Respiratory Disorders
advertisement

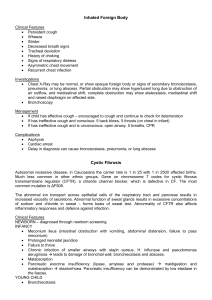
Chapter 5 NURSING CARE OF THE CLIENT WITH RESPIRATORY DISORDERS Dr. J.C.Helen Shaji Ph.D Structure of Respiratory System Respiratory System Its primary function is delivery of oxygen to the lungs and removal of carbon dioxide from the lungs. Thoracic Cavity The inside of the chest cage is called the thoracic cavity. Contained within the thoracic cavity are the lungs, cone-shaped, porous organs encased in the pleura, a thin, transparent double-layered serous membrane lining the thoracic cavity. The Physiology of the Lungs The right lung is larger than the left and is divided into three sections or lobes: upper, middle, and lower. The left lung is divided into two lobes: upper and lower. The upper portion of the lungs is the apex; the lower portion is the base. Conducting Airways The conducting airways are tubelike structures that provide a passageway for air as it travels to the lungs. The conducting airways include the nasal passages, mouth, pharynx, larynx, trachea, bronchi, and bronchioles. Anatomy and physiology of respiratory system Upper Nose Paranasal sinuses Pharynx Larynx Trachea Lower lung Pleura Mediastinum Lobes Bronchial and bronchioles Alveoli Pharynx Larynx Trachea The conducting airways that connect nasal passages and mouth to the lower parts of the respiratory tract. The passageway for air entering and leaving the trachea and containing the vocal cords. Commonly known as the windpipe, this tube is composed of connective tissue mucosa and smooth muscle supported by C-shaped rings of cartilage. Bronchi, Bronchioles Two tubes, the right and left primary bronchi, that each pass into its respective lung. Within the lungs, the bronchi branch off into increasingly smaller diameter tubes until they become the terminal bronchioles. Respiration A process of gas exchange necessary to supply cells with oxygen for carrying on metabolism, and to remove carbon dioxide produced as a waste by-product. Two types of respiration: external and internal. External & Internal Respiration The exchange of gases between the inhaled air and the blood in the pulmonary capillaries. The exchange of gases at the cellular level between tissue cells and blood in systemic capillaries. Signs & Symptoms 1. 2. 3. 4. 5. 6. Dyspnea Cough Sputum Production Chest Pain Wheezing Haemoptysis Sign and symptoms Cough Result from irritation of mucus membrane Protect from accumulation of secretion in bronchi and bronchiole Types Dry cough URTI of viral infection High pitched cough larngotrachiites Brassy cough tracheal lesion Cough at night indicate lt HF or asthma Cough at morning with sputum production indicate bronchitis Cough after food intake indicate aspiration Color change indicate bacterial infection Assessment Health History (allergies, occupation, lifestyle, health habits) Inspection (client's color, level of consciousness, emotional state) (Rate, depth, quality, rhythm, effort relating to respiration) Palpation and Percussion Auscultation (Listening for Normal and Adventitious Breath Sounds) Adventitious Breath Sounds Abnormal sounds and some conditions associated with them: Fine crackles (dry, highpitched popping…COPD, CHF, pneumonia) Coarse crackles (moist, low-pitched gurgling…pneumonia, edema, bronchitis) Sonorous wheezes (lowpitched snoring…asthma, bronchitis, tumor) Sibilant wheezes (highpitched, musical … asthma, bronchitis, emphysema, tumor) Pleural friction rub (creaking, grating… pleurisy, tuberculosis, abscess, pneumonia) Stridor (crowing…croup, foreign body obstruction, large airway tumor). Common Diagnostic Tests for Respiratory Disorders 1. 2. 3. Laboratory Tests (Hemoglobin; Arterial blood gases; Pulmonary Function Tests; “Sputum Analysis& culture”). Radiologic Studies (Chest X-ray; Ventilationperfusion scan; CAT scan; Pulmonary angiography). Other (Pulse oximetry; Bronchoscopy; Thoracentesis; MRI). Respiratory Care Modilities Oxygen Therapy The administration of Oxygen in concentration greater than that found in environmental atmosphere Indications -change in respiratory rate - hypoxemia - hypoxia Oxygen Therapy 1. 2. 3. 