Burns
advertisement

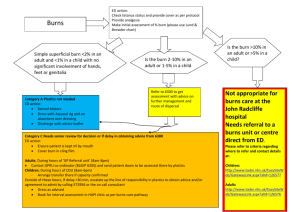
Burns Burns John van der Steeg MD Objectives Incidence and patterns of burn injury Pathophysiology of local and systemic responses to burn injury Classify burn Physical exam of the burned patient Prehospital management of burned patient Signs and symptoms of inhalational injury which may influence management Criteria for transport to a Burn Center Incidence and Pattern of Burn Types Tissue injury caused by thermal, electrical, radiation or chemical agents Burns are another form of trauma Associated with high mortality, lengthy rehabilitation. Greater than 2 million people/yr. seek care for burns. Morbidity and Mortality follow significant patterns regarding gender, age, and socioeconomic status Skin Largest body organ. Not a passive organ. – Protects underlying tissues from injury – Temperature regulation – Acts as water tight seal – Sensory organ Very young and old have thin skin thus short contact time = greater damage when compared to mid aged persons Skin concerns after burns Infection Problems with thermal regulation Inability to maintain normal water balance Skin layers Two layers – Epidermis – Dermis Epidermis – Outer cells are dead – Protective barrier and water tight seal – Deeper layers contain pigment to protect against UV radiation and produce stratum corneum Skin Layers Dermis – Consists of tough, elastic tissue which contains specialized structures such as hair follicles, sweat glands, blood vessels, oil glands, and nerve endings Classification of Burns First degree / superficial burnpainful, red, and dry and blanch with pressure. Classification of Burns 2nd degree / partial thickness burncharacterized by blisters, injury extends through the dermis to the epidermis, basal layers of skin are not destroyed Classification of Burns 3rd degree / full thickness burns- Entire thickness of dermis and epidermis is destroyed. Wound characterized by coagulatin necrosis and appears pearly white, charred or leathery. Sensation and cap refill are absent. Factors which affect Burn injury Water content Skin thickness Skin pigment Presence of absence of insulating substances Peripheral circulation Tissue damage depends on temperature and time Surface temperature of 44 C (111 F) begins to produce burns. But is dependent on exposure time. Temperature >44C and < 51C (124F) the rate of epidermal necrosis doubles with each degree of temperature increase. At > 70 C (185F) or greater, exposure time required to cause transepidermal necrosis is less than 1 second. Normal process of water evaporation is accelerated 5 to 15 time to that of normal skin. Pathophysiology of Burns (Local response) Based on Jackson’s thermal wound theory Zone of hyperemia – Increased blood flow due to normal inflammatory response Zone of stasis – Potentially viable tissue – Cells are ischemic due to clotting and vasoconstriction Zone of coagulation – Coagulation necrosis has occurred – Tissue is non viable Pathophysiology of Burns (Systemic response) Hypovolemic shock/”Burn shock” – Response proportional to extent of body surface injury Pulmonary response Gastrointestinal response Musculoskeletal response Neuroendocrine response Metabolic response Immune response Emotional response Burn injuries (Primary Survey) Recall that burn patients are first and foremost trauma patients Airway Breathing Circulation Disability Exposure Airway Airway control – Chin lift – Jaw thrust – Insert oral pharyngeal airway – Assess need for ET intubation Maintain in-line cervical immobilization in patients at risk Breathing Listen: verify breath sounds Assess rate and depth of respirations Administer high flow O2 Monitor chest wall excursion in presence of full thickness torso burns Inhalational injury Present in 10 – 20 % of burn patients Identified in 60 – 70 % of patients who die in burn centers Airway assessment and management Humidified 100% O2 by mask Endotracheal intubation indicated if – Airway obstruction imminent as signaled by progressive hoarseness and/or stridor – LOC is such that airway protective reflexes are impared Warning signs/clues Facial burns, singed nasal hairs Carbonaceous sputum Tachypnea, intercostal retractions Hoarsness Agitation (hypoxia) Rales, rhonchi, diminished breath sounds Inability to swallow Naso or oro-pharynx erythema Circulation Monitor BP, pulse rate, skin color Establish IV access – If possible, place iv in non-burned skin, but may place it in burned skin if needed. – How would you secure IV in burned tissue? Assess circulatory status of circumferentially burned extremities Disability, Neurologic Deficits Typically alert and oriented. If not, why not? Remember AVPU? – A-Alert – V-Responds to verbal stimuli – P-Responds to painful stimuli – U-Unresponsive Disability, Neurologic Deficits Please remember before you intubate, if possible, to get any pertinent history – AMPLE history – A – Allergies – M – Medications – P – Previous medical/surgical history – L – Last meal (time) – E – Events/environment surrounding the injury; ie. Exactly what happened Exposure/Environmental control First must remove patient to a safe area Stop the burning process – Exstinguish fire – cool smoldering areas – Remove ALL clothing and ALL jewelry – Cut around areas where clothing is stuck to the skin – Cool adherent substances (Tar, Plastic) Exposure/Environmental control Once patient in safe area Maintain patient’s temperature – Warm room or rig – Keep patient covered; dry sheets, blankets – Warm IV fluids Circumstances of Injury Circumstances of Injury: Flame How did it occur? – Inside or outside? – Clothing ignition? – Time to extinguish flame? – Extinguished how? – Gasoline or other fuel involved? – Explosion? Patient thrown? – Are purported circumstances of injury consistent with burn characteristics? Circumstances of Injury: Flame Structure fire? Smoke filled space? Others injured or killed in event? Was there LOC at the scene? How did the patient escape – Did the patient jump? How far was the drop? – Through glass? Circumstances of Injury: Flame Automobile crash? How badly was the car damaged? Other injuries? Did they hit anybody? Check around, under the vehicle. Car fire? Circumstances of Injury: Scald What is the history of the injury? – What was the liquid? – What was the volume of liquid involved? – What was the temperature of the liquid? If tap water, what was the heater temperature setting? If heated by other source, was the liquid boiling – – – – Was the patient wearing clothing? How quickly was it removed? Was the burned area cooled? Was other first aid administered? Circumstances of Injury: Scald Is abuse or neglect suspected? – How quickly was care sought? – Where did the burn occur? – Who was with the patient when the injury occurred? – Does the story fit the injury? Circumstances of Injury:Chemical Circumstances of Injury:Chemical What was the agent? Is it still around? Vapor?, Liquid?, Solid? How did the exposure occur? What was the duration of contact? What decontamination occurred? Was there an explosion? Was the patient thrown? What is the toxicity of the agent? Circumstances of Injury:Electrical What kind of current was involved? What was the duration of contact? Was the patient thrown or did the patient fall? What was the estimated voltage? Was there LOC? Was CPR administered? Circumstances of Injury:Electrical The great pretender – Small surface injuries may be associated with severe internal injuries – Causes about 1000 deaths/yr. First contact After patient in safe area… Complete head to toe exam Pre-existing medical conditions? Tetnus status? Other injuries? Determine Burn Severity You must assess % of body surface area (BSA) involved Depth of injury (1st, 2nd, or 3rd degree) – Realize that this is difficult to do as burns may “mature” over time AND getting an exact percentage is usually not possible Age of patient Associated / pre-existing disease or illness Burns to hands, face, genitalia. Extent of Burn Initial estimate of 2nd and 3rd degree burns: “rule of nines” – Adult areas = 9% BSA or multiples – Not accurate for infants/children due to larger BSA of head and smaller BSA of legs. To estimate scattered burns, palm of hands and fingers of patient = 1% BSA Burn Depth Very young and very old patients have thinner skin Therefore, contact time at similar temperatures will be worse for them. Pre-hospital management principles Stop the burning process Universal precautions Initiate fluid resusucitation per the consensus protocol: – – – – 2 - 4 ml % BSA burn ½ in 1st 8 hrs ½ over next 16 hrs *this is for adults only, pediatric patients require consensus formula + D5LR maintenence fluids Pre-hospital management principles Vital signs Assess extremity perfusion – * remove all rings, watches, other jewelry – *Elevation of burned areas if possible Ventilation status Pain relief/management Initial Burn Wound Care Thermal burns – Cover with clean, DRY cloth – NO ice or cold water soaks Initial Burn Wound Care Electrical Injury – Be aware of both cutaneous an internal injury Entrance and exit points versus contact points Arcing wounds vs electrical flash wounds – Consider electrical current cardiac effects Initial Burn Wound Care Chemical burns – Scene control – Brush powders from skin and clothes Watch shoes and socks – Remove contaminated clothing – Flush with COPIUS amounts of water – Eye irrigation if involved – Exposure protection for yourselves and anyone involved with patient care Burn center referral criteria The ABA identifies the following as injuries requiring a Burn Center referral: – 2nd degree burns > 10% TBSA – Burns to face, hands, feet, genitalia, perineum, major Joints – 3rd degree burns – Electric injury (lightning included) – Chemical burns Burn center referral criteria Inhalational injuries Burns accompanied by pre – existing medical conditions Burns accompanied by trauma, where burn injury poses greatest risk of morbidity or mortality Burns to children in hospitals without pediatric services Patients with special social, emotional or rehabilitative needs Summary Be able to assess injuries Be able to develop priority – based plan of care Base care plan on type, extent, degree of burn Consult with a burn center physician Decide upon local treatment and transport with burn center physician Feel that burn…in your colon