MOTOR NEURON DISEASE
advertisement

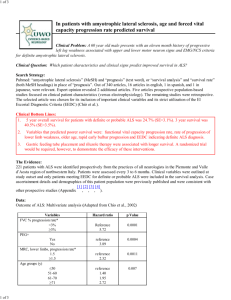
Motor neuron disease Motor Neuron Diseases The motor neuron diseases (MNDs) are a group of progressive neurological disorders that destroy cells that control essential muscle activity such as speaking, walking, breathing, and swallowing. ALS Demographics Incidence 2 per 100,000 Male slightlymorethan Female Peak age of onset: 6th decade (range 20 to 90) Classification of Motor neuron disease UMN: Primary Lateral Sclerosis (PLS) LMN: Spinal Muscular Atrophy (SMA) Progressive Muscular Atrophy UMN and LMN: Amyotrophic Lateral Sclerosis (ALS) cause No known cause Possible cause could be Mitochondrial dysfunction Gene defects Cytoskeletal protein defects Autoimmune dysfunction/ Inflammatory Damage Virus Amyotrophic Lateral Sclerosis (ALS) originally described by Charcot and thus it is often called Charcot's disease in Europe. Classical Amyotrophic Lateral Sclerosis (ALS) is a distinct syndrome characterized by a combination of Upper motor neuron (UMN) and Lower motor neuron (LMN) signs and symptoms Clinical features (65% cases)affects the hands first fasciculation is seen on examination Clinical features wasting of the muscles and paralysis of movement. Weakness of the muscles of the chest wall and diaphragm leads to difficulty in breathing. Clinical features Weakness of muscles controlling facial expression, the tongue, the palate ability to cough effectively and clear secretions is lost. ALS: Prognosis Poor prognosis if: Bulbar onset Older age at diagnosis ASSESSMENT Level of consciousness and orientation Basic ability to communicate Motor ability Co-ordination Respiratory system Swallow Function Equipment and environment Bladder and bowel function Mood Pain Goals of Physical Therapy Management The overall goals of intervention will vary as the condition progresses. Early stage - to optimise remaining function Middle stage - to maintain functional mobility Late stage - to maximise quality of life Early stage Preserving optimum level of mobility Active range of movement exercises Strengthening exercises Aerobic activities Training in pacing activity/fatigue management Stretching of affected joints Teaching breathing exercises Provision of appropriate equipment and assistive devices to support weak muscles. Provision of appropriate walking aids Middle stage The patient may remain ambulatory but have severe weakness in certain muscle groups provision of adaptive equipment (e.g. Ankle Foot Orthosis, splints, arm slings/trays, and wheelchair. access to equipment, provision of walking aids (Advice on footwear) management of oedematous limbs Middle stage soft collar provision active, assisted active, passive and /or aerobic exercise, as appropriate Middle stage teaching breathing exercises and assisted coughing advice regarding pressure care and provision of pressure relieving seating/mattress management of spasticity. prevention of contractures position for comfort Late stage The patient uses a wheelchair when out of bed or remains in bed teaching carers to perform gentle passive stretches, heat treatment and/or massage to relieve pain and improve comfort advising carers regarding positioning and movement of the patient in bed modified postural drainage to decrease retention of secretions, self-assisted or carer-assisted coughing and airway clearance techniques may need to be taught.