PPT CORONARY CIRCULATION BY DR QAZI
advertisement

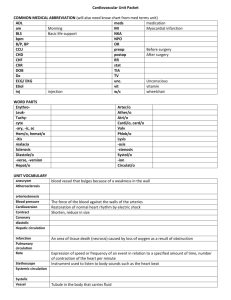
CORONARY CIRCULATION BY DR QAZI IMTIAZ RASOOL 1. 2. 3. Describe the physiological anatomy of coronary circulation. Identify the values for normal coronary blood flow. Discuss control of coronary blood flow. 4. Describe the physiological features of coronary circulation. 5. Correlate knowledge to clinical conditions related to myocardial ischemia. IMPORTANCE A) 1/3 rd Of All Deaths World Wide, B) 2/3 rd of which occur in the developing countries. C) CAD Prevalence In India- 3.5% In 1960s To 11% In Late 1990s In Urban India. Estimation - Doubling Of Deaths Due To CAD In India From 1985 To 2015. 1. represent the enlarged vasavasorum of larger vessels in the heart. 2. R about the width of a drinking straw,1/8 inch (4mm) . 3. 4. Coronary comes from the latin ”Coronarius= “Crown”. Arises from the sinuses just superior to the aortic valve behind cusps has 3 cusps –left coronary (LC), -right coronary (RC) -posterior non-coronary(NC) cusps. CHARACTERISTICS OF CORONARY CIRCULATION 1) Very short , rapid, and phasic . 2) Blood flow mainly during cardiac diastole 3) No efficient anastomoses between the coronary vessels. 4) It is a rich circulation (5% of the CO ,as heart wt is 300gm) 5) Regulation is mainly by metabolites and not neural 6) Capillary permeability is high (the cardiac lymph is rich in protein) 7) Vessels are susceptible to degeneration and atherosclerosis. 8) Evident regional distribution(subendocardial layer in LV receives < blood, due to compression (but normally compensated during diastoles by V.D). NOTE;- Hence more prone to IHD+MI. 8) Eddy current keep the valves away from the orifices of arteries it keeps the orifices patent throughout the cardiac cycle. 10) As having highest O2 uptake achieved by a dense network of capillaries, all is perfused at rest (no capillary reserve) 1. 2. 3. Length – 10-15mm Arises from left coronary cusps Almost immediately bifurcate into 1. left anterior descending 1. Diagonal Br.--- Most of Ant LV wall, A small part of RV 2.Septal perforating Br –ant 2/3rd to IVS 3.A part of the left br. Of the AV bundle 4.Terminal Br.---apex 2. Left circumflex artery. RIGHT CORONARY ARTERY Origin R anterior coronary sinus of Valsalva Courses through the R AV groove Branches;-Arteria coni arteriosis 1st Segment: 1. 2. 3. 4. Anterior Atrial Brs Artery to SA node Anterior Ventricular Brs Right Marginal Artery 1. 2. 3. 4. 5. Posterior Ventricular Brs Posterior Interventricular Brs Posterior Interventricular (descending) Artery Septal Brs AV nodal Artery 2nd Segment VENOUS DRAINAGE 2 systems: 1) Superficial system: which drains LV. It is formed of coronary sinus and anterior cardiac veins that open into the RA. 2) deep system: which drains the rest of the heart. It is formed of thebasian veins and arterio-sinusoidal vessels that open directly into the heart chamber. CAPILLARY DENSITY ANASTOMOTIC CHANNELS; Between coronary arteries & extracardiac arteries intercoronary anastomosis *IN NORMAL HEART THERE ARE NO COMMUNICATIONS BET n LARGE CORONARIES. * ANASTOMOSES DO EXIST AMONG THE SMALLER ARTERIES SIZED 20 TO 250 μ m. 3 Common areas of anastomoses. 1. Between branches of LAD & PIV OF RCA in iv groove 2. Between LCX & RCA IN AV groove. 3. Septal branches of 2 coronary arteries in the IVS. NOTE;-Lifesaving value of collaterals in heart: Occlusion-- within sec; dilatation n of small anastomoses( blood flow < ½) -normal or almost normal coronary (within 1 month). 1. 5% of CO = +/- 250ml / 60-80ml/100gm/min pass through coronary artery/min. 2. RCA has > flow in 50-70% of individual. 3. LCA > flow in 20% of individual. 4. Equal distribution of flow in 30% of individual. 5. At rest the heart extract 70-80% of O2 from each unit of blood delivered to it. NOTA;- Therefore, the most crucial factors for perfusing coronary arteries are - aortic pressure / - duration of diastole Why heart is extracting 60-70% of O2? 