4. Cautions Oxygen toxicity Suppression of ventilation Source of Cross infection Fire Danger Method of Oxygen Administration slide Chest Physiotherapy The Goal of chest physiotherapy is : 1. Remove bronchial secretion Improve Ventilation Increase efficiency of respiratory muscles Postural Drainage Chest Percussion &vibration Breathing exercise &retraining 2. 3. Air Way Management 1. 2. 3. 4. Emergency management of upper airway obstruction Causes foreign body Secretions Vomiting or food particles Enlarged tissue “edema, Ca, &abscesses” Assessment Inspection , palpation,& Auscultation Airway Management 1. 2. 3. 4. 5. Emergency Measures Opening airway by extend Pt neck back Observe airway Cross finger to clear airway If no passage “Abd thrust” Use resuscitation bag (AMBU bag) Endotracheal Intubation Passing endotracheal tube through mouth or nose into the trachea It is a method of choice in emergency Providing airway for specific patients For mechanical ventilation Tracheostomy It is a procedure in which an opening is made into the trachea and indwelling tube is inserted into the trachea Indications To bypass an upper airway obstruction 2. To allow removal of tracheobroncheal secretions 3. For long term ventilation 4. To prevent aspiration Complications “bleeding, pneumonia, air embolism emphysema , pneumothrax 1. Upper Respiratory Tract Infections/Inflammatory Disorders Rhinitis (coryza, common cold) Allergic rhinitis Sinusitis Pharyngitis Tonsillitis Laryngitis Upper Respiratory Tract Infections/Inflammatory Disorders Are the common conditions that affect most people on occasion, some infections are acute and other are chronic common cold Often is used when referring to a symptoms of an upper respiratory tract infection ch.bi nasal congestion ,sore throat , & cough Cold referred to a febrile, infectious, acute inflammation of the mucus membranes of the nasal cavity common cold 1. 2. 3. 4. 5. Clinical manifestations Nasal congestion Scratchy or sore throat Sneezing & cough Headache & muscle ache Herpes simplex sore (cold sore ) common cold Medical Management (symptomatic management) 1. Fluid intake ,rest ,prevention of chills. Aqueous decongestant,anti histamin, Vit. C. Expectorant as needed Analgesics for aches ,pain , & fever. Antimicrobial to reduce incidence of complications 2. 3. 4. 5. Nursing Management 1. Patient teaching of self care & prevention of infection & break chain of infection Rhinitis Inflammation of nose by viral , obstructive ,allergic reaction. Clinical manifestations 1. Rhinorrhea “ excessive nasal drainage” Nasal congestion, Itching ,& sneezing Headache may occur 2. 3. Rhinitis 1. 2. 3. 4. Medical Management Treatment of cause “antibiotics” Decongestant agents Antihistamine In severe cases corticosteroids Acute Sinusitis 1. 2. 3. It is inflammation of sinuses , it is resolved promptly if their opening into nasal cavity . Clinical Manifestations Pressure , pain over the sinus area Tenderness Purulent nasal secretions Acute Sinusitis Medical Management 1. 3. Antimicrobial agent “Amoxicillin” Oral & Topical Decongestant Heated mist or Saline irrigation Nursing management 2. “Teaching patient self care” Promote drainage (steam inhalation ) Increase fluid intake Apply local heat Acute Sinusitis 1. 2. 3. Complications Meningitis &osteomylitis Brain abscess Ischemic infarction Chronic Sinusitis 1. 2. 3. 4. It is an inflammation of sinuses that persists for more than 8 weeks in adult & or 2 weeks in children Clinical Manifestations Impaired mucociliary clearness & ventilation Chronic hoarseness & cough Chronic Headache Facial pain Chronic Sinusitis Medical Management 1. 2. Strong antibiotics (for 21 days ) Surgical intervention to remove obstruction cause that cause block of drainage passage (FESS) Nursing Management 1. Increase humidity Increase fluid intake Early signs of sinusitis 2. 3. PHARYNGITIS Acute Pharyngitis 1. 2. 3. 4. 5. It is a febrile inflammation of throat ,caused by virus about 70% , uncomplicated viral infection usually subsided promptly within 3-10 days Clinical Manifestations Fiery red pharyngeal membrane& tonsils Lymphoid follicles that are swollen Enlarge tender cervical lymph node Fever & malaise Sore throat , hoarseness,& cough Acute Pharyngitis Medical Management 1. Supportive measures for viral infection Pharmacologic therapy antibiotics for 10 days “cephalosporin”analgesic for severe sore anti tussive medications Nutritional therapy liquid or soft diet “If liquid can’t tolerated IV fluid administered “ Nursing Management (bed rest ,skin assessment, mouth care &normal saline gargle & self care teaching 2. 3. 4. Chronic Pharyngitis 1. 2. 3. Causes:Common in adults who work or live in dusty surrounding ,use the voice too excess , suffer from chronic cough , & habitually use alcohol & tobacco Types of pharyngitis Hypertrophic : ch.by general thickening& congestion of pharyngeal mucus membrane Atrophic : probably late stage of first type Chronic Granular : ch.by numerous swollen lymph follicles on the pharyngeal wall Chronic Pharyngitis Clinical Manifestations 1. 3. Constant sense of irritation or fullness in throat Mucus expelled by coughing Difficulty in swallowing Medical Management 1. Relieving symptoms Avoiding exposure to irritant Correct respiratory & cardiac conditions 2. Chronic Pharyngitis 2. Antihistamine drugs 3. Decongestant 4. Controlling malaise Nursing Management 1. Patient teaching of self care Avoid alcohol , tobacco , exposure to cold Face mask to avoid pollutant Warm fluids,&warm saline gargle 2. 3. 4. TONSILLITIS Tonsillitis The tonsils are composed of lymphatic tissue & situated on each side of the oropharynx ,they frequently are the site of acute infection (tonsillitis) Clinical Manifestations Tonsils : sore throat, fever , snoring & difficulty of swallowing Adenoids : ear ache , mouth breathing , drainage ear ,frequent cold , bronchitis, noisy respiration, foul smelling breath &voice impairment Tonsillitis Medical Management 1. 3. For recurrent tonsillitis “tonsillectomy” Conservative or symptomatic therapy Antimicrobial therapy “penicillin” for 7 days Nursing Management 1. Provide post op. care : hemorrhage , position head turned to side, water or ice chips Teaching patient :S&S of hemorrhage Avoid too much talking or coughing Liquid or semi liquid diet for several days Alkaline mouth washing with warm saline 2. 2. 3. 4. 5. Laryngitis It is an inflammation of larynx ,often occur as a result of voice abuse or exposure to dust , chemicals , smoke , & other pollutants Common in winter & easily transmitted The cause of infection is almost virus Clinical Manifestations 1. Hoarseness or aphonia Severe cough 2. Laryngitis Medical Management 1. Resting voice & avoid smoking Inhale cool steam or an aerosol Conservative treatment Antibiotics for bacterial organisms Nursing Management Rest voice Maintain a well humidified environment Daily fluid intake 2. 3. 4. 1. 2. 3. Lower respiratory tract infections Lower Respiratory tract infections Bronchitis Bronchiolitis Tracheobronchitis Pneumonia Pulmonary Tuberculosis Pleurisy/Pleural Effusion Pleurisy is a painful condition that arises from inflammation of the pleura, or sac that encases the lung. Pleural effusion occurs when the inflamed pleura secretes increased amounts of pleural fluid into the pleural cavity. Atelectasis 1. 2. 3. 4. 5. Collapse or airless condition of the alveoli caused byhypoventilation,obstruction of airway or compression Clinical Manifestations Cough & sputum production Dyspnea ,tachypnea ,tachycardia Signs of pulmonary infection may present Fever Central cyanosis Atelectasis 1. 2. 3. 4. 5. Management First line measures :(turning , early ambulation , lung volume expansion , coughing, spirometry ,breathing exercises If there is no response : (PEEP , IPPB) Bronchoscopy Postural Drainage & percussion If cause is compression remove the cause Acute Tracheobronchitis An inflammation of the mucus membrane of the trachea & the bronchial tree , often follow upper respiratory tract infection Clinical Manifestations 1. Dry irritating cough “expectorate sputum” Sternal soreness from coughing Fever ,stress , night sweating Headache & general malaise As the infection progress the patient develop (shortness of breath, noisy breath ,&purulent sputum 2. 3. 4. 5. Acute Tracheobronchitis Medical Management 1. 