The Digestive System Chapter 23
advertisement
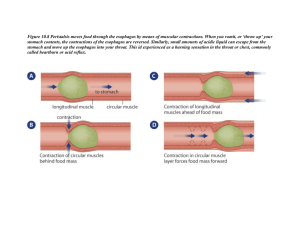
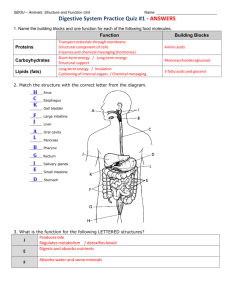
The Digestive System Chapter 23 The Digestive System Structures of the Digestive Tract: • Alimentary canal - The continuous tube from mouth to anus whose organs perform various digestive functions • Accessory structures - the additional organs and glands that play a role in digestion Figure 23.1 The Digestive System Functions of the Digestive System: • Ingestion - taking food into the alimentary canal at the mouth • Propulsion - the movement of food through the alimentary canal • Peristalsis – waves of muscle contraction that propel food • Mechanical digestion - physical breakdown of food into smaller pieces • Segmentation – contractions of the alimentary canal that mixes food • Chemical digestion - food molecules are broken down via enzymes • Absorption - transport of digested materials from lumen through an epithelium into the blood or lymph • Defecation – removal of indigestible materials through the anus Figure 23.2 The Peritoneum The Peritoneum - the serous membrane lining the abdominal/pelvic body cavity Visceral layer - lines the surfaces of the organs in the cavity Parietal layer – lines the inside of the body wall Peritoneal cavity - serous fluid-filled space between the visceral and parietal layers Figure 23.5 The Peritoneum Mesentery - a double layer of serous membrane that suspends organs in the abdominal body cavity Intraperitoneal – refers to organs that hang into the peritoneal cavity, suspended from mesenteries Retroperitoneal – refers to structures behind parietal peritoneum Figure 23.5 The Alimentary Canal Layers of the Alimentary Canal: • Mucosa - Innermost layer composed of epithelium, specialized for secretion and absorption • Submucosa - Connective tissue with glands, blood vessels, lymphatics, and nerves • Muscularis - Layers of smooth muscle • Circular layer – inner layer controlling lumen size • Longitudinal layer – outer layer controlling canal length • Serosa – serous membrane, also called the visceral peritoneum Figure 23.6 The Oral Cavity Oral cavity - start of the alimentary canal where ingestion occurs. Begins mechanical digestion via chewing (mastication) and chemical digestion via enzymes • Teeth - bony structures used in mastication • Tongue – skeletal muscle used to manipulate food and form a bolus • Palate – roof of the oral cavity, hard and soft regions • Uvula – extension of the soft palate, blocks the nasopharynx during swallowing Figure 23.7a Salivary Glands Salivary glands – paired glands that secrete saliva into the oral cavity to moisten food and cleanse the mouth Saliva – secretion containing salivary amylase which begins chemical digestion of starches. Also contains IgA antibodies and lysozymes to clear potential pathogens Figure 23.9 The Pharynx Pharynx - Begins propulsion, transporting food from the oral cavity to the esophagus, performing the act of deglutition (swallowing) • Only the oropharynx and laryngopharynx transport food Figure 23.7a The Esophagus Esophagus - Transports food from the pharynx to the stomach Esophageal Hiatus – Opening in the diaphragm, allowing passage of esophagus from thorax to abdomen Figure 23.12 The Esophagus Deglutition – when swallowing, the elevation of the larynx and uvula block the respiratory passages ensuring flood enters the esophagus Figure 23.13a The Esophagus Gastroesophageal sphincter (cardiac sphincter) - circular muscle allowing passage into stomach and prevents regurgitation Heartburn – burning when acidic gastric juices regurgitate into the esophagus Figure 23.13d, e The Stomach Stomach – stores food, performing mechanical digestion via churning and chemical digestion via enzymes Chyme – the acidic, paste-like substance passed to the small intestine after about 4 hours Regions: The cardia is nearest to the esophagus, the fundus is the superior dome, the body is the central region, and the pylorus is nearest the small intestine Figure 23.14 The Stomach Curvatures: the lateral surface of the stomach is the convex greater curvature, while the medial surface is the concave lesser curvature Rugae – large folds of the mucosa allowing expansion Muscle layers – only organ in the alimentary canal with 3 layers, outer longitudinal, middle circular, and inner oblique Pyloric sphincter – circular muscle regulating chyme movement into the small intestine Figure 23.14 The Omenta Omenta – the 2 mesenteries that attach to the surfaces of the stomach • Lesser omentum – mesentery from liver to the lesser curvature of the stomach • Greater omentum – largest mesentery draping from the greater curvature of the stomach Figure 23.30d The Stomach Gastric pits/glands – invaginations of the stomach mucosa containing cells that produce the gastric juices • Chief cells – secrete pepsinogen that quickly becomes pepsin, a protein enzyme that works best in acidic pH • Parietal cells – secrete hydrochloric acid (HCl), to produce acidic environment • Mucous neck cells – produce mucus that with the mucous of goblet cells protects the mucosa • Enteroendocrine cells – secrete local hormones to regulate stomach activity Figure 23.15 The Stomach Gastic Juice Secretion: 1. Cephalic phase – smell