Respiratory Bacteria Vaccines: Model Analyses for Vaccine and Vaccine Trial Design
advertisement

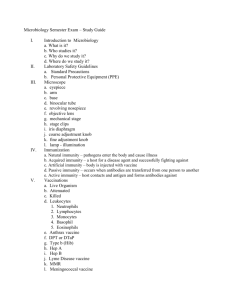
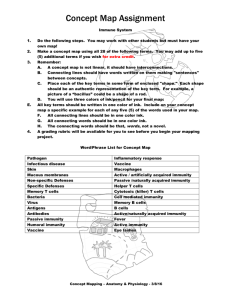
Respiratory Bacteria Vaccines: Model Analyses for Vaccine and Vaccine Trial Design Jim Koopman MD MPH Ximin Lin MD MPH Tom Riggs MD MPH Dept. of Epidemiology & Center for Study of Complex Systems University of Michigan Questions Addressed • What role does immunity affecting pathogenicity vs. transmission play in the sharp drop with age in NTHi otitis media? • What vaccine effects should be sought and measured in trials? • How should vaccine trials be designed to insure adequate power to detect important effects? General Issues Regarding NTHi • Causes 20-40% of acute otitis media • Vaccine market 1 billion $ per year in U.S. • Infection, immunity, and disease data is meager, non-specific, & highly variable • Knowledge of natural history of infection and immunity is deficient • Unquestioned assumption that vaccine trials will be individual based and assess disease outcomes Aspects of NTHi (& many other bacterial) infections • Partial immunity, rarely sterilizing – IgA proteases show evolutionary importance of immunity • Many variants arise due to transformation competency – No permanent strains yet identified • Immunity to colonization or infection, disease, & transmission can be distinct Using NTHi Models for Inference • Models with diverse natural Hx of infection and immunity, age groupings, and contact patterns were constructed • • • • • Deterministic compartmental (DC) models built first Gradual acquisition of immunity with each colonization and continuous loss over time All models were fit to the full range of data conformations deemed plausible using least squares Projections of vaccine effects made for all fits of all models (about 1000 total) Individual event history stochastic models corresponding to the DC models were used for vaccine trial design Natural history of NTHi colonization Susceptible Ca Cb D Cc Susceptible with* Susceptibility: θ n (n=0, …, m) Infectiousness: n (n=0, …, m) Pathogenecity: n (n=0, …, m) Colonization & Disease Waning of Immunity with* Susceptibility: θ min(n+1, m) Infectiousness: min(n+1, m) Pathogenecity: min(n+1, m) FA model D S Ca Cb S’ Modeling partial immunity Model agent variation and host response as single process Assumptions • equal immunity from each colonization • multiplicative effects of sequential infections • immunity limit (m levels) • immunity waning Modeling partial immunity: S1I1S2I2S3I3……Sm-1Im-1SmIm vs. SIR/SIRS/SIS S1 Ca1 S2 Ca2 Cb1 Sm D2 Cc1 Cb2 D1 Cc2 m-1 m-1 m-1 C am Cbm Dm m-1 m-1 m-1 Ccm m-1 m-1 Aspects of Immunity Modeled • Susceptibility • Contagiousness • Pathogenicity • Duration Population structure • Preschool children (0.5-5 years) 1. Day-care + Non-day-care 2. 9 age groups with 6-month interval • School children (5-15 years) • Adults Population structure Deaths Births Births N1 6-12 Mos daycare N10 6-12 Mos no daycare Aging Aging Deaths Deaths ... N9 54-60 Mos daycare Aging N19 5-15 Years ... N18 54-60 Mos no daycare Aging Deaths Deaths Aging Deaths N20 >=15 Years Contact structure General Mixing G Daycare N1-N9 G Non-Daycare N10-N18 D G G Adult N20 School N19 S Daycare Mixing School Mixing Population parameters Death rate of individuals less than 1 year 0.00181 Death rate of individuals aged 1-2 years 0.00036 Death rate of individuals aged 3-4 years 0.00036 Death rate of individuals aged 5-15 years 0.00021 Death rate of individuals aged 15 years and over 0.01086 Annual birth rate into 