Figure ES-1. How Well Do Different Strategies
advertisement

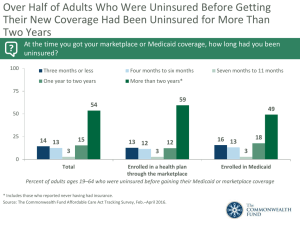
Figure ES-1. How Well Do Different Strategies Meet Principles for Health Insurance Reform? Tax Incentives and Individual Insurance Markets Mixed Private–Public Group Insurance with Shared Responsibility for Financing Public Insurance Covers Everyone 0 + + Minimum Standard Benefit Floor – + + Premium/Deductible/ Out-of-Pocket Costs Affordable Relative to Income – + + Easy, Seamless Enrollment 0 + ++ Choice + + + Pool Health Care Risks Broadly – + ++ Minimize Dislocation, Ability to Keep Current Coverage + ++ – Administratively Simple – + ++ Work to Improve Health Care Quality and Efficiency 0 + + Principles for Reform 0 = Minimal or no change from current system; – = Worse than current system; + = Better than current system; ++ = Much better than current system Figure 1. Figure 2. Employer-Provided Health Insurance, by Income Quintile, 2000–2006 Percent of population under age 65 with health benefits from employer 100% 80% 60% 88% 88% 87% 86% 85% 84% 77% 77% 62% 60% 75% 57% 87% 84% 74% 87% 83% 74% 87% 82% 72% 86% 82% Highest quintile Fourth 72% Third 55% 54% 54% 53% 40% 29% 26% 25% 23% 23% 20% 22% 22% Second Lowest quintile 0% 2000 2001 2002 2003 2004 2005 2006 Source: Analysis of the March Current Population Survey, 2001–07, by Elise Gould, Economic Policy Institute. Figure 3. Percentage of Uninsured Children Has Declined Since Implementation of SCHIP, but Gaps Remain 1999–2000 2005–2006 U.S. Average: 11.3% U.S. Average: 12.0% WA VT NH ME NH WA ND MT VT MT MN OR ID NY WI SD MI WY PA IA NE CA OH IN NV UT IL CO MA KS MO WV VA KY NJ RI CT MN OR ID MI PA IA NE CA IL CO KS MO AZ NM MS TX AL CT DE MD DC NC AZ GA NM OK SC AR MS LA TX AL GA LA FL AK VA NJ TN SC AR WV KY TN OK OH IN NV UT MA RI NY WI SD WY DE MD DC NC ME ND FL AK HI 16% or more 10%–15.9% HI 7%–9.9% Less than 7% Source: J. C. Cantor, C. Schoen, D. Belloff, S. K. H. How, and D. McCarthy, Aiming Higher: Results from a State Scorecard on Health System Performance (New York: The Commonwealth Fund, June 2007). Updated Data: Two-year averages 1999–2000, updated with 2007 CPS correction, and 2005–2006 from the Census Bureau’s March 2000, 2001 and 2006, 2007 Current Population Surveys. Figure 4. Uninsured Nonelderly Adult Rate Has Increased from 17.3 Percent to 20.0 Percent in Last Five Years 1999–2000 2005–2006 NH NH ME VT WA NH WA ND MT VT MT MN OR ID NY WI SD MI WY PA IA NE CA OH IN NV UT IL CO MA KS MO WV VA KY NJ RI CT MN OR ID MI PA IA NE CA IL CO KS MO AZ NM MS TX AL DE MD DC NC AZ GA NM OK SC AR MS LA TX AL GA LA FL AK VA NJ RI CT TN SC AR WV KY TN OK OH IN NV UT MA NY WI SD WY DE MD DC NC ME ND FL AK HI 23% or more 19%–22.9% HI 14%–18.9% Less than 14% Source: J. C. Cantor, C. Schoen, D. Belloff, S. K. H. How, and D. McCarthy, Aiming Higher: Results from a State Scorecard on Health System Performance (New York: The Commonwealth Fund, June 2007). Updated Data: Two-year averages 1999–2000, updated with 2007 CPS correction, and 2005–2006 from the Census Bureau’s March 2000, 2001 and 2006, 2007 Current Population Surveys. Figure 5. Prevalence of High Family Out-of-Pocket Cost Burdens by Poverty Status Among the Nonelderly Population, 1996 and 2003 Percent of nonelderly adults who spend >10% of disposable household income on out-of-pocket premiums and expenditures on health care services 75 1996 2003 50 33.3 25 15.8 19.2 25.9 24.1 23.7 15.6 22.7 7.1 9.7 0 Total <100% FPL 100%–<200% 200%–<400% FPL 400%+ FPL FPL Source: J. S. Banthin and D. M. Bernard, “Changes in Financial Burdens for Health Care: National Estimates for the Population Younger Than 65 Years, 1996 to 2003,” Journal of the American Medical Association, Dec. 13, 2006 296(22):2712–19. Figure 6. Access Problems Because of Costs in Five Countries, Total and by Income, 2004 Percent of adults who had any of three access problems* in past year because of costs 80 Below average income Above average income 57 44 40 40 35 34 29 29 26 24 25 17 12 9 12 6 0 UK CAN AUS NZ US UK CAN * Did not get medical care because of cost of doctor’s visit, skipped medical test, treatment, or follow-up because of cost, or did not fill Rx or skipped doses because of cost. UK=United Kingdom; CAN=Canada; AUS=Australia; NZ=New Zealand; US=United States. Data: 2004 Commonwealth Fund International Health Policy Survey of Adults’ Experiences with Primary Care (Schoen et al. 2004; Huynh et al. 2006). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. AUS NZ US Figure 7. Receipt of All Three Recommended Services for Diabetics, by Race/Ethnicity, Family Income, Insurance, and Residence, 2002 Percent of diabetics (ages 18+) who received HbA1c test, retinal exam, and foot exam in past year Total 53 55 White 54 Black 38 Hispanic 61 400% + of poverty 200% –399% of poverty 50 100% –199% of poverty 47 46 <100% of poverty Private* 54 24 Uninsured Urban** 55 45 Rural 0 50 * Insurance for people ages 18–64. ** Urban refers to metropolitan area >1 million inhabitants; Rural refers to noncore area <10,000 inhabitants. Data: 2002 Medical Expenditure Panel Survey (AHRQ 2005a). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 100 Figure 8. Adults Without Insurance Are Less Likely to Be Able to Manage Chronic Conditions Percent of adults ages 19–64 with at least one chronic condition* Insured all year Insured now, time uninsured in past year Uninsured now 75 58 59 50 27 25 18 35 16 0 Skipped doses or did not fill Visited ER, hospital, or both for chronic prescription for chronic condition condition because of cost * Hypertension, high blood pressure, or stroke; heart attack or heart disease; diabetes; asthma, emphysema, or lung disease. Source: S. R. Collins, K. Davis, M. M. Doty, J. L. Kriss, and A. L. Holmgren, Gaps in Health Insurance: An All-American Problem, Findings from the Commonwealth Fund Biennial Health Insurance Survey (New York: The Commonwealth Fund, Apr. 2006). Figure 9. Receipt of Recommended Screening and Preventive Care for Adults, by Family Income and Insurance Status, 2002 Percent of adults (ages 18+) who received all recommended screening and preventive care within a specific time frame given their age and sex* National 49 400%+ of poverty 56 200%–399% of poverty 48 <200% of poverty 39 Insured all year 52 Uninsured part year 46 Uninsured all year 31 0 50 * Recommended care includes seven key screening and preventive services: blood pressure, cholesterol, Pap, mammogram, fecal occult blood test or sigmoidoscopy/colonoscopy, and flu shot. Data: B. Mahato, Columbia University analysis of 2002 Medical Expenditure Panel Survey. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 100 Figure 10. Preventive Care Visits for Children, by Top and Bottom States, Race/Ethnicity, Family Income, and Insurance, 2003 Percent of children (ages <18) received BOTH a medical and dental preventive care visit in past year 59 U.S. average 73 Top 10% states 48 Bottom 10% states 62 White 58 Black 49 Hispanic 70 400% + of poverty 48 <100% of poverty 63 Private insurance 35 Uninsured 0 50 Data: 2003 National Survey of Children’s Health (HRSA 2005; retrieved from Data Resource Center for Child and Adolescent Health database at http://www.nschdata.org). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. 100 Figure 11. Children with a Medical Home, by Top and Bottom States, Race/Ethnicity, Family Income, and Insurance, 2003 Percent of children who have a personal doctor or nurse and receive care that is accessible, comprehensive, culturally sensitive, and coordinated* 46 U.S. average 60 Top 10% states 36 Bottom 10% states 53 White 39 Black 30 Hispanic 58 400% + of poverty 31 <100% of poverty 53 Private insurance 23 Uninsured 0 50 100 * Child had 1+ preventive visit in past year; access to specialty care; personal doctor/nurse who usually/always spent enough time and communicated clearly, provided telephone advice or urgent care and followed up after the child’s specialty care visits. Data: 2003 National Survey of Children’s Health (HRSA 2005; retrieved from Data Resource Center for Child and Adolescent Health database at http://www.nschdata.org). Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. Figure 12. Figure 13. People with Capped Drug Benefits Have Lower Drug Utilization, Worse Control of Chronic Conditions 50 Benefits Not Capped 49.2 Benefits Capped 38.5 45.2 39.5 31.4 26.5 26.2 25 21.2 19.6 18.1 21.3 17 14.6 19.7 16.6 18.7 0 t i-H An B r ug Pd s e ow l id Lip g dr u g rin s A b dia i t n eti s rug d c Percent of Drug Nonadherence h Hig BP h Hig ch s ole ol ter hb Hig loo lu dg s co ev el els Percent of Poor Physiological Outcomes E is Dv it s le ne o N cti v o eh i sp n tio za i l ta s Rate* of Medical Services Use * Rate per 100 person-years. Source: J. Hsu, M. Price, J. Huang et al., “Unintended Consequences of Caps on Medicare Drug Benefits,” New England Journal of Medicine, June 1, 2006 354(22):2349–59. Figure 14. Cost-Sharing Reduces Use of Both Essential and Less Essential Drugs and Increases Risk of Adverse Events Percent reduction in drugs per day 25 Elderly 22 140 120 20 14 15 10 Low Income Percent increase in incidence per 10,000 15 100 Elderly Low Income 117 97 78 80 9 43 60 40 5 20 0 0 Essential Less Essential Adverse Events ED Visits Source: R. Tamblyn, R. Laprise, J. A. Hanley et al., “Adverse Events Associated with Prescription Drug Cost-Sharing Among Poor and Elderly Persons,” Journal of the American Medical Association, Jan. 24/31, 2001 285(4):421–29. Figure 15. Many Americans Have Problems Paying Medical Bills or Are Paying Off Medical Debt Percent of adults ages 19–64 who had the following problems in past year: Total Insured all year Uninsured during the year 75 53 50 25 42 23 26 16 13 8 26 14 21 18 29 34 26 9 0 Not able to pay Contacted by medical bills collection agency* Had to change Medical way of life to pay bills/debt being medical bills paid off over Any medical bill problem or outstanding debt time * Includes only those who had a bill sent to a collection agency when they were unable to pay it. Source: S. R. Collins, K. Davis, M. M. Doty, J. L. Kriss, and A. L. Holmgren, Gaps in Health Insurance: An All-American Problem, Findings from the Commonwealth Fund Biennial Health Insurance Survey (New York: The Commonwealth Fund, Apr. 2006). Figure 16. One-Quarter of Adults with Medical Bill Burdens and Debt Were Unable to Pay for Basic Necessities Percent of adults ages 19–64 with medical bill problems or accrued medical debt Percent of adults reporting: Total Insured all year Insured now, time uninsured during year Uninsured now 19% 28% 40% Unable to pay for basic necessities (food, heat, or rent) because of medical bills 26% Used up all of savings 39 33 42 49 Took out a mortgage against home or took out a loan 11 10 12 11 Took on credit card debt 26 27 31 23 Source: S. R. Collins, K. Davis, M. M. Doty, J. L. Kriss, and A. L. Holmgren, Gaps in Health Insurance: An All-American Problem, Findings from the Commonwealth Fund Biennial Health Insurance Survey (New York: The Commonwealth Fund, Apr. 2006). Figure 17. Increased Health Care Costs Associated with Reduced Savings Has increased spending on health care expenses in the past year caused you to do any of the following? Among those with health insurance coverage who had increases in health care costs in the last year (percentage saying “yes”) 45% Decrease your contributions to other savings 53% 34% Have difficulty paying for other bills 37% 29% Use up all or most of your savings 33% Decrease your contributions to a retirement plan, such as a 401(k), 403(b), or 457 plan, or an IRA 26% 36% 24% Have difficulty paying for basic necessities, like food, heat, and housing Borrow money Source: EBRI Health Confidence Survey, 2005 and 2006. 28% 18% 21% 2005 2006 Figure 18. International Comparison of Spending on Health, 1980–2005 Average spending on health per capita ($US PPP) 7000 6000 United States Germany Canada France Australia United Kingdom Total expenditures on health as percent of GDP 16 14 5000 12 4000 10 8 3000 6 2000 4 19 80 19 82 19 84 19 86 19 88 19 90 19 92 19 94 19 96 19 98 20 00 20 02 20 04 0 2 0 19 80 19 82 19 84 19 86 19 88 19 90 19 92 19 94 19 96 19 98 20 00 20 02 20 04 1000 United States Germany Canada France Australia United Kingdom Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. Updated data from OECD Health Data 2007. Figure 19. Americans Spend More Out-of-Pocket on Health Care Expenses Total health care spending per capita $7,000 United States $6,000 $5,000 $4,000 France $3,000 Netherlands $2,000 Canada Germany a OECD Median New Zealand Australiab Japana $1,000 $0 $0 $100 $200 $300 $400 $500 $600 Out-of-pocket spending per capita a2003 b2003 Total Health Care Spending, 2002 OOP Spending Source: The Commonwealth Fund, calculated from OECD Health Data 2006. $700 $800 $900 Figure 20. Increases in Health Insurance Premiums Compared with Other Indicators, 1988–2007 Percent Health insurance premiums 20 Workers’ earnings 18.0 Overall inflation 15 ^ National health expenditures 13.9 per capita 12.9* 12.0 10 10.9* 8.5 8.2* 5.3* 5 9.2* 7.7* 0.8 19 88 19 89 19 90 19 91 19 92 19 93 19 94 19 95 19 96 19 97 19 98 19 99 20 00 20 01 20 02 20 03 20 04 20 05 20 06 20 07 0 11.2* * Estimate is statistically different from the previous year shown at p<0.05. ^ Estimate is statistically different from the previous year shown at p<0.1. Note: Data on premium increases reflect the cost of health insurance premiums for a family of four. Historical estimates of workers’ earnings have been updated to reflect new industry classifications (NAICS). Source: G. Claxton, J. Gabel et al., "Health Benefits in 2007: Premium Increases Fall to an Eight-Year Low, While Offer Rates and Enrollment Remain Stable," Health Affairs, Sept./Oct. 2007 26(5):1407–16. Kaiser/HRET Survey of Employer-Sponsored Health Benefits, 2007, and Commonwealth Fund analysis of National Health Expenditures data. 6.1* Figure 21. Health Expenditure Growth 2000–2005 for Selected Categories of Expenditures Average annual percent growth in health expenditures, 2000–2005 20 15 10.7 10 8.6 8.0 7.9 12.0 6.1 5 0 Total Hospital care Physician & Nursing home & clinical services home health Prescription drugs Source: A. Catlin, C. Cowan, S. Heffler et al., “National Health Spending in 2005: The Slowdown Continues,” Health Affairs, Jan./Feb. 2007 26(1):142–53. Prog. admin. & net cost of private health insurance Figure 22. Percentage of National Health Expenditures Spent on Health Administration and Insurance, 2003 Net costs of health administration and health insurance as percent of national health expenditures 8 7.3 5.6 6 4.8 4.0 4 4.1 4.2 3.3 2.6 2.1 1.9 2.1 2 0 a ce n a Fr a2002 b1999 d an l n Fi an p Ja b da a n Ca om d ng e Ki th e d N ite n U c ds n rl a a tri s Au l ia nd a a r l st er u z t i A Sw c2001 *Includes claims administration, underwriting, marketing, profits, and other administrative costs; based on premiums minus claims expenses for private insurance. Data: OECD Health Data 2005. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2006. * y s n e t a ta m r S e d G te i Un Figure 23. Employers Provide Health Benefits to More than 160 Million Working Americans and Family Members Numbers in millions, 2006 Military 3.4 (1%) Uninsured 47.0 (16%) Employer 163.3 (55%) Individual 16.0 (5%) Uninsured 46.4 (18%) Military 3.4 (1%) Employer 160.8 (62%) Individual 15.8 (6%) Medicaid 27.9 (9%) Medicaid 27.9 (11%) Medicare 39.1 (13%) Total population = 296.7 Source: Current Population Survey, March 2007. Medicare 6.4 (2%) Under-65 population = 260.7 Figure 24. How Well Do Different Strategies Meet Principles for Health Insurance Reform? Tax Incentives and Individual Insurance Markets Mixed Private–Public Group Insurance with Shared Responsibility for Financing Public Insurance Covers Everyone 0 + + Minimum Standard Benefit Floor – + + Premium/Deductible/ Out-of-Pocket Costs Affordable Relative to Income – + + Easy, Seamless Enrollment 0 + ++ Choice + + + Pool Health Care Risks Broadly – + ++ Minimize Dislocation, Ability to Keep Current Coverage + ++ – Administratively Simple – + ++ Work to Improve Health Care Quality and Efficiency 0 + + Principles for Reform 0 = Minimal or no change from current system; – = Worse than current system; + = Better than current system; ++ = Much better than current system