VIII Page 64
advertisement
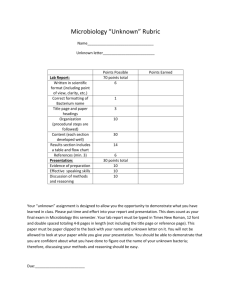
Texas Tech University Health Sciences Center Department of Pathology Resident Guidelines VIII Page 64 RE: Resident Responsibilities Revised June 21, 2010 NAME OF ROTATION: Microbiology and Immunology YEARS OF RESIDENCY ROTATION IS TAKEN AND DURATION: Year I-IV; minimum 6 months SITES: University Medical Center (UMC), Covenant Health Systems GOALS: Medical microbiology and immunopathology are combined into a multifaceted six-month program designed to prepare residents to successfully manage a clinical microbiology laboratory, function as a consultant for clinicians regarding infectious disease processes and their diagnoses, understand the entire scope of immunologic testing, manage a laboratory where immunologic testing is performed, and function as a consultant for clinicians regarding the proper use of these tests for patient care and diagnosis. Note that some immunopathology topics are discussed in the context of other rotations: HLA testing/tissue transplantation and immunohematology are covered during transfusion medicine rotations; flow cytometry/cellular immunology is covered during hematopathology rotations; immunoperoxidase techniques are covered during surgical pathology rotations. These topics, since they are taught in other rotations, are not discussed during these rotations. OBJECTIVES: I. SKILL LEVEL IA – RECOMMEND 2 MONTHS Goal: Develop everyday expertise in basic clinical laboratory skills as they apply to microbiology and immunology laboratories, including routine specimen collection, transport, and processing; gram stain methodology and importance; bacteriologic media; antimicrobial susceptibility testing; current immunologic testing methods; and introduction to the most common bacterial isolates encountered in clinical laboratories. A. Medical Knowledge: Demonstrate deep understanding of the following concepts based on suggested microbiology and immunology texts and didactic sessions with the responsible faculty: 1. Microbiology specimen collection, transport, and processing, gram staining, media 2. Immunologic testing methods 3. Antimicrobial susceptibility testing 4. Enteric gram-negative bacilli 5. Non-fermenting gram-negative bacilli 6. Gram-positive cocci 7. Haemophilus 8. Neisseria and Moraxella 9. Curved gram-negative bacilli Texas Tech University Health Sciences Center Department of Pathology Resident Guidelines VIII Page 65 RE: Resident Responsibilities Microbiology and Immunology Revised June 21, 2010 10. Miscellaneous fastidious gram-negative bacilli 11. Gram-positive bacilli 12. Immunoglobulin quantification 13. Complement assays 14. Delayed hypersensitivity skin testing, RIST and RAST assays B. Patient Care: Demonstrate proficiency in the following laboratory techniques following practical demonstration: 1. Specimen collection, transport, and processing (1 week) a. Proper plating of specimens on appropriate media with appropriate stains for specimens from the common sources b. Criteria and procedures for specimen rejection c. Proper incubation temperature and atmosphere d. Gram staining of clinical material e. Rapid testing for Group A Streptococci with appropriate follow-up f. Latex agglutination technique for bacterial antigen profile (CSF) 2. Rotate through primary plate reading benches (7 weeks) a. Distinguishing pathogenic from non-pathogenic bacteria b. Estimating bacterial load on cultures such as urine, sputum, and wounds c. Learning when to subculture isolates, and techniques for doing so d. Learning the time required to consider various types of cultures negative e. Performing rapid testing (catalase, bacitracin, optochin, CAMP, latex agglutination serotyping, bile esculin, 6.5% NaCl, oxidase, spot indole, urease, susceptibility screens, etc.) f. Use of the automated blood culture system, Isostat and Isolator specimens g. Identification and susceptibility testing using the Microscan, microtiter broth dilution, disc diffusion (Kirby-Bauer) testing, E-test C. Systems based practice: Interface with other services within the hospital and understand federal regulations as they apply to the microbiology and immunology laboratory. These experiences should continue throughout the remainder of the residents’ microbiology rotations: 1. Use of the laboratory computer system for order entry, data retrieval 2. Attendance of UMC and/or TTUHSC Infection Control committee meetings 3. Review of proper safety requirements (OSHA) 4. Understanding of basic concepts of laboratory medicine regulations as they apply to microbiology and immunology (CLIA, CAP, CMS, HIPAA): proficiency testing, QC, quality management, personnel qualifications, coding, procedures & policies, confidentiality, etc. Texas Tech University Health Sciences Center Department of Pathology Resident Guidelines VIII Page 66 RE: Resident Responsibilities Microbiology and Immunology Revised June 21, 2010 D. Interpersonal/communication skills: Interpersonal communication is of prime importance in clinical pathology, and residents must show proficiency in interpersonal communication with the following members of the health care team: 1. Medical technologists and medical laboratory technicians 2. Laboratory supervisors 3. Attending pathologists 4. Clinical residents and/or attendings from whom consultations are requested II. SKILL LEVEL 1B – RECOMMEND 2 MONTHS: Goal: Continue to utilize skills previously learned as they apply to more complicated/less commonly encountered organisms and test requests. A. Medical Knowledge: Areas which the resident must show competency are as follows: 1. Anaerobic bacteria 2. Mycobacteria 3. Antinuclear antibodies 4. Extractable nuclear antigens 5. Rheumatoid factor assays 6. Spirochetes 7. Mycoplasmas 8. Obligate intracellular bacteria (Chlamydia, Rickettsia, etc.) B. Patient Care: Continue practical bench side experience in the laboratory to include the following 1. Anaerobes a. Differentiation of true (obligate) anaerobes from facultative bacteria b. Differentiation of pathogenic anaerobes from non-pathogens c. Determination of the amount and type of work-up to be done on isolates d. Interpretation of tests for identification of anaerobes 2. Mycobacteriology laboratory (Covenant Medical Center) a. Safety precautions for working with acid-fast organisms b. Specimen processing, including concentration, digestion, decontamination, and plating c. Smear staining by acid fast and fluorochrome stains d. Special procedures for detecting AFB in blood e. Identification and susceptibility testing of AFB 3. Chlamydia, mycoplasma, rickettsia a. Direct examination for organisms b. Interpretation of cultures c. “Febrile agglutinins” Texas Tech University Health Sciences Center Department of Pathology Resident Guidelines VIII Page 67 RE: Resident Responsibilities Microbiology and Immunology Revised June 21, 2010 4. C. III. Cold agglutinins Immunology laboratory a. Performance of ANA by indirect immunofluorescence and interpretation of fluorescent patterns b. Extractable nuclear antigens using Crithidia assay c. Rheumatoid factor assays d. RPR Systems based practice: At this point residents should be conversant enough with laboratory medicine to be a hands-on consultant with clinical infectious disease teams and will be expected to attend clinical rounds with such teams as often as feasible. These sessions should be mutually beneficial, the pathology resident able to update the clinical team and answer their questions, and the clinical team able to fill in clinical information that might otherwise be lacking in the pathology curriculum. These experiences should continue throughout the remainder of the residents’ microbiology rotations. SKILL LEVEL IIA: RECOMMEND 1 MONTH: Goal: Continue resident education in microbiology, now focusing attention to the diagnosis of fungal infections. A. B. Medical Knowledge: Areas to be studied and discussed with microbiology faculty include: 1. Fungal specimen collection, transport, and processing. 2. Zygomycetes 3. Dermatophytes 4. Hyaline molds 5. Dematiaceous fungi 6. Dimorphic fungi 7. Yeasts 8. Unusual fungal and algal pathogens Patient Care: Demonstrate proficiency in the following areas of diagnostic mycology: 1. Plating and staining of specimens 2. Direct examination for fungi 3. Preparation and interpretation of wet mounts from cultures using lactophenol cotton blue stain 4. Identification of yeasts using germ tube test, cornmeal agar morphology, and biochemical testing 5. Latex agglutination assay for cryptococcal antigen (CSF) 6. Detection and identification of dimorphic fungi 7. Detection and identification of dermatophytes Texas Tech University Health Sciences Center Department of Pathology Resident Guidelines VIII Page 68 RE: Resident Responsibilities Microbiology and Immunology Revised June 21, 2010 IV. V. SKILL LEVEL IIB: RECOMMEND 1 MONTH: Goal: Continue resident education in the much more complicated area of virology and finish up immunology with autoantibodies directed against cytoplasmic antigens. A. Medical Knowledge: Demonstrate deep understanding of the clinical aspects and laboratory diagnosis of the following concepts: 1. Clinically significant virus families 2. Anti-parietal cell and –intrinsic factor antibodies 3. Anti-smooth muscle and –mitochondrial antibodies 4. Thyroid autoantibodies 5. Anti-neutrophilic cytoplasmic antibodies 6. Anti-adrenocortical antibodies B. Patient Care: Demonstrate proficiency in the following laboratory techniques: 1. Performance and interpretation of rapid testing for viral antigens. 2. Performance and interpretation of virus serology. 3. Reading and interpretation of viral cultures including confirmation of culture results. 4. Use of indirect immunofluorescence to detect anti-smooth muscle, antiparietal cell, and anti-mitochondrial antibodies. SKILL LEVEL IIC: RECOMMEND 1 MONTH Goal: Continue resident training in microbiology, now focusing on diagnostic parasitology. A. B. Medical Knowledge: Demonstrate deep understanding of the clinical significance and diagnosis of human parasites. 1. Protozoal parasites. 2. Trematodes. 3. Cestodes. 4. Nematodes. 5. Ectoparasites. Patient Care: Demonstrate proficiency in the following areas of diagnostic parasitology: 1. Interpretation of saline and iodine direct mounts. 2. Interpretation of special stains (trichrome, acid fast, etc.). 3. Identification of ova and parasites by microscopic examination. 4. Identification of parasites in histologic sections. 5. Identification and speciation of parasites in peripheral blood smears. 6. Identification of clinically significant arthropods. Texas Tech University Health Sciences Center Department of Pathology Resident Guidelines VIII Page 69 RE: Resident Responsibilities Microbiology and Immunology Revised June 21, 2010 DUTIES AND RESPONSIBILITIES OF RESIDENTS: I. II. III. IV. Residents will meet with the responsible pathology faculty several times a week for discussion of topics in microbiology and immunopathology as described above. The residents will receive a more specific, comprehensive schedule of discussion topics at the beginning of each rotation, and are expected to read about each topic prior to meeting with the faculty. Residents will gain practical experience by working alongside the technologists in the microbiology and immunology laboratories as described above. Residents will accompany the attending pathologist to UMC and TTUHSC Infection Control Committee meetings and participate in all consultations by clinicians pertaining to microbiology or immunologic testing. Residents will periodically make patient rounds with the Infectious Disease specialists of Internal Medicine and Pediatrics departments from the third rotation onward. Pathology residents will not be expected to round on these patients alone or write progress notes, but simply accompany these teams when they round and gain clinical insight into infectious disease processes and their treatment. TEACHING STAFF RESPONSIBLE FOR SUPERVISION: Jane Colmer-Hamood, Ph.D. – rotations 1-5 Afzal Siddiqui, Ph.D. – rotation 6 SUPERVISION AND EVALUATION: Residents’ performance and progress will be evaluated at the end of each rotation. These evaluations will be written, and will be discussed with the individual residents. These evaluations will be based on performance during didactic sessions, presentations, laboratory bench work, and proper identification of unknown slides/specimens. The latter will be given on a weekly schedule. SUGGESTED TEXTBOOKS: Color Atlas and Textbook of Diagnostic Microbiology, 5th ed. by Koneman et al. Bailey & Scott’s Diagnostic Microbiology, 11th ed. by Forbes et al. Manual of Clinical Microbiology, 8th ed. by Murray et al. Medically Important Fungi: A Guide to Identification, 4th ed. by Larone. Markell and Voge’s Medical Parasitology, 8th ed. by Markell et al. Atlas of Human Parasitology, 4th ed. by Ash & Orihel Parasites in Human Tissues by Orihel & Ash Manual of Clinical Laboratory Immunology, 6th ed. by Rose et al.