5. Antibiotics depend on symptoms & culture Expectorant may be prescribed Increase fluid intake Rest & cool therapy Suctioning & Bronchoscopy Nursing Management 1. Patient teaching Encourage fluid intake Coughing exercises to remove secretions Complete antibiotics course, Prevent over exertion 2. 3. 4. 2. 3. 4. 5. Pneumonia An inflammation of the lung tissue that is caused by microbial agent Community Acquired Pneumonia (CAP) 1. Occurs either in community setting or within the first 48 hrs of hospitalization Most common in people younger than 60 yrs Most prevalent during winter & spring Caused by pneumococcus & H influenza Virus the cause in infants & children 2. 3. 4. 5. Pneumonia Hospital Acquired Pneumonia (HAP) the onset of pneumonia symptoms more than 48 hrs after admission to hospital. Also called nosocomial infection Common organism E.coli ,Klebsiella ,S.aurious It occurs when host defense impaired in certain conditions Pneumonia in the Immuno compressed host Caused by organisms also observed in CAP,HAP. Has subtle onset with progressive dyspnea , fever , &productive cough Streptococcus pneumoniae Types of Pneumonia Lobar pneumonia all or a large segment of one or more pulmonary lobes is involved. Bronchopneumonia begins in the terminal bronchioles which become clogged with mucopurulent exudates to form consolidated patches in nearby lobules. Interstitial pneumonia the inflammatory process in the alveolar walls and per bronchial Pathological changes Exudates consolidate material replaces air in the lung so the density of the lung increases, and leads to increase sound heard on auscultation & dullness of the lung area on percussion. Pneumonia Clinical Manifestations 1. Sudden onset of shaking chills Rapidly increase in body temperature 38-40 C Chest pluretic pain increased by deep breathing Patient looks severely ill with marked tachypnea Shortness of breath Orthopnea Poor appetite Diaphoresis &tires easily Purulent sputum 2. 3. 4. 5. 6. 7. 8. 9. Chest X-ray finding in Pneumonia Pneumonia Medical Management 1. Appropriate antibiotics depend on culture result Hydration (increase fluid intake ) Antipyretic for fever & Headache Warm moist inhalation to relieve irritation Antihistamine to relieve sneezing & rhinorrhea Oxygen & respiratory supportive measures Complications : Shock & respiratory failure , Atelectasis & plural effusion Super infection 2. 3. 4. 5. 6. Chronic Obstructive pulmonary Disease (COPD) Disease state in which air flow is obstructed by emphysema or chronic bronchitis or both The airway obstruction is usually progressive & irreversible Clinical Manifestations 1. Cough Increase work of breathing Severe dyspnea that interfere with patient activity 2. 3. COPD – Risk factors Exposure to tobacco Passive smoking Occupational exposure Air pollution Pathophysiology The inflammatory response of the lungs to noxious particles or gases. Bcoz of the Ch.inflammation body attempts to repair it. Narrowing occurs in the small peripheral airways Overtime this injury and repair process causes scar tissue formation which leads to narrowing of the small peripheral airways. Chronic Obstructive pulmonary Disease (COPD) Medical Management Inhaled bronchodilators to improve airway 2. Oxygen therapy as prescribed 3. Pulmonary rehabilitation emotional & physiologic needs ,breathing exercises ,&methods of symptoms elevation Complications:1. Respiratory insufficiency 2. Respiratory failure 1. Chronic Obstructive pulmonary Disease (COPD) Nursing Management Patient Education About COPD Breathing exercise Inspiratory muscles training Self care activity Coping measures 1. 2. 3. 4. 1. 2. 3. 4. Complications Pneumonia Atelectasis Pneumothrax Respiratory insufficiency & failure Chronic Bronchitis 1. 2. It is a productive cough that lasts in each of 3 months in 2 consecutive years in a patient whom other causes of cough is excluded. Clinical Manifestations Chronic productive cough in winter Increase frequency of respiratory infection Bronchitis Chronic Bronchitis 1. 2. 3. 4. 5. 