Immune System Part III: Adaptive Immune System & Cell Mediated Immunity
advertisement

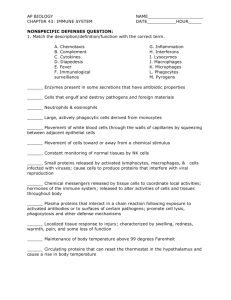
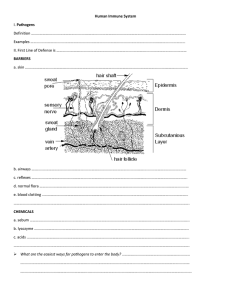
Immune System Part III: Adaptive Immune System & Cell Mediated Immunity Adaptive Immunity (Specific Immunity) Third Line of Defense • Develops after exposure to pathogens • Involves very specific response to pathogens • Much slower than innate immunity • Requires support of innate immunity to function • Two parts: • humoral immunity and • cell mediated immunity 2 Adaptive Immunity Lymphocytes—Specialized Cells •B cells- are synthesized and mature in the red bone marrow with characteristic plethora of rough E.R. •T cells- are synthesize in bone marrow but mature in the thymus with an abundance of free floating ribosomes Immature B and T cells are virtually indistinguishable. Adaptive Immunity and Primary Lymphatic Tissue Primary lymphatic tissue All lymphocytes originate in the red bone marrow. T cells then migrate to, and mature in, the thymus. B cells remain in the marrow to mature. 4 T cell receptor sites T cells have T cell receptor (TCR) sites that can attach to an antigen that is presented by another cell such as a macrophage or dendritic cell. 5 B Cell Receptor Sites and Antibody Structure B cell receptor (BCR) sites • Each one can attach to two antigens. • • Made of four poly-peptide chains held in place by covalent bonds known as disulfide bridges. Two identical heavy chains and two identical light chains with variable and constant regions. • Antibodies also have this same construction. 6 Secondary Lymphatic Tissue Where Lymphocytes are Activated Four Characteristics of Adaptive (Specific) Immunity 1. Self/Nonself Recognition - T cells and B cells have the ability to recognize one’s own cells versus a pathogen (invader). 2. Specificity - Lymphocytes are tailored to combat specific antigens due to the great diversity of B cells and T cells. 3. Diversity - There are potentially billions of different antigen receptors on B cells and T cells that recognize billions of different antigens. 4. Memory - Immune system is capable of “remembering” a pathogen once exposed. 8 Self Versus Non-self Major Histocompatibility Complex (MHC) Major Histocompatibility Complex (MHC) Proteins are cell surface proteins that are unique for each individual (except for identical twins). • Three classes of MHC proteins - MHC I, II, and III. • MHC I proteins are on ALL cells and MHC II proteins are on antigen presenting cells (B cells, macrophages, dendritic cells). 9 Major Histocompatibility Complex (MHC) • Four polypeptide chains with cleft to attach to antigens which are small polypeptide chains. • Extremely polymorphic with some classes having as many as 500 different alleles. • Antigens can attach to the cleft. 10 Major Histocompatibility Complex (MHC) • MHC I and II proteins have the ability to attach to foreign material (small polypeptides) and transport the foreign polypeptides to the surface of the infected cell. • Antigen presenting cells (APC) are mostly phagocytes. As APC are in the process of cleaning up an infection, bits and pieces of the pathogens are displayed on the MHC proteins. 11 Recognizing Self from Non-self for T cells T cells migrate to and mature in the thymus with interaction of dendritic cells. 12 T Cells Recognizing Self from Non-self Three possible outcomes: 1. TCR binds to a dendritic cell with body’s own proteins and MHC protein. Apoptosis is induced and T cell dies 2. TCR weakly binds to a dendritic cell with MHC with no proteins. T cell survives. 3. TCR does not bind to any MHC protein. Apoptosis is induced and the T cell dies. 13 T Cells Recognizing Self from Non-self Surviving T cells (called naïve T cells) can recognize MHC proteins that have some foreign protein in the cleft. It must be a double match. T cells ignore MHC proteins without any foreign material in the cleft or healthy cells. 