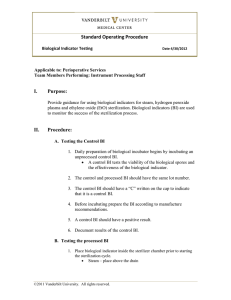
Equipment Washers and Sterilizers 2016-01-02 rev 1 do not print it to pdf
advertisement

Equipment Washers and Sterilizers 2016-01-02 rev this is now slide 1 do not print it to pdf things to do (check off when complete): x add revision date to cover page x remove triangles x create list for pages to print in the handout 2-11,15,17-18,28,31-33,37,39-40,44,47,54,57-66,69-74 add captions for photo slides incorporate notes taken during presentation Equipment Washers and Sterilizers Joseph Lister © D. J. McMahon 150104 rev cewood 2016-01-02 Definitions - Antiseptic: germicide for use on living tissue - Antibiotics or antibacterials: a type of antimicrobial used in the treatment and prevention of bacterial infection. They may either kill or inhibit the growth of bacteria - Cleaning: removal of foreign material, using disinfectant and friction - Disinfection: process that only kills vegetative bacteria ( Can be low, intermediate, and high levels ) - Decontamination: process that renders a surface safe to handle but not totally free of microorganisms - Sterilization: any process that renders a surface completely free of microorganisms - Pasteurization: High-level disinfection (HLD) by the use of moderate heat (71-76° C) for ~30 minutes Sterilization: Sterility occurs when all microorganisms are killed by breaking open the capsule or wall of the organism. We can do this with heat, chemicals, or various types of radiation. Methods of Sterilization: Live Steam: the ‘gold standard’ > basic exposure is steam at 121°C (250°F) and 15psi for 15 minutes (note: > 14.7 psi) > heat and time duration vary depending on the type and volume of material being processed > biological “controls” are used to verify that sterilization occurred > Autoclave: Any system that sterilizes instruments or packs by means of wet heat under pressure. Methods of Sterilization: Chemical Methods - Ethylene oxide (EtO) gas > exposure in a closed chamber > kills almost all microorganisms > toxic and carcinogenic - Cidex™ (glutaraldehyde) > liquid solution of 1% glutaraldehyde > used mostly for instruments or (rigid) scopes > technically a disinfectant only Methods of Sterilization: Chemical Methods continued - - Peracetic Acid > powder diluted in hot water > used in Steris’ “System 1” > used primarily for endoscopes - Peroxide in Plasma > exposure to hydrogen peroxide in a chamber with an electric field > “Sterrad” system by ASP > esp. good for fragile, plastic items > substitute for EtO Methods of Sterilization: Ionizing Energy Methods Used for bulk quantities in manufacturing - Electron Beam > created by e-beam generators > low penetration, high dose - Gamma Ray > emitted from Cobalt-60 source > better for larger, denser items Olympic (Natus) Pasteurmatic System -- Pasteurmatic cycles: Bulk sterilization by gamma radiation -- Washers: > Not sterilizers > Automated washing systems for decontaminating large volumes of trays of surgical instruments > Usually found in Central Services > Often in a ‘pass-through’ wall to the “clean side” of the CS Dept, where instrument trays and sets are reassembled before sterilization CDC and FDA agree on the “Spaulding Classification” for processing devices: Critical devices: enter a surgical field or the vascular system - these require sterilization Semicritical devices: contact mucous membranes, do not break tissue - should be at least high-level disinfected if not sterilized Noncritical devices: touch only intact skin - can be cleaned by low-level disinfection ANSI/AAMI ST79 – Recommended Practice for Hospital Steam Sterilization Primary reference for autoclave users Expiration Dates for sterile packages are now “Event-Related” (vs “Time-Related”): A properly sterilized package can be considered sterile indefinitely as long as it is not torn, does not become wet or damaged and is not suspected of being compromised. All packages are dated for date of sterilization, and the package with the earliest date is always picked. When The Joint Commission inspects a facility, they want to see a policy for management of sterile supplies, and consistent compliance with that policy. Maintenance & Repair of Autoclaves – Service schools are provided by major autoclave makers Get the book out before opening-up any autoclave Many hospitals outsource autoclave maintenance to ISO’s - eg Seattle Surgical or Omega Mechtronics Typical city or state “boiler inspection” regulations require autoclaves to be inspected every 2 years by the city or county