6. Medical Management the objective of treatment are to keep the bronchioles opened & functioning Antibiotics therapy for recurrent infection Bronchodilators to remove secretion Postural Drainage & chest percussion Hydration & fluid intake Corticosteroid may be used Smoker patient should stop smoking Emphysema A complex and destructive lung disease wherein abnormal distension of the air spaces beyond the terminal bronchioles, with destruction of alveoli. Smoking is the major cause of Emphysema Classification 1. Panlobular : destruction of the respiratory bronchiole,aleveolar duct &alveoli Centrilobular : pathogenic changes take place mainly in the center of secondary lobule 2. Emphysema 1. 2. 3. 4. 5. 6. Clinical Manifestations Increase dyspnea on exertion Annoroxia & Weight loss Weakness & Inactivity Pursed –lip- breathing Increase cough, wheezing, purulent sputum & occasionally fever Barrel chest Emphysema 1. 2. 3. 4. 5. 6. Medical Management Bronchodilators Antimicrobial Agents Oxygen therapy Pulmonary rehabilitation Smoking cessation corticosteroids Emphysema Surgical management Bullectomy:-Removal of bullae in the lung Bullae are enlarged air spaces that do not contribute ventilation but occupy the space in thorax. Lung volume reduction surgery Lung transplantation Bronchiectasis A chronic dilation of the bronchi. Main causes of this disorder are pulmonary TB infection, chronic upper respiratory tract infections, and complications of other respiratory disorders of childhood, particularly cystic fibrosis. Asthma A condition characterized by intermittent airway obstruction in response to a variety of stimuli. “inflammatory” Asthma differ from COPD in that it is reversible process either spontaneously or with treatment Allergy is the strongest predisposing factor for the development of asthma Asthma 1. 2. Clinical Manifestations The most three common symptoms are: a- cough b- dyspnea c- wheezing Hypoxemia may occur along with a- cyanosis b- diaphoresis c- tachycardia d- widened pulse pressure Asthma 1. 2. 3. 4. Prevention : allergic test to identify the substances cause the symptoms and avoid it as possible Complications Status Asthmaticus (Severe and persistant asthma longer than 24 hours) Rib fracture Pneumonia Atelectasis Medical management of Asthma 1. 2. 3. 4. 5. 6. Pharmacologic Therapy (long term) Corticosteroid :Inj.Dexamethasone sodium. Most effective anti inflammatory medication (inhaled form) Mast cell stabilizers:- eg. Cromolyn sodium Long-acting beta2adrenergic agonist mild to moderate bronchodilator (Tab. Salbutamol) Xanthine derivatives:- Inj.Aminophylline, Theophylline Quick relive medications (short acting beta2 adrenergic agonists – Inj. Albuterol Peak flow monitoring Asthma 1. 2. 3. 4. 5. 6. Nursing Management Immediate care based on severity of symptoms Assessment & Allergic History Administer medication & observe patient response Antibiotics as prescribed for infection Assist in intubations procedure if needed Psychological support for patient & his family Health Education for COPD Breathing and coughing exercises Pursed lip breathing Activity pacing Nutritional therapy Nursing Diagnosis Impaired gas exchange R/T ch.inhalation of toxins. Ineffective airway clearance R/T bronchial constriction, increased mucous production Ineffective breathing pattern R/T shortness of breath Self care deficit R/T fatigue Activity intolerance R/T ineffective breathing pattern Deficient knowledge R/T home health care TUBERCULOSIS Tuberculosis is an infectious disease primarily affect the lung parenchyma which is caused by Mycobacterium tuberculosis. Causative organism: Mycobacterium tuberculosis. Mode of transmission: - Droplet infection (inhalation) or - By direct contact with infected person. Pathophysiology Primary infection: It occurs when the causative organism enters the lung tissue _____ the invaded tissue react by inflammation & calcification (later on) = primary focus which heals spontaneously if the patient's resistance is good. The primary complex includes the initial lesion & lesions in the the regional lymph nodes. Pathophysiology contin…. The disease process may spread to other parts inside the lung & to the GIT because of swallowed infected sputum. NB: when wide spread infection occurs, the patient is said to have miliary tuberculosis. Later because of lowered resistance, the latent lesion may again become active. Tuberculosis Chest X-ray film. Presence of numerous miliary opacities to middle and upper field of right and to middle and lower field