An Approach for Sub-Saharan Africa 2010 Dr. Linda hawker
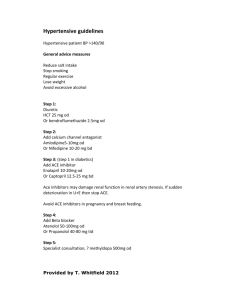
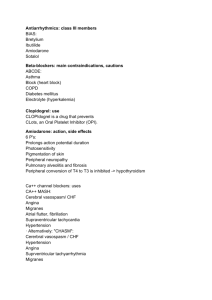
advertisement
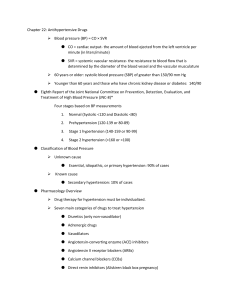
An Approach for Sub-Saharan Africa 0CTOBER 2010 Dr. Linda Hawker, MD, CCFP General Practice Kelowna BC Canada Contents based on the WHO CVD - Risk Management Package For low and medium resource settings 2002 “Hypertension plays a major role in the development of cerebrovascular disease, ischemic heart disease, cardiac and renal failure. Treating hypertension has been associated with about a 40% reduction in the risk of stroke and about a 15% reduction in the risk of myocardial infarction.” “Hypertension remains inadequately managed everywhere.” (2003 WHO / ISH statement on the management of hypertension) Appropriate assessment and management of cardiovascular risk is vital to prevent fatal and non fatal heart attacks and strokes and to improve health outcomes of those at high risk of cardiovascular disease (CVD). Hypertension is a major risk factor in development of CVD. Three major risk categories Likelihood of stroke, heart attack in next 10 years: ◦ 1. Low risk : less than 15% ◦ 2. Medium risk : 15 – 20% ◦ 3. High risk: more than 20% High Blood pressure Males over 55 years Females over 65 years Smoking Total cholesterol > 6.1 mmol/l LDL (“bad”) cholesterol > 4.0 mm/l HDL (“good”) cholesterol , M<1, F<1.2mmol/l History of CVD in parents, siblings or children before age 50 Obesity, physical inactivity Left ventricular hypertrophy (EKG or echo) Microalbuminuria (20- 300 mg/day) X –ray or ultrasound evidence of artery plaque (aorta, carotid, coronary, femoral) Hypertensive retinopathy grade 3 or 4 Diabetes History of TIA or stroke Heart disease : angina, heart attack, congestive failure Kidney disease : ◦ High creatinine: Females >120, Males >133umol/l ◦ Albuminuria >300 mg/day or >0.3 gms/L random History of Peripheral Vascular Disease Blood Risk factors Disease History : Pressure 140-159 90-99 160-179 100-109 >180 >110 Medium risk High risk No other risk factors: Low risk 1- 2 risk factors: Medium risk Medium risk High risk 3 or more risks Or TOD, or ACC: High risk High risk High risk BP < 140/90 if uncomplicated BP < 130/80 if Diabetes Chronic renal disease History of heart disease, TIA, stroke,PVD Manage risk factors, TOD and ACC Educate your patients Lifestyle Modification ◦ Weight reduction – aim for BMI 25 or less ◦ Limit salt intake – one teaspoon per day or less! ◦ Limit alcohol – 2 drinks/day men,1drink/day women ◦ Stop smoking ◦ Regular exercise – brisk walk for 30-60 min/day ◦ Healthy diet – low in fat, sugar and refined foods, high in fresh fruits, vegs, fish. Low fat dairy foods. ◦ Reinforce lifestyle message at every visit For most patients, if there is no compelling reason for another class of drug, a low dose diuretic should be the first choice of therapy. The major classes of drugs are equal in effectiveness and safety. If there is a specific indication (eg: renal disease), use the most cost effective drug of the appropriate class. 1. Thiazides ◦ Moduret (combo amiloride, HCT) 2. Beta Blockers Atenolol, Propanolol 3. Calcium Channel Blockers Nifedipine (short acting-not recommended) 4. ACE Inhibitors Captopril 5. Other: hydralazine, methyldopa Start with low dose thiazide diuretic, then add: Kidney disease +/- Diabetes: ACE inhibitor Heart disease: ◦ Post heart attack: ACE inhibitor ◦ Angina: Beta blocker ◦ Congestive Heart failure: Beta blocker, ACE inhibitor, diuretic – thiazide, furosemide, spironolactone ◦ Left ventricular hypertrophy: ACE inhibitor ACE inhibitors/ ARB Pregnancy Hyperkalemia Beta Blockers Severe bradycardia, < 50 COPD Diuretics Gout Diastolic BP over 120mmHg with acute end organ damage Encephalopathy Papilledema Angina, heart attack Transient ischemic attack, stroke Acute renal failure Acute pulmonary edema Aortic dissection Admit to CCU, aim to lower BP to 160-180/100110 by 2 hours, may need IV meds Diastolic BP over 120 mmHg without acute end organ damage Admit and aim to lower BP to 160/100 over 24-48 hours. Note: Too rapid lowering of BP can cause ischemia to brain, heart, kidneys Use oral meds – diuretics, B Blockers, ACEI, Methyldopa DO NOT USE FAST ACTING NIFEDIPINE Hypertension, proteinuria, edema after 20wks BP 180/110 or greater x 2 Treatment: Give IV fluids, avoid diuretics IV hydralazine 5 mg over 5 mins, repeat in 20 mins. Aim: BP 140-160/90-100 Deliver as soon as possible! Hypertension may persist post delivery Use methyldopa Detect – take BP Identify and Stratify Risk Factors Treat according to risk/assoc. disease Follow Educate your patients about cardiovascular disease risks Make them partners in treatment