Chapter 12 The Lymphatic and Body Defenses
advertisement

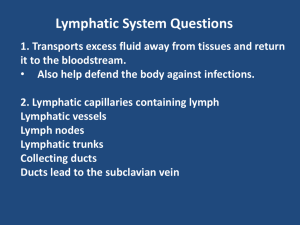
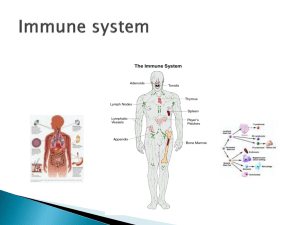
Chapter 12 The Lymphatic and Body Defenses • General – subsystem of circulatory system – functions • fight disease • clean blood • fluid balance – a drainage system • 3 liters liquid out of blood per day blood capillaries reabsorb 85% • 15% (2 – 4 L/day) of the water and about half of the plasma proteins enters lymphatic system and then returned to the blood Lymphatic and Immune Systems Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Capillary bed Tissue fluid Tissue cell Lymphatic capillary Venule Arteriole Figure 21.3a (a) • maintain fluid balance • protect body from infection and disease 21-4 • Circulation – lymph fluid • interstitial fluid “clear ” – lymph capillaries • take fluid out of capillary beds by diffusion – lymph vessels “lymphatics” • carry fluid through the body – lymph nodes- axillary cervical inguinal - about 450 in young adult • remove foreign substances • macrophages, lymphocytes, monocytes • nodes inflamed tender “bubo” Lymphatic ducts • right lymphatic duct- drains the right arm, shoulder area, and the right side of the head and neck. • thoracic duct-drains everything else, including the legs, GI tract and other abdominal organs, thoracic organs, and the left side of the head and neck and left arm and shoulder. • lymph ---> into blood via subclavian veins Lymphatic Drainage of Mammary and Axillary Regions Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Right lymphatic duct Right subclavian vein Axillary lymph nodes Lymphatics of breast (b) 21-9 Figure 21.6b The Fluid Cycle Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Lymphatic system Cardiovascular system Cervical lymph nodes Lymphatic capillaries Pulmonary circuit Lymph nodes Palatine tonsil L. internal jugular v. Thoracic duct R. lymphatic duct Thymus Lymphatic trunks Collecting duct Axillary lymph node Subclavian vein Thoracic duct Cisterna chyli Spleen R. and l. lumbar trunks Abdominal, intestinal, and mesenteric lymph nodes Superior vena cava Collecting vessels Intestinal trunk Red bone marrow Inguinal lymph nodes Blood flow Popliteal lymph nodes Lymph flow Systemic circuit Lymphatic vessels Lymphatic capillaries Figure 21.5 21-10 Figure 21.1 • Other Lymphatic Organs – spleen • make lymphocytes • filter out debris and deadly pathogens – thymus gland • T cells, more immunocompetent – Peyer’s Patches • end of ileum – MALT mucosa associated lymphatic tissue • tonsils, Peyers patches, and appendix – tonsils • rings of lymphatic tissues that trap pathogens crypts – palatine tonsils • pair at posterior margin of oral cavity • most often infected – lingual tonsils • pair at root of tongue – pharyngeal tonsil (adenoid) • single tonsil on wall of nasopharynx • Tonsillectomy removal of palatine & linguinal Defenses Against Pathogens • pathogens – environmental agents capable of producing disease – infectious organisms, toxic chemicals, and radiation • three lines of defenses against pathogens: – first line of defense – external barriers, skin and mucous membranes – second line of defense – several nonspecific defense mechanisms • leukocytes and macrophages, antimicrobial proteins, immune surveillance, inflammation, and fever • effective against a broad range of pathogens – third line of defense – the immune system • defeats a pathogen, and leaves the body of a ‘memory’ of it so it can defeat it faster in the future 21-15 Non - Specific Body Defense • Surface membranes – skin • many layers - closely packed cells • pH 5.5 – epithelial & mucous membranes • saliva & tears : lysozyme • cilia - move foreign substances to esophagus • stomach - gastric juice - HCl pH 1-2 • mucus - trap pathogens & dirt Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Mobilization of Defenses • leukocyte behavior Splinter – margination From damaged tissue • selectins cause leukocytes to adhere to blood vessel walls 1 Inflammatory chemicals Bacteria From mast cells From blood Mast cells • leukocytes squeeze between endothelial cells into tissue space 4 Chemotaxis Increased permeability 3 Neutrophils – diapedesis (emigration) 5 Phagocytosis 2 Margination Blood capillary or venule Diapedesis 21-17 Figure 21.19 • White Blood Cells- Leukocytes – defense and immunity 5000 - 10,000 WBC’s • neutrophil’s ~ 3,000 - 7,000 54-62% of WBC –Phagocytes –Chemical killing zone(superoxide, H2O2, hypochlorite) • eosinophils ~ 100-400 1-3% of WBC –Chemicals (superoxide, H2O2, toxins) – kill parasitic worms allergies • basophils ~ 20-30 less than 1% of WBC –secrete histamines - vasodilators –chemicals to kill foreign substances –heparin • Monocytes 100-700 3-9 % of WBC – Large cells – Macrophages- go into connective tissue – Present in chronic infections • Lymphocytes ~ 1500 – 3000 25-33% – small cells - r.b.c size – Provide immunity B cells, T cells, and natural killer cells – Secrete antibodies Macrophages Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Macrophages Pseudopods Bacteria Peter Arnold, Inc. 21-20 Figure 21.7 5 µm – inflammation • secondary line of defense • heat red swelling and pain • seal off area / more blood • histamines and kinins inflammatory chemicals also attract neutrophils • pus : dead neutrophil’s & dead pathogens • absceses • Antimicrobial Chemicals – complement • 20 plasma proteins attach to foreign cells – interferon • proteins released from virus infected cells which protects other cells from virus – fever • w.b.c secrete pyrogens • raise body temp. inhibits bacterial growth • Decreases iron in blood- inhibits growth of bacteria and fungi • Increases phagocytic action Specific Defense Mechanisms • General – types • cellular ~ lymphocytes T cells • humoral ~ antibodies B cells – immune response • antigen specific • systemic • memory • Antigens – proteins which cause an immune response • Cells of the Immune System – lymphocytes • T cells - cell mediated • B cells - make antibodies humoral – macrophages • • • • engulf foreign particles – monocytes neutrophils T cells - release chemicals create macrophages T’ stand for thymus derived have best ability to recognize foreign antigens – B cells • bind to antigens • T helper cells release chemical so B cells make clones • plasma cells secrete antibodies • B cells can become memory cells remember foreign antigens • Active Immunity – have or exposed to disease – naturally acquired - had disease – artificially “ - vaccine – vaccines - dead, weakened pathogen • Passive Immunity – antibodies transferred – naturally acquired - placenta “mother’s milk” IgG’s – artificial “ – gamma globulins • Antivenoms tetanus botulism • Antibodies – Structure – – Classes of Antibodies • IgM - 1st released B cells • IgA - in tears saliva mucus • IgD - activate B cells • IgG - most abundant -- > placenta • IgE - skin gastrointestinal respiratory tracts release histamine – Antibody function • complement system - antibodies bind to antigen lyse foreign cells • neutralization - antibodies bind to specific sites or neutralize foreign substances • agglutination - antibodies bind to antigens --> clumping effect • precipitation - antibodies and antigens form precipitate insoluble substances Cell Mediated Immunity • T Cells – killer T cells - secret chemical --> kill virus infested cells – helper T cells - stimulate production of killer T and B cells – suppresor T Cells - slows killer and B cells • Memory Cells – B plasma cells- secrete antibodies Organ Transplant and Rejection • Grafts - 75 % match – autografts • same person site to site – isografts • twin identical – allografts • unrelated persons – xenografts • different species Disorders of Immunity • Allergies – abnormal immune response – immediate hypersensitivity • inflammatory response • runny nose, watery eyes, itching, redness • basophiles IgE --> histamines • acute systemic- anaphylatic shock – delayed hypersensitivity • reaction 1-3 days • T cells release lympokines • poison ivy • Immunodeficiencies – SCID - lack of B and T cells vulnerability to opportunistic infection and must live in protective enclosures – AIDS - destroy helper T cells • incubation period from several months to 12 years • Autoimmune Disease – against its own tissue – some resulting disease • multiple sclerosis • myasthenia gravis • graves disease • systemic lupus • rheumatoid arthritis • Hashimotos thyroditis – causes • virus or infection alters your self protection Developmental Aspects • Immunity – genetics – stress – depression – mind over matter – diet