7-12 month age group 0.00938 Rate at which children enter daycare 0.174 Rate at which children leave daycare 0.0358 Day-care attendance at 6 months 0.0785 * The units of all rates are year-1. Limited & Highly Variable Epidemiologic data • NTHi prevalence by age & daycare attendance (diverse methods) • AOM incidence < age 5 by daycare (combine incidence studies & fraction with NTHi studies) • Antibody levels by age (diverse methods) • Colonization duration (quite limited) • Daycare risk ratios for AOM Colonization prevalence values fitted Low Values High Values Colonization prevalence ages 0-5 when in daycare Colonization prevalence ages 0-5 when not in daycare Colonization prevalence ages 6-15 23% 51% 9.5% 21% 7% 15% Colonization prevalence in adults 4% 9% Annual NTHi AOM incidence age* <1 0.08 0.22 Annual NTHi AOM incidence age 1-2 0.13 0.33 Annual NTHi AOM incidence age 2-3 0.08 0.22 Annual NTHi AOM incidence age 3-4 0.06 0.18 Annual NTHi AOM incidence age 4-5 0.05 0.17 AOM Incidence values fitted Other Data • Antibody levels peak during elementary school • Daycare Risk Ratios from 2 to 3 • Colonization mean of 2 months but many transient episodes and some long (limited data) • Waning “seems” to be relatively fast Presumptions Before Our Work • Very different from Hi Type B • Colonization is so frequent, even at older ages, that immunity to transmission cannot be important • Trials should assess effects on AOM, not colonization General assumptions of our model • Every colonized individual is infectious • Acute otitis media (AOM) is the only relevant disease (Unlike Hi Type B or Strep pneumo) • Maternal immunity (Children aged 0-6 months totally immune from colonization) Fitting model to epidemiologic data • Berkeley Madonna: “boundary value ODE…” & optimize functions • Empirical identifiability checking • Extensive robustness assessment for both data conformation and model conformation rather than estimating variance of estimates Fitting Results • Most efficient level # is 4 • Needed immunity profile includes – Susceptibility – Contagiousness – Pathogenicity • Contagiousness and Duration Effects are highly co-linear when fitting equilibrium Parameter values that fit NTHi prevalence & AOM incidence for models without all immunity effects. Immune Effects In The Model (Path effects in all models) Susc S& Infect S & Durat D &I Goodness of Fit (Root Mean Square Error) 0.01 0.02 0.03 0.37 Duration of immunity (years) 84.7 9.8 4.0 5.1 Relative susceptibility after each colonization 0.55 0.519 0.535 1 Relative contagiousness when re-infected 1 0.76 1 0.301 Relative duration of colonization when re-infected 1 1 0.839 0.599 Colonization prevalence and AOM incidence data fit* H col H AOM H col L AOM L col H AOM L col L AOM Goodness of fit (root mean square error) 0.07 0.05 0.05 0.02 Duration of each level of immunity (years), 3.7 4.7 3.4 9.8 Duration / stage colonization | lowest immunity 0.104 0.107 0.0613 0.0549 P(AOM | colonization at the lowest immunity) 0.343 0.127 0.374 0.136 % decrease in AOM probability per immunity level (pathogenicity effect), 0.334 0.301 0.294 0.279 % decrease in susceptibility per immunity level, 0.597 0.594 0.732 0.481 % decrease in contagiousness / immunity level, 0.582 0.237 0.116 0.24 Effective contact rate per year at general site, 173 80.1 50.3 94.4 Effective contact rate per year at daycare site, 655 218 359 113 Effective contact rate per year at school site, 301 68 217 61 Data Conformation Fitted Colonization Prevalence High High Low Low AOM Incidence High Low High Low Sensitivity Analysis to 