inspectors. - includes checks of safety valves, overall condition, documentation. In order to work effectively, steam autoclaves must first force all air out of the chamber. Most are the “gravity fill” type: steam enters at the top of the chamber and displaces all the air. Other methods use an evacuation pump. Table-top autoclaves - Maintenance of Tabletops – Major players in large autoclaves: - Steris (was Amsco) - Getinge-Castle - Vernitron Major players in table-tops: - Midmark-Ritter - Pelton & Crane - Tuttnauer Third party parts provider for autoclaves and related equipment: Replacement Parts, Inc (RPI) www.rpiparts.com Chemical Sterilization: Sterilization by gluteraldehyde – “Cold” sterilization Usually sold as Cidex™ 1% solution Immersion for ~30 minutes, and thorough rinsing Cidex is toxic and used in limited amounts Best for ‘lensed’ instruments and flexible scopes EvoTech scope washer from ASP - uses Cidex™ Chemical Sterilization: Sterilization by Peracetic Acid: Endoscope washer/sterilizers Automated systems that sterilize fiberoptic scopes, cameras, or ultrasound probes in chemical sterilants (usually peracetic acid). Include a way to expose all internal lumens (which can be .5mm) and recessed areas to the sterilant solution to assure that all microorganisms are killed. Olympus MD-2 system - Steris System-1 (now System-1E) Specifically for endoscopic scopes Exposes items to peracetic acid solution Entire cycle ~40 minutes Can be high-maintenance: requires very hot water supply, several high-level filters, and will shut down under many conditions Has been redesigned (2012) by Steris per the FDA Steris System 1e - replaced System1 System 1e requires highly filtered hot water - Chemical Sterilization: Sterilization by Peroxide Plasma Sterrad™ sterilization system – >> Proprietary to ASP Corp >> Exposes items to hydrogen peroxide (H2O2) in an electrical field >> Entire cycle ~ 45 minutes >> Good for small, fragile, heat-sensitive items Table-top Sterrad model NX - Chemical Sterilization: Sterilization by Ethylene Oxide – (‘EtO’ or ‘EO’) EtO gas is mixed with an inert gas in a chamber Kills all microorganisms chemically Used for the majority of bulk-sterilized disposables Toxic to liver, causes cataracts Used in fewer hospitals today Chemical Sterilization: Sterilization by Ozone – > Kills microorganisms by exposure to ozone (O3) > Needs only oxygen, water, & electrical power > Cycle time ~5 hours > Limited range of items that can be processed TSO3 Corp, model 125L ozone sterilizer - Uses the oxidizing properties of ozone (O3) to kill microorganisms. Limited market success. Verifying sterility Bowie-Dick Test – (ANSI/AAMI ST66) Pack of special papers subjected to a cycle in a steam autoclave, to detect any remaining pockets of air that were not evacuated. Black symmetrical patterns will be uneven or discolored if air is present. Not a biological performance test - serves only to warn of inadequate air removal. Bowie-Dick Test; 3M “Comply” Test Pack Chemical controls – (before exposure) Change color when exposed to sterilizing conditions steam Sterrad steam EtO ozone Biological controls – Verification that a sterilizer is effective Live bacteria that are difficult to kill are added to the sterilizer load, and checked to be sure that they are killed-off. All sterilizer controls are documented. Biological controls – 3M Attest Biological Indicator (BI) goes through steam sterilization cycle with the items being sterilized. (Other BIs are available for other sterilization processes, including Ethylene Oxide EO) BI is incubated for 24-48 hours. (“Super Rapid” system for steam sterilization requires just one hour of incubation.) Each BI contains > 1,000,000 living spores of a highly resistant organism. If the spores are inactivated or killed by the sterilization cycle, you have a direct measure of an effective sterilization process. “Super Rapid” G.I. Endoscopy -- Upper G.I. Lower G.I. Typical endoscopy scenarios - Processing of endoscopes: - #1 in ECRI’s Top Ten Hazards for 2016 - flexible fiberoptic scopes - endoscopic cameras - rigid scopes & instruments Most automated endoscope reprocessors achieve high-level disinfection, but the trend is to full sterilization. - Steris ‘System 1e’ achieves sterilization with peracetic acid The Sterrad (peroxide-plasma) can be used for limited scope types, with only one channel. EtO is generally not used due to long process times. Scope washers in a G.I. endoscopy clinic Typical endoscope washers in a G.I. clinic: autoclaves of the past: