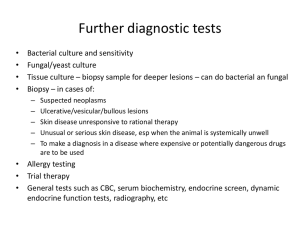
Post-surgical anti-BP230 bullous pemphigoid: a rare cause of non-healing wound Pipitò, Maglie, Senatore, Montefusco, Baffa, Bianchi, Del Bianco, Antiga Department of Health Sciences, Section of Dermatology, University of Florence, Florence, Italy Bullous pemphigoid is the most frequent autoimmune bullous disease and mainly affects elderly individuals. In most cases, it presents with itch and tense blisters over erythematous and edematous skin on the trunk and extremities. They may be localized in a certain area of the body surface or widespread. We report a case of bullous pemphigoid with unusual location and presentation. An 80year-old woman presented with a 10-month history of a nonhealing figurate erosive lesion that traces almost precisely the outline of the surgical abdominal scar following bowel resection for intestinal ischemia performed one year earlier. Since then, the lesion has been treated every 2-3 days with wound care dressings, without noticeable improvement; moreover, the use of topical and systemic antibiotics was ineffective as well. According to the clinical features and the medical history, the possible diagnostic hypotheses included, among others, post-traumatic bullous pemphigoid and pyoderma gangrenosum. Therefore, a skin biopsy of the lesion for histological examination, direct immunofluorescence (DIF) on perilesional skin, and blood drawn to search for skin-directed autoantibodies were performed. While histological examination was unspecific, DIF revealed the presence of linear IgG and C3 deposits at the basement membrane zone. Moreover, an enzyme-linked immunosorbent assay was positive for IgG against BP230 (30 UI/mL; reference value < 9 UI/ml), with no evidence of antiBP180 antibodies and indirect IF being negative. Clinical and laboratory findings were compatible with the diagnosis of post-traumatic anti-BP230 bullous pemphigoid. The patient was treated with an oral prednisone at 0.5 mg/kg/day, associated with topical application of clobetasol ointment 0.5%, achieving almost complete healing of the lesion in 3 weeks. Although BP180 is the major autoantigen of bullous pemphigoid, some cases of patients having only anti-BP230 autoantibodies have been reported yet. Interestingly, patients having bullous pemphigoid with only anti-BP230 autoantibodies usually show a more localized clinical involvement as well as atypical clinical features; moreover, some of these cases are secondary to trauma. It is also of note that experimental models of anti-BP230 bullous pemphigoid were more prone to develop the disease after skin wounding with subsequent antigen exposure. The case reported herein confirmed these findings and hypotheses; accordingly, surgical trauma might have served as a trigger, leading to the exposure of the antigen and, subsequently, to an autoimmune response toward BP230 in a predisposed individual. In conclusion, bullous pemphigoid should be considered as a differential diagnosis in patients with post-surgical wounds that do not heal with conventional wound care; in these patients, steroids, that are not used as a standard treatment for wound healing, usually lead to a prompt remission with improvement of the quality of life of the patient.