10% Change In Pathogenicity or Transmission Immunity AOM Incidence Decrease Immunity Type Decreased 0-1 year 1-2 years 2-3 years 3-4 years 4-5 years Pathogenicity 1.6% 3.9% 7.9% 10.9% 12.5% Transmission 12.0% 9.5% 11.8% 17.8% 23.4% Pathogenicity 1.6% 3.8% 7.6% 10.2% 13.2% Transmission 23.4% 14.6% 15.3% 23.6% 32.8% Pathogenicity 1.4% 2.9% 5.1% 6.8% 8.1% Transmission 15.9% 19.2% 32.6% 48.7% 62.7% Pathogenicity 1.8% 3.7% 6.7% 9.0% 10.4% Transmission 59.7% 34.1% 33.5% 53.2% 70.3% Age 0-1 Age 1-2 Age 2-3 Age 3-4 Age 4-5 Base analysis from previous Table 16.5 5.5 3.7 4.2 4.8 Only susceptibility effects on transmission 15.6 6.0 3.9 4.3 4.7 Susceptibility and duration effects on transmission 8.4 2.6 1.4 1.5 1.8 Susceptibility, contagiousness, & duration effects on transmission 10.2 3.3 2.1 2.5 2.8 Eight levels of immunity 4.6 5.1 2.0 1.5 1.7 Alternate ratios of contact rates by age at the general mixing site 39.5 11.0 5.9 6.7 7.6 Prevalence and incidence fall more steeply with age 19.2 4.7 0.6 0.6 1.2 Prevalence and incidence fall less steeply with age 9.5 3.3 2.0 2.0 2.0 Simpler pattern of compartments for the natural history of infection and immunity 36.3 6.4 3.2 3.4 3.9 Further Sensitivity Analysis Vaccination Immunity acquisition & waning for P vaccine (Vaccine effects don’t exceed natural immunity effects) Vaccination Immunity acquiring & waning in vaccinated population: SIP vaccine Vaccination strategy All children at age of 6 months vaccinated % reduction in AOM incidence among all preschool children as the result of vaccination at birth P % Reduction of AOM Incidence 90% IP SP SIP 80% 70% 60% 50% 40% 30% 20% 10% 0% 4_LL 8_LL 4_HH Models 8_HH % reduction in AOM incidence among preschool children due to vaccination at birth. P_Daycare % Reduction of AOM Incidence 100% 90% SIP_Daycare P_Non-daycare 80% SIP_Non-daycare 70% 60% 50% 40% 30% 20% 10% 0% 6-12 12-18 18-24 24-30 30-36 36-42 42-48 48-54 54-60 Age (months) Absolute reduction of AOM incidence by age and daycare attendance among preschool children due to vaccination at birth. AOM Cases per 100 Person-years 30 P_Daycare 25 SIP_Daycare P_Non-daycare 20 SIP_Non-daycare 15 10 5 0 6-12 12-18 18-24 24-30 30-36 36-42 Age (months) 42-48 48-54 54-60 AOM cases among daycare and non-daycare children from a population of 1,000,000 before and after vaccination at birth with SIP vaccines. 700 Before vaccination_daycare No. of AOM Cases 600 After vaccination_daycare Before vaccination_non-daycare 500 After vaccination_non-daycare 400 300 200 100 0 6-12 12-18 18-24 24-30 30-36 36-42 42-48 48-54 54-60 Age (months) Summary of Deterministic Model Findings • Wide range of feasible models fit to a wide range of feasible data • Over this entire huge range, the intuition that immune effects on pathogenicity are the major determinants of AOM incidence proves to be wrong • Trials must assess transmission Model Refinements Desirable • Model agent strains with different degrees of cross reacting immunity • Incorporate evolution of agent into vaccine effect assessment • Make maternal immunity and acquisition time for vaccine immunity more realistic Additional Practical Need for Indirect Effects • Very young age of highest risk means little time to get all the booster effects needed Using NTHi Models for Inference About Vaccine Trial Design • • • • Convert deterministic compartmental model to individual event history model Add distinct daycare units and families Construct vaccine trials assessing colonization in the IEH models with varying randomization schemes, vaccine effects exceeding natural immunity, sample