Integumentary System BIOL241 INTERCONNECTEDNESS
advertisement

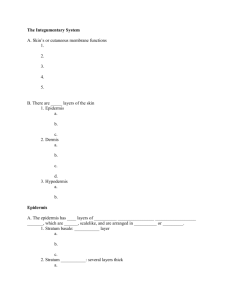
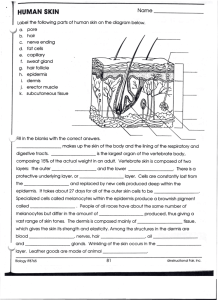
Integumentary System BIOL241 INTERCONNECTEDNESS Outline • Structure and function of integument – Epidermis – Dermis – Hypodermis • • • • • • Skin color Skin cancer Accessory structures of Integument Temperature regulation Aging Skin Injury and regeneration Integumentary System (skin) Skin (Integument) • Consists of three major regions – Epidermis – outermost superficial region – Dermis – middle region these two together make up the cutaneous membrane) – Subcutaneous region (aka Hypodermis or (superficial fascia) – deepest region • Also includes all the accessory structures found in the skin (hair, glands, etc.) What are some of the functions of skin? • • • • • • Protection Excretion (salts, water, wastes) Maintenance of body temperature Metabolism (Vitamin D3) Storage (lipids, blood reserve) Detection of sensation • Note: skin keeps water in as well as keeping it out Hair shaft Pore Dermal papillae (papillary layer of dermis) Epidermis Meissner's corpuscle Free nerve ending Reticular layer of dermis Sebaceous (oil) gland Arrector pili muscle Dermis Sensory nerve fiber Eccrine sweat gland Pacinian corpuscle Artery Hypodermis (superficial fascia) Vein Hair root Hair follicle Eccrine sweat gland Adipose tissue Hair follicle receptor (root hair plexus) Figure 5.1 Parts of the Cutaneous Membrane • Outer epidermis: – superficial epithelium (epithelial tissues) Composed of keratinized stratified squamous epithelium, consisting of four distinct cell types and four or five layers – Cell types include keratinocytes, melanocytes, Merkel cells, and Langerhans’ cells – Outer portion of the skin is exposed to the external environment and functions in protection • Inner dermis: – connective tissues (what are they?) Epidermis • Avascular stratified squamous epithelium • Nutrients and oxygen diffuse from capillaries in the dermis to lower layers of epidermis Cells of the Epidermis • Keratinocytes – produce the fibrous protein keratin • Melanocytes – produce the brown pigment melanin; cell bodies in upper dermis that have extensions into the epidermis • Langerhans’ cells – epidermal macrophages that help activate the immune system • Merkel cells – function as touch receptors in association with sensory nerve endings Organization of the Epidermis: Figure 5–2 Layers of the Epidermis Figure 5.2b The thick of it Thin Skin • Covers most of the body • Has 4 layers of keratinocytes Thick skin • Covers the palms of the hands and soles of the feet • Has 5 layers of keratinocytes Layers of the epidermis are known as “strata” Layers of the Epidermis Top: Free surface of skin - stratum corneum - stratum lucidum - stratum granulosum - stratum spinosum - stratum germinativum Bottom: Basal lamina 1. Stratum Germinativum (Basale) • The “germinative layer” (or basal layer): – Deepest epidermal layer firmly attached to the basal lamina and dermis via hemidesmosomes – Consists of a single row of the youngest keratinocytes along with projections of melanocytes – Cells undergo rapid division, Structures of Stratum Germinativum • Epidermal ridges – – cause the pattern of your fingerprints; – created by presence of: • Dermal papillae (tiny mounds): – increase the area of basal lamina – Function? Fingerprints are epidermal ridges • Which themselves are negative images of the dermal papilla Figure 5–4 2. Stratum Spinosum • “spiny layer” • 8-10 cells (keratinocytes) thick • Immature keratinocyte cells continue to divide, then shrink until cytoskeletons stick out (spiny), a system of intermediate filaments attached to desmosomes • Melanin granules and Langerhans’ cells are abundant in this layer 3. Stratum Granulosum • “grainy layer” • Consists of 3-5 cell layers of keratinocytes • Cells stop dividing in this layer, dehydrate and produce tons of proteins: – Keratohyaline – Keratin 4. Stratum Lucidum • • • • The “clear” layer Only found in thick skin Covers granulosum Consists of a few rows of flat, dead keratinocytes filled with keratin • The layer appears, ironically, very thin in slides • Probably functions to hold on the thicker corneum layer above A note on thick vs. thin skin • Thick skin has an extra layer (lucidum) but that is NOT the reason that it is thicker than thin skin. • The reason is the other layers are thicker in thick skin than in thin skin, esp. s. corneum 5. Stratum Corneum • • • • • • • The “horn layer”: exposed surface of skin 15 to 30 layers of keratinized cells Accounts for ¾ of epidermal thickness water resistant (not water proof!) Protects from abrasion and penetration shed and replaced every 2 - 4 weeks Skin is often called a cornified epithelium Skin Life Cycle • It takes 15–30 days for a cell to move from stratum germinosum to stratum corneum Layers of the Epidermis Figure 5.2b Dermis consists of connective tissue The Dermis • Deeper part of cutaneous layer • Located between epidermis and subcutaneous layer • Anchors epidermal accessory structures (hair follicles, sweat glands) • Contains strong, flexible connective tissue • Cell types include fibroblasts, macrophages, and occasionally mast cells and white