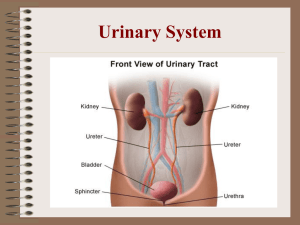
Urinary System
advertisement

Urinary System Urinary System 2 kidneys Two ureters Urinary bladder Urethra Functions of the Urinary System Formation of urine = kidneys - rids body of waste products such as urea, creatine and ammonia • Elimination of urine= ureters, bladder, urethra • Regulation of the volume of blood by excretion or conservation of water Regulation of the electrolyte content of the blood • Regulation of the acid-base balance of the blood • Kidneys Located in upper abdominal cavity on either side of the vertebral column Are enclosed and protected by the lower rib cage Embedded in adipose tissue that act as cushion and fibrous conn. Tissue which helps hold kidneys in place Hilus: indention on the medial side of each kidney - Renal artery= branch of the abdominal aorta - Renal vein= returns blood to the inferior vena cava Internal Kidney Structure The kidneys are composed of three distinct areas: 1. Renal cortex- outer layer 2. Renal medulla- inner layer 3. Renal pelvis- inner cavity Internal Structure of Kidney • Renal cortex - Outer tissue layer - Made of renal corpuscles and convoluted tubules (parts of nephron) Renal medulla - Made of loops of Henle and collecting tubules - Consist of wedge-shaped pieces called renal pyramids Internal Structure of Kidney Renal pelvis - Cavity formed by the expansion of the ureter within the kidney at the hilus - Funnel shaped extensions of the renal pelvis called calyces - Urine flows from the renal pyramids into the calyces, then to the renal pelvis and out into the ureter The Nephron Structural and functional unit of the kidney Each kidney contains 1 million nephrons It is here that urine is formed 2 major portions - Renal corpuscle - Renal tubule The Nephron Cont. 3 basic functions 1. Glomerular filtration 2. Tubular reabsorption 3. Tubular secretion Renal Corpuscle The renal corpuscles are the sites where the process of urine formation begins with a filtrate of blood plasma The renal corpuscle consist of a glomerulus surrounded by a Bowman’s capsule The glomerulus is a capillary network, composed of an afferent and efferent arteriole Renal Corpuscle Blood enters the glomerulus through the afferent arteriole Blood leaves the glomerulus through the efferent arteriole The glomerulus is suspended within the Bowman’s capsule, and are supported by podocytes within the Bowman space Renal Tubule Continues from the Bowman’s capsule, and can be found in both the renal cortex and renal medulla There are four parts of the renal tubule 1. Proximal tubule, in the cortex, is the beginning of the tubule; reabsorbs minerals and nutrients from the tubular fluid and passes them to blood Renal Tubule 2. Loop of Henle, dips into the medulla where it helps establish the hypertonic saline environment within the medulla, which allows for the recovery of water 3. Distal convoluted tubule returns near the corpuscle; it pumps ions and molecules through its gradient Renal Tubule 4. Collecting ducts collect urine from the distal tubules (found in medulla) All parts are surrounded by peritubular capillaries which arise from the efferent arteriole Glomerular Filtration In glomerular filtration, blood pressure forces plasma, dissolved substances, and small proteins out of the glomeruli and into Bowman’s capsule The fluid is no longer plasma but is called renal filtrate Tubular Reabsorption Tubular reabsorption takes place from the renal tubules into the peritubular capillaries. Peritubular capillaries arise from the efferent arteriole, and receives materials reabsorbed by the renal tubules Approx. 99% of renal filtrate is absorbed back into the blood in the peritubular capillaries. 