Figure 1. Mortality Amenable to Health Care Deaths per 100,000 population* International
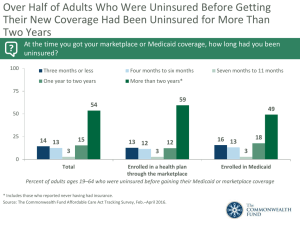
advertisement

Figure 1. Mortality Amenable to Health Care Mortality from causes considered amenable to health care is deaths before age 75 that are potentially preventable with timely and appropriate medical care Deaths per 100,000 population* International variation, 1998 150 100 75 92 88 88 88 84 81 97 97 99 106 107 109 109 State variation, 134 2002 129 130 132 115 115 119 110 103 84 90 50 Fr an ce Ja pa n Sp a Sw in ed en I Au ta ly st ra Ca l ia na N da Ne or th wa y er la nd s G re G ece er m an y Ne Au s w t Ze ria al De an d Un n ite m a rk d St at es Fi nl an Un ite Ire d l d Ki and ng d Po o m rtu ga l 0 U.S. avg 10th 25th Med- 75th ian Percentiles * Countries’ age-standardized death rates, ages 0–74; includes ischemic heart disease. See Technical Appendix for list of conditions considered amenable to health care in the analysis. Data: International estimates—World Health Organization, WHO mortality database (Nolte and McKee 2003); State estimates—K. Hempstead, Rutgers University using Nolte and McKee methodology. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 90th Figure 2. Infant Mortality Rate, 2002 Infant deaths per 1,000 live births International variation State variation 10 9.1 8.1 7.0 7.1 7.0 6.0 5.4 5.6 5.2 5.1 5.0 5.0 5.0 5.0 5 5.3 4.4 4.4 4.5 4.5 4.1 4.1 4.1 4.2 4.2 3.0 3.0 3.3 3.5 2.2 Ic el a nd Ja pa Fi n nl an Sw d ed e No n rw ay Sp ai Fr n an ce Cz A ec us h Re tria pu b Ge lic rm a Be ny lg i De um nm ar k Sw Ita ly itz Ne erla nd th er la n Au ds st ra Po lia rtu ga Ire l la nd Un G ite re d ec Ki ng e do m C an Ne a w da Z Un eal ite and d St * at es 0 U.S. avg * 2001. Data: International estimates—OECD Health Data 2005; State estimates—National Vital Statistics System, Linked Birth and Infant Death Data (AHRQ 2005a). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 10th 25th Median 75th Percentiles 90th Figure 3. Uninsured Rates High Among Adults with Low and Moderate Incomes, 2001–2005 Percent of adults ages 19–64 75 Insured now, time uninsured in past year Uninsured now 49 50 16 25 28 24 26 9 9 9 52 53 15 16 28 33 37 37 15 17 18 0 35 11 41 13 11 17 24 28 13 7 6 16 18 9 9 7 9 4 3 4 2 7 3 2001 2003 2005 2001 2003 2005 2001 2003 2005 2001 2003 2005 2001 2003 2005 Total Low income Moderate income Middle income High income Note: Income refers to annual income. In 2001 and 2003, low income is <$20,000, moderate income is $20,000– $34,999, middle income is $35,000–$59,999, and high income is $60,000 or more. In 2005, low income is <$20,000, moderate income is $20,000–$39,999, middle income is $40,000–$59,999, and high income is $60,000 or more. Source: S.R. Collins et al., Gaps in Health Insurance Coverage: An All-American Problem, Findings from the Commonwealth Fund Biennial Health Insurance Survey, The Commonwealth Fund, April 2006. Figure 4. Adults Ages 19–64 Who Are Uninsured and Underinsured, by Poverty Status, 2003 Insured, not underinsured Underinsured* Uninsured during year 100% 26 80% 13 4 49 9 60% 83 40% 19 65 20% 32 0% Total 200% of poverty or more Under 200% of poverty * Underinsured defined as insured all year but experienced one of the following: medical expenses equaled 10% or more of income; medical expenses equaled 5% or more of incomes if low-income (<200% of poverty); or deductibles equaled 5% or more of income. Data: 2003 Commonwealth Fund Biennial Health Insurance Survey (Schoen et al. 2005b). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. Figure 5. Access Problems Because of Costs in Five Countries, Total and by Income, 2004 Percent of adults who had any of three access problems* in past year because of costs 80 Below average income Above average income 57 44 40 40 35 34 29 29 26 24 25 17 12 9 12 6 0 UK CAN AUS NZ US UK CAN * Did not get medical care because of cost of doctor’s visit, skipped medical test, treatment, or follow-up because of cost, or did not fill Rx or skipped doses because of cost. UK=United Kingdom; CAN=Canada; AUS=Australia; NZ=New Zealand; US=United States. Data: 2004 Commonwealth Fund International Health Policy Survey of Adults’ Experiences with Primary Care (Schoen et al. 2004; Huynh et al. 2006). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. AUS NZ US Figure 6. Receipt of All Three Recommended Services for Diabetics, by Race/Ethnicity, Family Income, Insurance, and Residence, 2002 Percent of diabetics (ages 18+) who received HbA1c test, retinal exam, and foot exam in past year Total 53 55 White 54 Black 38 Hispanic 61 400% + of poverty 200% –399% of poverty 50 100% –199% of poverty 47 46 <100% of poverty Private* 54 24 Uninsured Urban** 55 45 Rural 0 50 * Insurance for people ages 18–64. ** Urban refers to metropolitan area >1 million inhabitants; Rural refers to noncore area <10,000 inhabitants. Data: 2002 Medical Expenditure Panel Survey (AHRQ 2005a). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 100 Figure 7. Adults Without Insurance Are Less Likely to Be Able to Manage Chronic Conditions Percent of adults ages 19–64 with at least one chronic condition* Insured all year Insured now, time uninsured in past year Uninsured now 75 58 59 50 27 25 18 35 16 0 Skipped doses or did not fill Visited ER, hospital, or both for chronic prescription for chronic condition condition because of cost *Hypertension, high blood pressure, or stroke; heart attack or heart disease; diabetes; asthma, emphysema, or lung disease. Source: S. R. Collins, K. Davis, M. M. Doty, J. L. Kriss, A. L. Holmgren, Gaps in Health Insurance: An All-American Problem, Findings from the Commonwealth Fund Biennial Health Insurance Survey (New York: The Commonwealth Fund, Apr. 2006). Figure 8. Receipt of Recommended Screening and Preventive Care for Adults, by Family Income and Insurance Status, 2002 Percent of adults (ages 18+) who received all recommended screening and preventive care within a specific time frame given their age and sex* National 49 400%+ of poverty 56 200%–399% of poverty 48 <200% of poverty 39 Insured all year 52 Uninsured part year 46 Uninsured all year 31 0 50 * Recommended care includes seven key screening and preventive services: blood pressure, cholesterol, Pap, mammogram, fecal occult blood test or sigmoidoscopy/colonoscopy, and flu shot. Data: B. Mahato, Columbia University analysis of 2002 Medical Expenditure Panel Survey. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 100 Figure 9. Preventive Care Visits for Children, by Top and Bottom States, Race/Ethnicity, Family Income, and Insurance, 2003 Percent of children (ages <18) received BOTH a medical and dental preventive care visit in past year 59 U.S. average 73 Top 10% states 48 Bottom 10% states 62 White 58 Black 49 Hispanic 70 400% + of poverty 48 <100% of poverty 63 Private insurance 35 Uninsured 0 50 Data: 2003 National Survey of Children’s Health (HRSA 2005; retrieved from Data Resource Center for Child and Adolescent Health database at http://www.nschdata.org). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 100 Figure 10. Children with a Medical Home, by Top and Bottom States, Race/Ethnicity, Family Income, and Insurance, 2003 Percent of children who have a personal doctor or nurse and receive care that is accessible, comprehensive, culturally sensitive, and coordinated* 46 U.S. average 60 Top 10% states 36 Bottom 10% states 53 White 39 Black 30 Hispanic 58 400% + of poverty 31 <100% of poverty 53 Private insurance 23 Uninsured 0 50 100 * Child had 1+ preventive visit in past year; access to specialty care; personal doctor/nurse who usually/always spent enough time and communicated clearly, provided telephone advice or urgent care and followed up after the child’s specialty care visits. Data: 2003 National Survey of Children’s Health (HRSA 2005; retrieved from Data Resource Center for Child and Adolescent Health database at http://www.nschdata.org). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. Figure 11. Test Results or Medical Record Not Available at Time of Appointment, Among Sicker Adults, 2005 Percent reporting test results/records not available at time of appointment in past two years International comparison United States, by race/ethnicity, income, and insurance status 40 30 30 28 27 23 19 20 11 12 GER AUS 16 16 NZ UK 21 20 18 0 CAN US White Black Hispanic Above average income Below average income Insured GER=Germany; AUS=Australia; NZ=New Zealand; UK=United Kingdom; CAN=Canada; US=United States. Data: Analysis of 2005 Commonwealth Fund International Health Policy Survey of Sicker Adults; Schoen et al. 2005a. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. Uninsured Figure 12. Duplicate Medical Tests, Among Sicker Adults, 2005 Percent reporting that doctor ordered test that had already been done in past two years United States, by race/ethnicity, income, and insurance status International comparison 40 25 23 23 21 20 20 18 16 15 11 9 10 NZ CAN AUS 12 6 0 UK US GER White Black Hispanic Above average income Below average income Insured UK=United Kingdom; NZ=New Zealand; CAN=Canada; AUS=Australia; US=United States; GER=Germany. Data: Analysis of 2005 Commonwealth Fund International Health Policy Survey of Sicker Adults; Schoen et al. 2005a. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. Uninsured Figure 13. Health Expenditure Growth 2000–2005 for Selected Categories of Expenditures Average annual percent growth in health expenditures, 2000–2005 20 15 10.7 10 8.6 8.0 7.9 12.0 6.1 5 0 Total Hospital care Physician & Nursing home & clinical services home health Source: A. Catlin et al., “National Health Spending in 2005: The Slowdown Continues,” Health Affairs, Jan./Feb. 2007 26(1):142–53. Prescription drugs Prog. admin. & net cost of private health insurance Figure 14. Percentage of National Health Expenditures Spent on Health Administration and Insurance, 2003 Net costs of health administration and health insurance as percent of national health expenditures 8 7.3 5.6 6 4.8 4.0 4 4.1 4.2 3.3 2.6 2.1 1.9 2.1 2 0 a ce n a Fr a2002 b1999 d an l n Fi an p Ja b da a n Ca om d ng e Ki th e d N ite n U c ds n rl a a tri s Au l ia nd a a r l st er u z t i A Sw c2001 *Includes claims administration, underwriting, marketing, profits, and other administrative costs; based on premiums minus claims expenses for private insurance. Data: OECD Health Data 2005. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. * y s n e t a ta m r S e d G te i Un Figure 15. Figure 16. Figure 17. Figure 18. Figure 19. Figure 20. Figure 21. Figure 22.