blood cells • Has 2 components: – outer papillary layer – deep reticular layer The Papillary Layer • Consists of areolar tissue with collagen and elastic fibers • Contains smaller capillaries, lymphatic vessels, and sensory neurons • Has dermal papillae projecting between epidermal ridges The Reticular Layer • Consists of dense irregular connective tissue • Accounts for approximately 80% of the thickness of the skin • Contains larger blood vessels, lymph vessels, and nerve fibers • Collagen fibers in this layer add strength and resiliency to the skin • Elastin fibers provide stretch-recoil properties Contains collagen and elastic fibers The Subcutaneous Layer • Subcutaneous layer (superficial fascia or hypodermis): – loose connective tissue - areolar and adipose – connected to the reticular layer of dermis by connective tissue fibers – stabilizes the skin – allows separate movement – Insulates and stores energy – location of hypodermic injections Skin Color • Skin color depends on three pigments: – Melanin -yellow to reddish-brown to black pigment, responsible for dark skin colors • Freckles and pigmented moles – result from local accumulations of melanin • Produced by melanocytes just below stratum germinativum • Stored in transport vesicles (melanosomes) • Projections extend up into epidermal layers • Some transferred to keratinocytes – Hemoglobin in red blood cells – Carotene (minor factor) Melanocytes Figure 5–5 Function of Melanocytes • Ultraviolet (UV) radiation: – causes DNA mutations and burns which lead to cancer and wrinkles • Melanin protects skin from sun damage • Pigment molecules absorb UV and diffuse it, preventing it from penetrating to the DNA of cells in the strata germinativum and spinosum Melanocytes • Skin color depends on amount of melanin production per melanocyte, not number of melanocytes. Capillaries and Skin Color • Oxygenated red blood contributes to skin color: – blood vessels dilate from heat, skin reddens – blood flow decreases, skin pales – corpses appear pale and lighter because they lack this coloration Cyanosis • Bluish skin tint • Caused by severe reduction in blood flow or oxygenation • The veins appear blue when blood is deoxygenated but deoxegenated blood is NOT blue – it is darker red Illness and Skin Color • Jaundice: – buildup of bile produced by liver – yellow color • Addison’s disease: – and other diseases of pituitary gland – skin darkening • Vitiglio: – loss of melanocytes – localized loss of color Vitamin D • The “sunshine vitamin” • Epidermal cells produce cholecalciferol (vitamin D3) in the presence of UV radiation • Liver and kidneys convert vitamin D into calcitriol which aids in absorption of calcium and phosphorus at the intestines • Insufficient vitamin D: – can cause rickets – Symptoms? Skin Damage • Sagging and wrinkles (reduced skin elasticity) are caused by loss (or decresed production) of collagen and elastin by fibrolasts, due to: – dehydration – age – hormonal changes – UV exposure Skin Cancer Figure 5–6 Skin Cancer • The three major types of skin cancer are: – Basal cell carcinoma (s. germinativum) – Squamous cell carcinoma (s. spinosum) – Melanoma • The vast majority of all skin cancers are of the first two types (basal and squamous) • They rarely metastasize and can be taken care of by excision; thus they are not included in most cancer statistics Melanoma • Cancer of melanocytes is the most dangerous type of skin cancer because it is: – Highly metastatic – Resistant to chemotherapy • Kind of ironic because they evolved to protect basal cells, but basal cell cancer has a much better prognosis Skin Cancers Figure 5.7a–c Skin color tradeoff? • Vitamin D is necessary for bone strength, but if there is not much UV (high latitudes), individuals with a lot of melanin have trouble getting enough Vitamin D. But when UV is plentiful, they are better protected from skin cancer. • On the other hand, in places with a lot of UV (low latitudes), people with very little melanin are at high risk of skin cancer. But they are more likely to get enough UV from the sun in low UV regions. Use Protection! Accessory Structures of the Integument • Are of epidermal lineage (cells are modified epithelial cells) • “Originate” in the dermis (this is where you look to find them) • Extend through the epidermis to skin surface: – Hair ad follicles – nails – multicellular exocrine glands (sebaceous, sweat) The Hair Follicle • • • • Is located deep in dermis Is made of epidermal tissue Produces nonliving hairs Is wrapped in a dense connective-tissue sheath • Base is surrounded by sensory nerves Structures of Hair and Follicles Figure 5–9a Structures of Hair • Arrector pili: – involuntary smooth muscle – causes hairs to stand up – produces “goose bumps” • Sebaceous glands: – lubricate the hair – control bacteria Properties of hair • As hair is produced, it is keratinized: – middle medulla contains flexible soft keratin – outer cortex and cuticle contain stiff hard keratin • Hair Color – Produced by melanocytes at the hair papilla (base) – Determined by genes Sebaceous glands and follicles (oil glands): • Holocrine exocrine glands that secrete waxy, oil secretion called sebum – Lubricates and protects