1. Muscle has 40% of cell is occupied by mitochondria 2. When more O2 is needed e.g. exercise, O2 can be increased to heart only by increasing blood flow. NOTE;- low-pressure limit for autoregulation in the endocardial layer is > in the epicardial layer. – endocardial arterial dilation reaches a maximum when arterial pressure drops to ~70 mm hg, whereas maximum dilation in the epicardial arteries is not reached until pressure is ~40 mm hg. BLOOD FLOW DURING SYSTOLE & DIASTOLE 1. In systole as muscle contracts it compresses arteries therefore CBF is less -LV during systole and more during diastole. 2. Subendocardial portion of LV, occurs only during diastole therefore, prone to IHD+MI. 3. CBF to R side is not much affected during systole. Reason;-Pressure difference between aorta and RV is greater during systole than during diastole, therefore more blood flow to RV occurs during systole 15 NOTE—Blood flow shows considerable Autoregulation. A.PHYSICAL FACTORS a. Cardiac cycle & myocardial pressure ( the phasic variation) – CBF not only varies in time during C.C also varies with depth in the wall of the heart norma subendocardium receives slightly > blood flow than epicardium(1.1:1) NOTE;- (LCA blood flow during systole is 15 - 16% of diastole) 2) Chemical factors(PRIMARY CONTROLLER) affecting Coronary blood flow a)Metabolic factors causing Coronary vasodilatation CBF 1. -Lack of oxygen 2. 3. 4. 5. -Increased local concentration of Co2 -Increased local concentration of H+ ion -Increased local concentration of k + ion -Increased local concentration of Lactate, Prostaglandin, Adenosine, Adenine nucleotides. 6. NO NOTE – Adenosine, which is formed from ATP during cardiac metabolic activity, b) Drugs: Nitrites,Aminophylline,Caffeine & Khellin are coronary vasodilator CBF. 3. Nervous Factors: - α (DOMANCE IN EPICARDIAL )ᵦ The effect of the autonomic nerves to the heart on the coronary arteries is indirect through their effect on cardiac metabolism I.e a) Stimulation of sympathetic cardiac metabolism coronary vasodilatation CBF. -Alpha Adrenergic receptors which mediate vasoconstriction Beta Adrenergic receptors which mediate vasodilatation b) Stimulation of parasymp cardiac metasbolism coronary vasoconst. CBF. 4. Neurohormonal factors 1. Thyroxin cardiac metabolism CBF. coronary vasodilator 2.Vasopressin (antidiuretic hormone) coronary vasoconst CBF. Applied Aspect CORONARY ARTERY DISEASE 21 is caused by myocardial ischemia due to Imbalance between myocardial oxygen demand and supply from coronary arteries. Four types of Ischemic Heart Diseases: 1. Angina pectoris (Most common) 2. Acute Myocardial infarction (AMI) 3. Chronic IHD 4.Sudden cardiac death (SCD) Unexpected death within 1 hour due to cardiac causes In many patients SCD is the first clinical manifestation of IHD 1. Literally means chest pain 2. Is intermittent chest pain caused by transient reversible myocardial ischemia. 3. 4. Ischemia insufficient to cause death of myocardium 3 Types: 1. Stable angina 2. Prinzmetal’s angina (Variant angina) occuring at rest due to coronary artery spasm. Stress ECG reveals ST elevation representing transmural ischemia 3. Unstable (crescendo) angina Frequent bouts of chest pain at rest or with minimal exertion. May progress to acute MI 24 1. Within seconds: Switch to Anaerobic glycolysis for ATP 2. Less than 2 min: loss of contractility 3. 1 - 10 min: Reversible injury 4. 20-40 minutes: irreversible damage 5. Reperfusion within 40 min. saves muscle. 25 26 27 1. Investigations: 1. ECG 2. Cardiac enzymes e.g. CK, LDH, Troponin etc. 3. Echocardiography 4. Treadmill exercise test 5. Thallium stress test 6. Coronary angiography 7. Note: 1. ECG changes in IHD: 1. St depression occurs in ECG in respective leads 2. ECG changes in MI: 1. St elevation occurs in ECG in respective leads 28 TREATMENT: 1. CORONARY DILATORS E.g. NITRATES 2. BETA-BLOCKERS 3. ANGIOPLASTY (DILATE AREA OF CONSTRICTION) 4. STENT 5. BYPASS SURGERY 29