or thought of food begins limited gastric secretions 2. Gastric phase – stretch and chemicals in stomach trigger largest secretions 3. Intestinal phase – a balance of excitatory and inhibitory actions • Excitatory – movement of chyme into intestine triggers continued secretion Figure 23.16 The Stomach Gastic Juice Secretion: 3. Intestinal phase – a balance of excitatory and inhibitory actions • Excitatory – movement of chyme into intestine triggers continued gastric secretion • Inhibitory – stretch of duodenum inhibits gastric secretion and motility (prevents overload of duodenum) Figure 23.16 The Small Intestine Small intestine – coiled digestive organ transporting food from stomach to large intestine. Completes digestion and performs all nutrient absorption. Receives secretions form liver, gall bladder, and pancreas. Regions – divided into duodenum, jejunum, and ileum Length: 6-7 meters (about 20 ft) in a living person (add 10ft in a cadaver) Diameter: 2.5 - 4cm Figure 23.1 The Small Intestine Hepatopancreatic sphincter (of Oddi) – regulates the entrance of secretions from the liver, gall bladder and pancreas into the duodenum Figure 23.20 The Small Intestine Specializations for absorption: • Circular folds – large folds of the mucosa and submucosa that help slow food movement Figure 23.21a The Small Intestine Specializations for absorption: • Villi– finger-like projections of the mucosa that increase surface area of the epithelium. Each villus contains a capillary bed and a lacteal for nutrient absorption. • Intestinal crypts – invaginations producing intestinal juices, a mucous secretion Figure 23.21b The Small Intestine Specializations for absorption: • Microvilli – finger-like extensions of the epithelial cell membranes with attached “brush border enzymes,” further increasing surface area Figure 23.21b, c The Liver Liver – a 4-lobed gland whose digestive function is the production of bile Hepatitis – inflammation of the liver, usually resulting from viral infection Cirrhosis – chronic inflammation usually associated with alcohol abuse Bile – a green, alkaline fluid containing bilirubin pigment and bile salts that perform emulsification of fats. Drains from the liver via the hepatic ducts Figure 23.23a The Liver Emulsification – the physical breakdown of large fat globules into smaller fat droplets, thus increasing surface area for enzymatic digestion • bile salts are partially polar and partially nonpolar, thereby breaking up fat globules like a detergent Figure 23.35 The Gall Bladder Gall bladder - muscular sac on the posterior surface of the liver that stores and concentrates bile. The gall bladder is drained by the cystic duct Gall stones - crystallization of bile that accumulate in the gall bladder, may be passed naturally or removed via ultrasound, drugs, or surgery Figure 23.23b The Pancreas The Pancreas – gland whose acinar cells produces pancreatic juices containing digestive enzymes such as proteases, lipases, nucleases, and amylases. Figure 23.26 The Pancreas Pancreatic duct - drains pancreatic juices into the duodenum through the sphincter of Oddi Accessory duct – alternate pathway that drains directly Figure 23.20 Intestinal Hormones Intestinal hormones - chemicals released by enteroendocrine cells when chyme enters the duodenum • Cholecystokinin (CCK) - triggers secretions of bile from the gall bladder and relaxation of hepatopancreatic sphincter • Secretin – triggers liver to increase bile production Figure 23.25 Intestinal Hormones • Cholecystokinin (CCK) triggers release of pancreatic juices rich in enzymes • Secretin – triggers release of pancreatic juices rich in bicarbonate Figure 23.28 The Large Intestine Large Intestine (Colon) transports food from the small intestine to the anus while absorbing water and forming feces Ileocecal valve – regulates movement of food from the small to the large intestine Haustra – individual pouches of the large intestine wall Teniae coli – thin longitudinal muscle layer forming the haustra Figure 23.29a The Large Intestine Regions: • Cecum - pouch-like region with the hanging vermiform appendix • Ascending colon – transports food up the right side of the abdomen, turning at the hepatic flexure •Transverse colon – transports food across the abdomen, turning at the splenic flexure • Descending colon – transports food down the left side of the abdomen • Sigmoid colon – s-shaped region Figure 23.29a The Rectum and Anus Rectum – most distal region of the colon, where feces is stored until defecation Rectal valves – projections that allow gases to pass around feces Anus – end of the alimentary canal from which defecation occurs Internal anal sphincter – smooth muscle regulating anal opening External anal sphincter – skeletal muscle regulating anal opening Figure 23.29b The Defecation Reflex Defecation reflex – series of impulses that trigger release of feces 1. Sensory fibers sense stretch of rectum wall due to filling 2. Parasympathetic fibers trigger contraction of rectum wall and relaxation of internal anal sphincter 3. External anal sphincter can allow defecation, or voluntarily contract to temporarily stop the reflex Figure 23.32 Chemical Digestion Overview Figure 23.33a Chemical Digestion Overview Figure 23.33b