of left. Pathophysiology contin… Secondary infection: Secondary infection may include extensive inflammatory reaction with tissue destruction & cavitations healing by means of scar or fibrosis. Clinical manifestations Low grade fever Cough Night sweating Fatigue Weight loss Haemoptysis Diagnostic evaluation: - Mantoux test = skin test is the most important test to diagnose TB. - About 6 weeks after infection an antigen = ماده تؤدي إلى مولد المضاد (تفاعل المضاد معهاPurified Protein Derivative) is injected intradermaly. The presence of allergy or hypersensitivity to tuberculo-protein is observed within 48 to 72 hrs and then interpreted in relation to induration not erythema (redness) in centimeters. Contin--Interpretation: - A reaction of less than 5cm in diameter is considered –ve. - Induration of 5 to 9cm is considered doubtful and should be repeated. - A lesion of 10cm or more is considered +ve. . Other diagnostic tests include chest x-ray & sputum culture Mantoux test Medical management First – line management:INH, Rifampicin, Pyrizinamide, Ethambutol or Inj.Streptomycin. This will be continued for 8 weeks. Pyrizinamide and Rifampicine will be continued another 4 months. Vit B will be given with INH to prevent INH induced peripheral neuropathy. Ethionamide and capreomycine are second – line medications. Nursing interventions Promoting airway clearance Advocating adherence to treatment regimen Promoting activity and adequate nutrition Monitoring and managing potential complications Health education on prevention of spread of infection.(Sputum disposal) Prevention of TB Prevention: 3 methods for effective prevention: 1. Isolation of infected cases. 2. Immunization with B.C.G. 3. Prophylactic treatment using INH. For infants & children who must live a household with an infectious adult. Acute Respiratory Failure Conditions wherein there is a failure of the respiratory system as a whole. It is a sudden & life threatening deterioration of gas exchange function of the lung Acute : a fall in arterial PaO2 to less than 50mmHg &a rise in arterial PaCo2to greater than 50mmHg Acute Respiratory Failure 1. 2. 3. 4. Causes Decrease respiratory derive “brain” Dysfunction of chest wall “nerves & muscles” Dysfunction of lung parenchyma “expansion” Postoperative & inadequate ventilation Acute Respiratory Failure 1. 2. 3. 4. 5. 6. 7. Clinical Manifestations Impaired oxygenation & may be include restlessness Fatigue & headache Dyspnea & air hunger Tachycardia &hypertension Confusion & lethargy Diaphoresis …… Respiratory Arrest Uses of accessory muscles Acute Respiratory Failure Medical management: Intubations and mechanical ventilation may be required to maintain adequate ventilation and oxygenation Acute Respiratory Failure 1. 2. 3. 4. 5. Nursing management: Monitoring patient responses and arterial blood gases Monitoring vital sign turning ,mouth car , skin care , and rang of motion . Teaching about the underlying disorders Assists in intubations procedure Pulmonary Embolism Obstruction of a pulmonary artery by a bloodborne substance. Causes: Deep vein thrombus, immobility, congestive heart failure, hematological disorders. Intravenous infusions and Thrombophlebitis Fat from long bone fractures. Deep vein thrombosis is a common cause of pulmonary embolism. Other types (Air , Fat , Septic ) Pulmonary Embolism 1. 2. 3. 4. Clinical Manifestations Dyspnea & Tachypnea Sudden & pluretic chest pain Fever & cough & hemoptysis Apprehension Diaphoresis & syncope Pulmonary Embolism 1. i. ii. iii. iv. v. vi. Medical Management Emergency Management Nasal O2 IV infusion for Medication Perfusion Scan ABGs &ECG Small dose of Morphine Intubation & mechanical Ventilation Pulmonary Embolism Pharmacologic Management i. Anticoagulant therapy heparin 5000-10000 bolus then 18u/kg body wt Tab. warfarin for three months ii. Thrombolytic therapy (Streptokinase therapy, Actylase (TPA)) iii. Surgical Management (Surgical Embolectomy) Pulmonary Embolism 1. 2. 3. 4. 5. 6. Nursing Management Preventing thrombus formation Monitoring thrombolytic therapy Providing post operative nursing care Managing O2 therapy Preventing anxiety Monitor for complications. Pulmonary Embolism 7. Auscultate breath sounds every 4 hours. 