collection periods, serology & typing results Hundreds of thousands of vaccine trial simulations performed Conclusions from Vaccine Trial Simulations • Most efficient randomization unit is daycare – Individual randomized trials run too much risk of missing important vaccine effects • Standard power calculation methods for Group Randomized Trials are far off because they are based on individual effect • Role of inside vs. outside transmission in daycare significantly affects power • Molecular assessment of transmission worthwhile Standard variance calculation in Group Randomized Trials (GRTs) P ( 1 P ) • variance: (1 ( N 1) ICC ) N • ICC: intraclass correlation • Assumes objective is measurement of individual effects ICC & Vaccine effect Change of ICC with Prevalence, Daycare Size, and Vaccine Effect 1 0% 5% 10% 15% 20% DC Size: 25; Before Vax DC Size: 25; S: 90% DC Size: 25; S: 0% 0.1 ICC I0% I50% I60% I70% I80% 0.01 I90% I70% I65% I85% I90% I95% I60% …... DC Size: 200; S: 0% 0.001 25% DC Size: 200; S: 90% NTHi prevalence DC Size: 200; Before Vax Change in Variance with Daycare Size & Sample Size Change of Variance with Daycare Size 0.1 0% 5% 10% 15% 20% Variance 0.01 0.001 DC Size: 25; Subsample Size: 25 DC Size: 200; Subsample Size: 25 DC Size: 200; Subsample Size: 200 0.0001 NTHi prevalence 25% Preliminary results (1): variance & immunity Change of Variance with Prevalence, Daycare Size, and Vaccine Effect 0.100 0% 5% 10% 15% 20% 25% DC Size: 25; Before Vax DC Size: 25; S: 0% Variance 0.010 0.001 I65% I60% DC Size: 25; S: 90% I70% I0% I75% I80% I50% I85% I60% I90% I70% I95% I80% I65% I90% I75% I70% I90% I80% I90% I85% I90% I90% I90% I95% I90% DC Size: 200; S: 0% I90% DC Size: 200; S: 90% 0.000 NTHi prevalence I60% DC Size: 200; Before Vax Simple Model For Insight S I S* Equilibrium distribution of states solved theoretically for daycare with 12 children Vaccine effect decreases susceptibility by 50% Unvacc mostly within trans 30%Prev Unvacc mostly outside trans SIS* cum prob distn (UNVAC) 1 1 0.8 0.8 0.6 S 0.4 I S* 0.2 Prob. distn Prob. distn SIS* cum prob distn (UNVAC) 0.6 S 0.4 I S* 0.2 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 1 2 3 4 5 # infected 0.8 0.8 0.6 0.4 S_vac 0.2 I_vac S*_vac 0 5 6 7 8 # infected 9 10 11 12 13 Prob. distn Prob. distn 1 4 9 10 11 12 13 SIS* cum prob distn (VAC) 1 3 8 Vacc mostly outside trans SIS* cum prob distn (VAC) 2 7 # infected Vacc mostly within trans 1 6 0.6 0.4 S_vac 0.2 I_vac S*_vac 0 1 2 3 4 5 6 7 8 # infected 9 10 11 12 13 Unvacc mostly within trans 50%Prev Unvacc mostly outside trans SIS* cum prob distn (UNVAC) 1 1 0.8 0.8 0.6 S 0.4 I Prob. distn Prob. distn SIS* cum prob distn (UNVAC) S* 0.2 0.6 S 0.4 I S* 0.2 0 0 1 2 3 4 5 6 7 8 1 9 10 11 12 13 2 3 4 5 7 8 9 10 11 12 13 # infected # infected Vacc mostly within trans Vacc mostly outside trans SIS* cum prob distn (VAC) SIS* cum prob distn (VAC) 1 1 0.8 0.8 0.6 0.4 S_vac 0.2 I_vac Prob. distn Prob. distn 6 0.6 0.4 S_vac 0.2 I_vac S*_vac 0 S*_vac 0 1 2 3 4 5 6 7 8 # infected 9 10 11 12 13 1 2 3 4 5 6 7 8 # infected 9 10 11 12 13 Significance of S & S* Contribution to Power Calculation • Serological ability to assess cumulative infection level would contribute considerably to power Empirical power calculation Empirical power & the number of the pairs of daycare centers Why standard power calculations for GRTs are way off • ICC is determined by transmission dynamics • Effect is determined by transmission dynamics • Power is not just determined a single outcome state but by correlated infection and immunity states Thank You