1% becomes urine Four Mechanisms of Reabsorption 1. Active transport- the cells of the renal tubule use ATP to transport filtrate to the blood 2. Passive transport- negative ions that are returned to blood are reabsorbed 3.Osmosis- the reabsorption of water follows the reabsorption of minerals 4. Pinocytosis- occurs in the proximal tubules, by enveloping small proteins Tubular Secretion Changes the composition of urine Substances are actively secreted from the blood in the peritubular capillaries into the filtrate in the renal tubules Waste products such as ammonia, some creatine, and medication may be secreted into the filtrate to be eliminated Other Functions of Kidney 1. Secretion of renin- when blood pressure decreases cells in the afferent arteriole secrete the enzyme renin; which triggers the renin-angiotensin mechanism and the production of aldosterone 2. Secretion of erythropoietin- stimulates the red bone marrow to increase the rate of RBC production; which increases oxygen carrying capacity Other Functions 3. Activation of vitamin D- vitamin D is converted to calciferol by the kidneys. Calciferol increases the absorption of calcium and phosphate in the small intestine Dialysis Separation of large particles from smaller ones through a selectively permeable membrane Hormones that affect kidneys Antidiuretic hormone (ADH)- Increases reabsorption of water Aldosterone- increases reabsorption of Na and excretion of K+ Atrial natriuretic hormone (ANH)Decreases reabsorption of Na+ Renal Failure Inability of the kidney to function properly 3 Causes 1. Prerenal- problem is before the kidneys, decrease blood flow (hemorrhage) 2. Intrinsic- problem is in kidneys (bacterial infections) 3. Postrenal- problem is after kidney, obstruction of urine flow (kidney stones) Floating Kidney A floating kidney is one that has moved out of its normal position. If a ureter becomes twisted or kinked, urine cannot flow properly. This could lead to urine backing up into the renal pelvis, and Bowman’s capsule, ultimately causing permanent kidney damage. Ureters Ureters extend from the hilus of a kidney to the lower, posterior side of the urinary bladder The smooth muscle in the walls of the ureter contracts in peristaltic waves to propel urine toward the urinary bladder Urinary Bladder The urinary bladder is a muscular sac below the peritoneum and behind the pubic bone In women, the bladder is inferior to the uterus In men, the bladder is superior to the prostate gland Urinary Bladder The mucosa of the bladder is transitional epithelium, which permits expansion without tearing the lining. When the bladder is empty, the mucosa appears wrinkled; the folds are called rugae and permit expansion The trigone is a triangular area on the floor of the bladder, it has no rugae and does not expand The points of the triangle are the two ureters and the urethra Urinary Bladder The detrusor muscle is the smooth muscle layer of the bladder which contracts and decreases its volume The muscle fibers of the detrusor form the internal urethral sphincter or sphincter of the bladder (involuntary) Urethra The urethra carries urine from the bladder to the exterior The external urethral sphincter is made of skeletal muscle (voluntary) In women the urethra is 1 to 1.5 inches long In men the urethra is 7 to 8 inches long, and carries semen as well as urine Micturition (Urination Reflex) The urination reflex is a spinal cord reflex in which voluntary control can occur The stimulus for the reflex is stretching of the detrusor muscle of the bladder The bladder can hold as much as 800ml of urine, but the reflex is activated around 200 to 400 ml When the limit is reached impulses travel to the sacral spinal cord Aging With age the number of nephrons decrease, often by half The urinary bladder decreases in size and tone The chance of infection also increases, because of residue left behind during micturiiton Kidney Stones Kidney stones are crystals of the salts that are present in urine, and block the flow of urine in the ureter Kidney stones are most likely to form in the renal pelvis Urinary Tract Infection Infection of a part of the urinary system Symptoms include burning or painful urination If chronic, scar tissue forms and impairs function Bright’s disease Inflammation of the glomeruli Caused by bacteria Endothelial space becomes highly permeable to blood and protein Renal Failure 1. 2. 3. Acute is a decrease in glomerular filtration Chronic is the irreversible decline in glomerular filtration Diminished- up to 75% Renal- 75% End stage- 90% Causes edema, acidosis, anemia Polycystic kidney disease Inherited disorder (1:1000) Tubules become filled with cyst Apoptosis occurs in tubule cells Diabetes Insipidus Excretion of very dilute urine Patients exhibit extreme thirst The cause of DI is the defect in the production of ADH