MOTOR NEURON DISEASE
advertisement

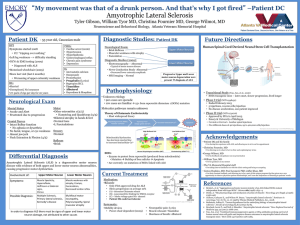
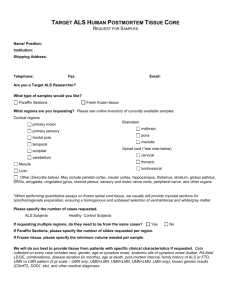
MOTOR NEURON DISEASE Definition Motor Neuron Diseases group of diseases which include progressive degeneration and loss of motor neurons with or without similar lesion of the motor nuclei of the brain replacement of lost cells with gliosis ALS Demographics Incidence 2 per 100,000 Male slightly > Female Peak age of onset: 6th decade (range 20 to 90) No racial predilection 95% sporadic 5% hereditary classification UMN: Primary Lateral Sclerosis (PLS) Familial Spastic Paraparesis LMN: Spinal Muscular Atrophy (SMA) Progressive Muscular Atrophy UMN and LMN: Amyotrophic Lateral Sclerosis (ALS) cause No know cause Possible cause could be Defective glutamate metabolism Free radical injury Mitochondrial dysfunction Gene defects Programmed cell death (apoptosis) Cytoskeletal protein defects Autoimmune dysfunction/ Inflammatory Damage Protein aggregation Virus Amyotrophic Lateral Sclerosis originally described by Charcot and thus it is often called Charcot's disease in Europe. Classical ALS is a distinct syndrome characterized by a combination of UMN and LMN signs and symptoms Clinical features (65% cases)affects the hands first fasciculation is seen on examination wasting of the muscles and paralysis of movement. Weakness of the muscles of the chest wall and diaphragm leads to difficulty in breathing. muscles controlling facial expression, the tongue, the palate ability to cough effectively and clear secretions is lost. Diagnostic Triad: ALS Upper motor neuron Progression Lower motor neuron ALS: Prognosis Prognosis 50% dead in 3 years 20% live 5 years 10% live 10 years Worse prognosis if: Bulbar onset Simultaneous arm/leg onset Older age at diagnosis (onset < 40: 8.2 yr duration, onset 61-70: 2.6 yr duration) medication Riluzole, a drug given orally may have some effect in slowing the progression of the disease Symtomatic treatment Baclofen, dantrolene, diazepam, gabapentin to relieve muscle stiffness and cramps Analgesics – paracetamol, Hyoscine, atropine to reduce salivation Antidepressants e.g. amitriptiline, fluoxetine to alleviate symptoms of anxiety, depression and emotional lability Benzodiazepines e.g. diazepam to reduce anxiety Opiates e.g. morphine, fentanyl, oxycodone to control pain, treat breathlessness, choking attacks and reduce anxiety ASSESSMENT Subjective assessment: Course of the disease Social history and support network Lifestyle Expectations Objective assessment: Level of consciousness and orientation Basic ability to communicate Motor ability Co-ordination Respiratory system Swallow Function Equipment and environment Bladder and bowel function Mood Pain Outcome Measurement Modified fatigue impact scale Berg balance scale Elderly Mobility Score Timed walk Timed Unsupported Steady Stand Ashworth scale intervention The overall goals of intervention will vary as the condition progresses. Early stage - to optimise remaining function Middle stage - to maintain functional mobility Late stage - to maximise quality of life Early stage Preserving optimum level of mobility Active range of movement exercises Strengthening exercises Aerobic activities Training in pacing activity/fatigue management Stretching of affected joints Teaching breathing exercises Provision of appropriate equipment and assistive devices to support weak muscles. Provision of appropriate walking aids Middle stage The patient may remain ambulatory but have severe weakness in certain muscle groups provision of adaptive equipment (e.g. Ankle Foot Orthosis, splints, arm slings/trays, and wheelchair. access to equipment, provision of walking aids (Advice on footwear) management of oedematous limbs soft collar provision active, assisted active, passive and /or aerobic exercise, as appropriate teaching breathing exercises and assisted coughing advice regarding pressure care and provision of pressure relieving seating/mattress management of spasticity. prevention of contractures position for comfort Late stage The patient uses a wheelchair when out of bed or remains in bed teaching carers to perform gentle passive stretches, heat treatment and/or massage to relieve pain and improve comfort advising carers regarding positioning and movement of the patient in bed modified postural drainage to decrease retention of secretions, self-assisted or carer-assisted coughing and airway clearance techniques may need to be taught. A suction machine maybe required at this stage. Carers may be shown how to use suction to keep the patient's mouth clear of secretions but only experienced health professionals should attempt deep suction,