By: Diana Blum RN MSN Metropolitan Community College
advertisement

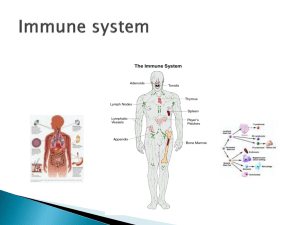
By: Diana Blum RN MSN Metropolitan Community College Bone marrow= spongy center of the bones where WBCs are made Lymphatic System= network of open ended tubes separate from the blood circulation system that collects the plasma left behind and returns it to the venous system. WBC travel through the tissues looking infection Lymph fluid=mix of plasma and cells Propelled along the lymphatic system by normal muscle contraction One way valves prevent the fluid from pooling Lymph nodes= small patches of tissue that filter microorganisms from the lymph fluid before it is returned to the bloodstream. Located throughout the body Swell with infection and cancer Spleen= in LUQ of the abdomen. Filters microorganisms from the blood. Once trapped, WBCs destroy them Removed if Trauma (MVA), hodgkin’s dx ▪ Greater risk of infection Thymus= located below the thryoid Early in life WBCs called lymphocytes migrate from bone marrow to the thymus where they mature into T Cells As humans age the thymus shrinks Stem Cells=called progenitor cells Develop into various WBCs, RBCs, or Platelets Most located in bone marrow Some circulate in blood WBCS (Leukocytes)=produced by bone marrow Identify and destroy antigens (proteins) Life span of WBC is 12 hours Macrophages= clean up WBC debris If WBCs build faster than macrophages can clean pus is formed. Neutrophils=fight bacterial infections Most numerous of the WBCs about 60% Monocytes= circulate for 1 day before entering tissue Macrophages=monocytes when they enter tissue Destroyed during phagocytosis ▪ Ingest foreign material and can live months to years Eosinophils=combat parasitic infections Also associated with allergic responses Basophils= can initiate massive inflammatory response to bring other WBCs to infection site Work with Immunoglobin E (IgE) by releasing histamine from cell vesicles in the basophil ▪ Histamine is a potent vasodialator that increases blood circulation to the site Mast cells= store histaminein cell vesicles. Located in tissue B cells= manufacture antigen binding proteins (immunoglobins) on the cell membrane when immunoglobin binds w/ antigen, the b cell is stimulated to produce plasma cells and memory B cells. Plasma cells are antibody factories that produce large amounts of immunoglobins. Memory B cells go into a resting state but can be quickly reactivated. Once immunoglobin released it is called an antibody. ▪ 4 types ▪ IgM=first to be secreted during primary immune response ▪ IgG= secreted during 2nd ary immune response ▪ IgA=present in secretions like mucus and mother’s milk ▪ IgE=attaches to the cell membrane of basophils and mast cells where it triggers the cell to release histamine. T Cells= 2 types: T helper(CD4) and T cytotoxic CD4 cells are found on cell membrane When CD4 cells come in contact with foreign antigens they secrete cytokines that activate other components of immune system CD4 cells can be infected with HIV Tc cells= CD8 cells because protein complex on cell membrane. Tc cells destroy invaders Cytokines= hormones secreted by cells to signal others (interferon, interleukin, tumor necrosis factor, granulocyte=macrophage colony stimulating factor, EPO) Eicosanoids=class of fatty acids that regulate blood vessel vasodilation, temperature elevation, WBC activation NSAIDS disrupt production Innate immunity: operational at all times Present at birth Include– barriers, inflammatory response, phagocytosis ▪ Barriersskin and mucous membranes= first line of defense, sweat glands ▪ Inflammatory responsedilate capillaries to increase permeability of affected area ▪ s/s: rubor (redness), tumor (swelling), Calor (heat), and dolor (pain) ▪ Phagocytosis process of ingesting and digesting invading pathogens, dead cells, and cellular debris ▪ Neutrophils, monocytes, and macrophages are capable and sometimes refered to as phagocytes Acquired immunity=fights a particular pathogen and is only activated when needed 2 types ▪ Antibody mediated: activated when IgM detects foreign antigen. See page 594 ▪ Can be active or passive Active:the person manufactures antibodies in response to infection ***permanent Passive:antibody is produced by animal or person and then transferred to another (ex. through breast milk) ***lasts 1-2 months after antibodies received ▪ Cell mediated: aimed at intracellular defects like virus and cancer ▪ Delays hypersensitivity reactions and transplant rejections ▪ Tc are primary component ▪ When Tc cells recognize foreign antigens they secrete cytotoxic substances to destroy the defective cell (transplant organ) Immune system must be able to recognize its own proteins and not fight itself Occurs as part of neonatal growth Autoimmune diseases occur when: Example: acute rheumatic fever, lupus, rheumatoid arthritis, diabetes, thyroiditis, graves disease Bone marrow is less productive Immunity not usually affected unless unusual stress, trauma, chronic infection, cancer tx Lymphatic tissue grows between age 6-20 As we age lymph tissue shrinks Result is fewer and smaller lymph nodes Hx of present illness: frequent infections, prolonged bleeding, easy bruising, chronic fatigue PMH: cancer, HIV, Splenectomy, long term venous access device, infections, current meds, immunizations System review: skin-rash ulcers, enlarged lymph nodes NeuroRespiratoryGIGUMuscleEndocrine- See page 630 Hobbies Occupation Self concept Activity and exercise Sleep and rest Nutrition Interpersonal relations Coping and stress Health perception Urine Tests-urine protein electrophoresismeasures immunoglobin in the urine Blood tests: CBC Serum protein electrophoresis(measures immunoglobin in the blood) (used to look for multiple myeloma) Antinuclear antibody test-looks for lupus ELIZA- looks for HIV/AIDS Cultures-detect infection of blood, sputum, urine, stool Bone marrow biospy- done if CBC abnormal Diagnoses leukemia, WBC cancer, and Multiple Myeloma See page 600 Lymphangiography-evaluates anatomy of lymph vessels and lymph nodes Helps stage cancer Liver- Spleen Scan-evaluates size and function of liver and spleen Gallium Scan-uses radioactive tracer to detect presence of malignancy Skin tests-Ex. TB tine The lower the WBC the greater chance of infection See page 635 Pvt room Vistors wash hands Monitor vs q2-4 hours Aseptic technique Isolation C and DB Patient wears mask when outside room No fresh flowers or plants in room Stimulates bone marrow to produce more blood cells Drugs may be given to stimulate ex. Neupogen Done to restore immune system Complications: infection, thrombocytopenia, renal insufficiency, graft vs host dx Neutropenia: neutrophils level low Leukemia: cancer of WBC- bone marrow produces too many immature cells Cause: exposure to benzene, large dose of radiation 2 types: ▪ myelogenous-most often in adults ▪ Lymphocytic-most often in kids 2-6 yrs old- At risk for severe infection and bleeding s/s:infection, fever, nite sweats, low RBC ct, fatigue, paleness, tachycardia, tachypnea, petechiae, purpura, epistaxsis, gingival bleed, melena (blood in stool), bone pain, weight loss, swollen lymph nodes Tx: high dose chemo, therapy Induction therapy-initial dose of chemo Maintenance therapy- lower dose of chemo over 1-3 years Intensification and consolidation therapybone marrow transplant(monitor for infection, bleeding) Risk for injury r/t infection aeb thrombocytopenia and anemia. Goal absence of injury from infection, bleeding, and inadequate oxygenation aeb normal body temperature, no bruising, or frank bleeding, pulse and respiratory, rates WNL Fatigue Impaired oral mucous membranes Imbalanced nutrition<less than body requirements Anxiety Ineffective therapeutic regimen management Thorough hand washing Encourage patient to shower everyday Discourage patients from eating fresh fruit and veggies and dairy Possible transfusions Monitor for stomatitis Encourage patients and family to express their feelings and ask questions LUPUS S/S: Butterfly rash= characteristic sign, malaise, anorexia, muscle pain, swollen joints, photosensitivity etc DX: no one test definitely diagnoses SLE Tx: No cure. Minimize symptoms, steroids, cytotoxic agents Initial: lasts 4-8 weeks High levels in blood Flulike symptoms Latent: inactive until a virus presents than replication begins Lasts 2-12 years Asymptomatic Third stage=opportunistic infections 2-3 years Once CD4 Level below 200 it is considered AIDS Opportunistic infections Pneumonia Herpes CMV retinitis Meningitis toxoplasmosis Wasting Weight loss malnutrition Cancer Kaposi’s sarcoma Non hodgkins Anal cancer Cervical cancer Dementia From encephalitis Flu like symptoms Fever Night sweats Swollen lymph nodes Headache Skin lesions that don’t heal Sore throat Dyspnea Burning with urination diarrhea Fatigue Weight loss Positive ELIZA test Positive Western Blot test No cure Treat symptoms Prevent infections Encourage to eat balanced diet Exercise regularly Maintain good dental hygiene Smoking/illegal drug cessation Limit alcohol Minimize stress Practice safe sex Early stages- usually treated outpatient Late stages- more intensive in nature Infection is the leading cause of death in those with HIV Ineffective therapeutic regimen Anxiety Infection Impaired oral mucosa Imbalanced nutrition less than body requirements Disturbed thought process pain Provide education Offer support group Encourage questions Encourage them to express self Anti infectives Medication education Encourage regular dental hygiene Have dietician see Appetite stimulants Saftey precautions Monitor pain Estimated 53900 new cases diagnosed in 2002 Stages Low grade Intermediate grade High grade The higher the grade the more aggressive Tx: chemo, bone marrow transplant, stem cell transplant 5 year survival rate is 52% Characterized by reed- sternberg cells in the lymph nodes Highest occurance is in 20s and50s Men are more likely than women to have Tx: radiation, chemo, bone marrow transplant, stem cell transplant Survival rates vary 5 yr survival rate is 82% Cancer of the plasma cells Most common over the age of 60 No known cause Genetics and radiation exposure play a part s/s: bone pain, hyperuricemia (kidneys), anemia, hypercalcemia, fractures, spinal cord compression Diagnosis: radiographs, serum and urine protein electrophoresis, bone marrow biopsy No known cure Tx: chemo and radiation to treat symptoms