Practical-6
advertisement
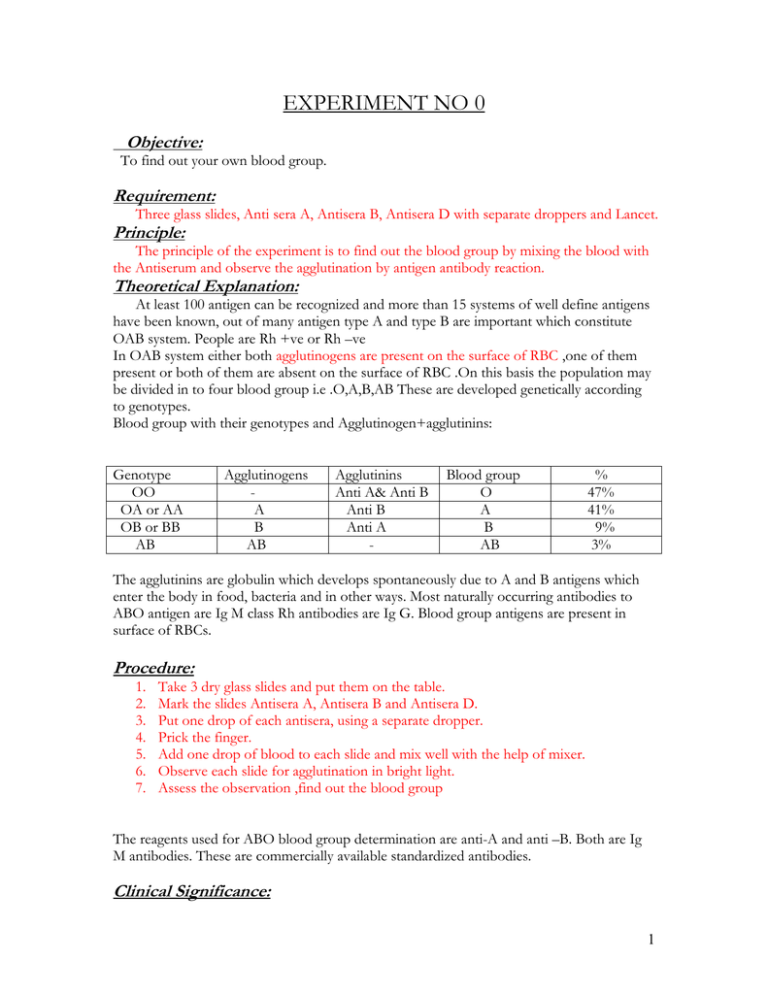
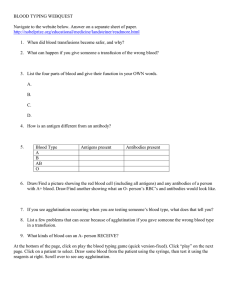
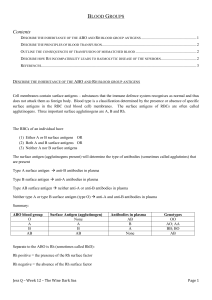
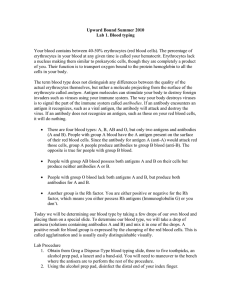
EXPERIMENT NO 0 Objective: To find out your own blood group. Requirement: Three glass slides, Anti sera A, Antisera B, Antisera D with separate droppers and Lancet. Principle: The principle of the experiment is to find out the blood group by mixing the blood with the Antiserum and observe the agglutination by antigen antibody reaction. Theoretical Explanation: At least 100 antigen can be recognized and more than 15 systems of well define antigens have been known, out of many antigen type A and type B are important which constitute OAB system. People are Rh +ve or Rh –ve In OAB system either both agglutinogens are present on the surface of RBC ,one of them present or both of them are absent on the surface of RBC .On this basis the population may be divided in to four blood group i.e .O,A,B,AB These are developed genetically according to genotypes. Blood group with their genotypes and Agglutinogen+agglutinins: Genotype OO OA or AA OB or BB AB Agglutinogens A B AB Agglutinins Anti A& Anti B Anti B Anti A - Blood group O A B AB % 47% 41% 9% 3% The agglutinins are globulin which develops spontaneously due to A and B antigens which enter the body in food, bacteria and in other ways. Most naturally occurring antibodies to ABO antigen are Ig M class Rh antibodies are Ig G. Blood group antigens are present in surface of RBCs. Procedure: 1. 2. 3. 4. 5. 6. 7. Take 3 dry glass slides and put them on the table. Mark the slides Antisera A, Antisera B and Antisera D. Put one drop of each antisera, using a separate dropper. Prick the finger. Add one drop of blood to each slide and mix well with the help of mixer. Observe each slide for agglutination in bright light. Assess the observation ,find out the blood group The reagents used for ABO blood group determination are anti-A and anti –B. Both are Ig M antibodies. These are commercially available standardized antibodies. Clinical Significance: 1 When blood transfusion is necessary, the blood typing of the recipient and the donor should be done very carefully, to avoid hazards of blood transfusion. The mismatched blood transfusion result in to hemolytic jaundice and transfusion reaction associated with hemolysis, haemoglobinurea and severe type of anemia. Erythroblastosis Fetalis is a hemolytic disease of new born characterized by progressive agglutination and subsequent phagocytosiss of RBC .If father is Rh+ve, mother is Rh –ve and child has inherited Rh +ve antigen from father. The mother develops Anti Rh antibodies that diffuse through placenta in to the fetus to cause RBC agglutination. Prevalence of disease Rh –ve mother having her first Rh +ve child does not does not develop this disease but 3% of second and10% of third baby develop erythroblastosis fetalis and they are born with severe anemia in which many blast forms appear in circulation. The incidence rises progressively with subsequent pregnancies. Hemolytic transfusion reactions occur mainly due to ABO and Rh system. Observation chart: Antisera Antisera A &1 drop of blood Antisera B & 1dop Antisera D& 1 of blood drop of blood Agglutination Agglutination = +ve No agglutination= -ve Result: My blood group is =__________ The Rh +ve person has Rh antigen but no antibodies. Rh –ve person neither Rh antigens nor antibodies. Rh antibodies do never develop spontaneously until and unless Rh –ve person is exposed to Rh antigen. ABO and Rh blood group are of main importance in routine use. Some other blood group include MNS ,P, Kell ,Duffy ,Kids, Lewis etc and a very important Rh group. Precautions: 1. 2. 3. 4. Slides should be washed and dried carefully. Separate dropper should be used for each antisera. The blood drop should not be touched to antisera. A separate mixer should be used for mixing. 2