14 B cells Recognizing Self from Non-self • Mature in the bone marrow. • If the receptor site on a B cell matches a surface protein found on bone marrow cells, apoptosis occurs. • The B cells that survive (naïve B cells) are those that will ignore the body’s own surface proteins but will recognize foreign material. 15 A Few Self-Reactive B and T Cells Do Survive • NOT all self-reactive B and T cells are destroyed. Those few that do survive, are suppressed to insure that the self-reactive B and T cells DO NOT react with the body’s own tissue. • More on this later. • Once mature, naïve B and T cells migrate out of the secondary tissue to wait to be selected. 16 Specificity and Diversity of Immune System The specificity and diversity of adaptive immunity lies in the receptor sites on B and T cells and production of free floating antibodies. 17 Structure of Antibodies Are Like B Cell Receptors B cells produce proteins called antibodies that interact with pathogens. The basic structure is similar to that of the B cell receptors. Antibodies are a part of the humoral response 18 Genes of Receptor Sites and Antibodies 19 Adaptive Immune System (Specific Immune System): Cell Mediated Immunity Adaptive Immune System: Two Components 1. Cell Mediated Immunity- Selected T cells recognize and destroy infected body cells and cancer cells. 2. Humoral Immunity- Selected B cells produce copious amounts of antibodies to fight pathogens. 20 Cell Mediated Immunity-Needs the Support of Innate Immunity (Nonspecific Immunity) The cell mediated immunity needs the support of the cells involved in the innate immunity. The dendritic cells and macrophages are used to present antigens to select and clone T cells in the secondary lymph tissues. The secondary lymph tissue includes tonsils, adenoids lymph nodes, etc. 21 Cell Mediated Immunity 1. Macrophages and dendritic cells arrive at the site of infection. 2. Phagocytosis occurs. 3. Both types of cells have MHC I and MHC II proteins. 22 Role of the Macrophage or Dendritic Cell 4. The antigen (AG) combines with either a MHC I or MHC II protein 5. Complex migrates to the cell surface to become antigen presenting cell. Cytotoxic T cells are Selected and Cloned • APC cell migrates to secondary lymphoid tissues. • Begins searching for a match with a T cell. • If the match is with MHC I protein, the T cell becomes cytotoxic cell or memory cell. Helper T Cells If the MHC II protein makes a match with the T cell, the T cell is destined to become a helper T cell and memory helper T cells. More on this later. Dendritic Cells • Dendritic cells are found in skin and other tissues that interact with the environment. • Involved in being APC to T cells T Cells and Cell Signaling Explain how the previous slides illustrate the process of cell signaling or cell communication. Pathogens Invade Body Cells • While appropriate T cells are being selected and cloned, body cells are becoming infected. • Bits and pieces of the pathogen end up on the MHC I protein of the body cell. 28 Matching T Cells with Infected Cells • The body cell is tagged as infected. • Selected cytotoxic cell recognizes the infected body cell and attaches to the cell. Cytotoxic Cells Destroy Infected Cells • Once attached, the cytotoxic cell secretes perforin which makes pores in the membrane of the infected cell. • The cytotoxic cell also secretes granzymes which cause the infected cell to die. Cytotoxic Cells Destroy Infected Cells This is another rendition of how a cytotoxic cell kills in infected cell. Below is a cytotoxic cell (orange) killing a cancer cell (purple) 31 Cell Mediated Immunity Summarized Homeostasis • Regulatory T cells (Treg) help to halt the immune response. • Do not know how they are activated possibly through antigens. • Thought to stop any further naïve B or T cells from being activated. Then the immune response stops because activated immune cells die due to their short life span. Created by: Carol Leibl Science Content Director National Math and Science