8. Assess vital sign and capillary refill, pain. 9. Encourage deep breathing and coughing, fluids, unless contraindicated. 10. Give oxygen to maintain oxygen saturation as ordered. 11. Give medications as ordered. Assess for evidence of bleeding. 12. Assist the client in assuming a position of comfort, if possible (high Fowler's position). Pneumothorax/Hemothorax 1. 2. 3. Traumatic disorders of the respiratory tract wherein the underlying lung tissue is compressed and eventually collapses. Types Simple Pnuemothrax Traumatic Pnuemothorax Tension Pneumothorax/Hemothorax 1. 2. 3. 4. 5. 6. 7. Clinical Manifestations Sudden pluretic pain Anxious patient , dyspnea & air hunger Increase use of accessory muscles Central cyanosis Tympanic sound in percussion Absent of breath sound & tactile fremitus Agitation Diaphoresis & hypotension Pneumothorax/Hemothorax 1. 2. 3. 4. 5. 6. 7. Medical Management High concentration supplemental O2 Chest tube for drainage In emergency anything may be use to fill the chest wound Heavy dressing Needle aspiration thoracenthesis Connecting chest tube to water seal drainage An emergency thoracotomy may also performed Pulmonary Edema Abnormal accumulation of fluid in lung tissue and or alveolar space , it sever life threatening condition Causes:-Can result from severe left ventrical failure, rapid administration of I.v. fluids, inhalation of noxious gases, or opiate or barbiturate overdose. Pulmonary Edema S&S 1. 2. 3. 4. 5. Dyspnea Air hunger Central cyanosis Anxious cough with foamy or froth often blood tinged secretion Confused Diagnosed by 1. 2. 3. Crackles Chest X-ray Hypoxemia Pulmonary Edema Management A- medical 1. 2. 3. 4. 5. Correct cause Vasodilatation Diuretic O2 Morphine to reduce anxiety and pain B- nursing 1. 2. 3. Assist for oxygenation and intubations Give medication as prescribed )morphine , vasodilator ) Monitor patient response Adult Respiratory Distress Syndrome (ARDS) A life-threatening condition characterized by severe dyspnea, hypoxemia, and diffuse pulmonary edema. Cause 1. 2. 3. 4. 5. 6. Aspiration Shock Trauma Major surgery Fat or air embolism Systemic sepsis ARDS S&S 1. 2. Rapid onset of severe Dyspnea Arterial hypoxemia Diagnosed by 1. 2. Chest X-ray Intercostals retraction Management A- medical 1. Treat underlining cause 2. Intubations Chest surgery: It is used to cure or relief disease condition such as lung abscess, cancer, cyst, and benign tumors. Most common chest surgery: Thoracotomy: surgical creation of opening into the thoracic cavity. Segmental resection: removal of small segment of lung tissue. Lobectomy: removal of a complete lobe. Pneumonectomy: removal of the lung. Chest surgery Preoperative assessment and intervention: 1. Prepare patient physically and psychologically 1. Physically: assess functional, nutrition 2. Psychologically: assess patient emotional status and fears and encourage him to communicate feelings. 2. 3. 4. 5. 6. 7. Explain examination: ECG, chest x-ray, sputum culture, bronchoscopic exam, blood test, pulmonary function test. Encourage ambulation (if allowed). Perform percussion and postural drainage. Good mouth care before and during the day of operation. Administer drugs: antibiotics, blood, and IV fluid as ordered. Explain about surgery and post operative procedure or care (he will stay 1-2 day in ICU, use of incentive spirometry, and care for the chest drainage). Chest surgery Postoperative assessment and intervention: 1. Assess vital sings. 2. O2 administration. 3. IV fluid (on low rate to prevent pulmonary edema). 4. NPO till recovery (as ordered). 5. Positioning patient according to surgical site Chest surgery 6-Give pain medication. 7-Frequently and continuously assess respiratory and cardiac function. 8-Support the chest when the patient is coughing by providing firm support for the patient's incision with your hands 9-Doing of passive exercise (rang of motion). 10-observe for sings of complication: -Cyanosis, dyspnea, and acute chest pain → Atelectasis. -Increase temperature and pulse→ beginning of infection. -Pallor and drop in BP → internal hemorrhage. 14-Check dressing for bright red blood (external hemorrhage). 15-Care for drainage.