the hair and skin epidermis – Inhibits bacterial growth • Sebaceous glands: – associated with most hair follicles (on head and body) • Sebaceous follicles: – discharge directly onto skin surface – found on face and trunk only – when clogged acne Sebaceous glands and follicles Types of Sweat Glands • Merocrine (eccrine) sweat glands: – more numerous, widely distributed on body surface, especially on palms and soles (thick skin) – Produce thin sweat for evaporative cooling • Apocrine sweat glands: – found in armpits, around nipples, and anogential areas – produce thick sweat Both are actually merocrine “Apocrine” Sweat Glands • Merocrine secretions, not apocrine • Associated with and discharge into hair follicles in groin, nipples, and axillae (armpits) • Become active at puberty • Produce sticky, cloudy secretions (thick sweat) that breaks down, feeds bacteria and causes odor: pungent, not for cooling Merocrine Sweat Glands • Also called eccrine glands: – discharge directly onto skin surface – produce thin sweat – contains water, salts, and organic compounds • Thin sweat functions – sensible perspiration for evaporative cooling – excretes water and electrolytes – flushes microorganisms and harmful chemicals from skin Sweat Glands of the Skin Merocrine Apocrine Other Integumentary Glands Specialized sweat glands: • Mammary glands: – produce milk • Ceruminous glands: – protect the eardrum – produce cerumen (earwax) Control of Glands • Autonomic nervous system: – controls sebaceous and apocrine sweat glands – works simultaneously over entire body • Merocrine sweat glands: – are controlled independently – sweating occurs locally (e.g. you can sweat on just one palm) Temperature Regulation: Dermal Circulation Figure 5–8 Dermal circulation • Arteries – Cutaneous plexus: a network of arteries along the bottom of the reticular layer – Papillary plexus: capillary network from small arteries in papillary layer • proximate source of nutrients for epidermal cells • Cells in the s. corneum are too far away to be nourished through difusion – that’s why they are dead • Venous plexus: – capillary return deep to the papillary plexus – Bruises usually occur from breakage of these vessels Temperature Regulation: Perspiration • Sensible perspiration: – Water excreted by merocrine sweat glands – Cools skin evaporatively • Insensible perspiration: – Interstitial fluid lost by evaporation through the stratum corneum – Not so important in cooling but a very important source of water loss Water Loss Through Skin • Dehydration results: – from damage to stratum corneum, e.g., burns and blisters (insensible perspiration) – from immersion in hypertonic solution, e.g., seawater (osmosis) Nerves • Nerve fibers in the skin control: – blood flow through the dermis – gland secretions – sensory receptor (Merkel cells, Meissner’s corpuscles) Temperature Regulation: Homeostasis • Skin plays a major role in controlling body temperature (thermoregulation): • Body temperature regulation is accomplished by dilation (cooling) and constriction (warming) of dermal vessels – Dilation allows skin to act as a radiator, removes heat from dermal circulation (radiates heat through skin to environment); constriction helps retain heat – evaporation of sensible perspiration improves heat removal by Dermal circulation is the most important factor in body cooling. Sweat makes this cooling more efficient. Skin: Effects of Aging • • • • • • • • • • • Decreased numbers of immune cells Decreased vitamin D3 production Decreased melanocyte activity Decreased function of hair follicles Slower repair rate Reduction of elastic fibers (wrinkles) Skin becomes dry and itchy Subcutaneous fat layer diminishes (cold intolerance) Decreased glandular activity (sweat and oil glands) Epidermal and dermal thinning Reduced dermal blood supply Aging and thermoregulation (or “why grandma is always cold”) 1. Epidermis thins, subcutaneous fat decreases, heat escapes more easily 2. Blood supply to dermis is reduced – Causes skin to become cooler – Stimulates thermoreceptors in skin which signal “coldness,” even in a warm environment However, there is danger of overheating because: – reduced merocrine sweat gland activity and reduced dermal circulation both lessen ability to lower body temperature effectively Repair of Localized Injuries to the Skin: Step 1 • Bleeding occurs • Mast cells trigger inflammatory response Figure 5–13 (Step 1) Repair of Localized Injuries to the Skin: Step 2 • A scab stabilizes and protects the area Figure 5–13 (Step 2) The Inflammatory Response • Germinative cells migrate around the wound • Macrophages clean the area • Fibroblasts and endothelial cells move in, producing granulation tissue Repair of Localized Injuries to the Skin: Step 3 • Fibroblasts produce scar tissue • Inflammation decreases, clot disintegrates Figure 5–13 (Step 3) Repair of Localized Injuries to the Skin: Step 4 • Fibroblasts strengthen scar tissue • A raised keloid forms Figure 5–13 (Step 4) Summary • Structure and function of integument – Epidermis – Dermis – Hypodermis • • • • • • Skin color Skin cancer and other diseases Accessory structures of Integument Temperature regulation Aging Skin Injury and regeneration