtration rate (GFR) or B. reducing tubular reabsorption – Example 1: Caffeine, dilates the afferent arteriole and increases GFR (due to A or B above; circle one) – Example 2: Alcohol inhibits ADH secretion (due to A or B above; circle one) 23-77 § Renal Clearance 1. Def.– the volume of blood plasma from which a particular waste is completely removed in 1 minute; Example: A. B. C. – Urea concentration in urine = 6.0 mg/mL Rate of urine output = 2 mL/min Urea concentration in plasma = 0.2 mg/mL Renal clearance = AB/C = (6.0 mg/mL x 2 mL/min)/0.2 mg/mL = 60 mL/min – This means the equivalent of 60 mL of blood plasma is completely cleared of urea per minute • Renal clearance of glucose? (healthy adults) 23-78 § Glomerular filtration rate (GFR)-(1) 1. Def.– the rate at which glomerular filtrate is formed; volume of filtrate formed each minute by all glomeruli; Example: Inulin (no tubular reabsorption, nor tubular secretion) A. B. C. D. Urine concentration of inulin = 30 mg/mL Urine output is = 2 mL/min Plasma concentration of inulin = 0.5 mg/mL GFR = AB/C = (30 x 2)/0.5 = 120 mL/min = Renal clearance of inulin (why?) (next slide) 79 § Glomerular filtration rate (GFR)-(2) For inulin, GFR (120 mL/min) is equal to the renal clearance. Why? 1. All inulin filtered by the glomerulus remains in the renal tubule and appears in the urine. 2. A solute that is reabsorbed by the renal tubules will have renal clearance less than the GFR; renal clearance of urea @ 60 mL/min 3. A solute that is secreted by the renal tubules will have a renal clearance greater than the GFR; renal clearance of creatinine @ 140 mL/min 80