Endocrine Control of Growth Metabolism
advertisement
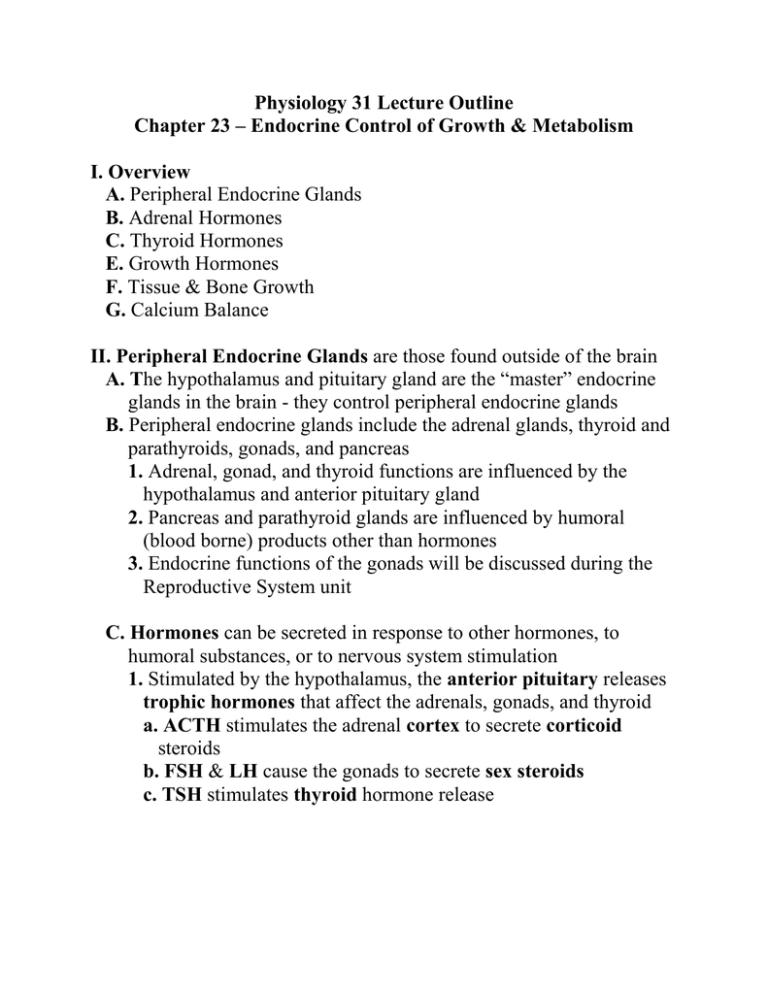
Physiology 31 Lecture Outline Chapter 23 – Endocrine Control of Growth & Metabolism I. Overview A. Peripheral Endocrine Glands B. Adrenal Hormones C. Thyroid Hormones E. Growth Hormones F. Tissue & Bone Growth G. Calcium Balance II. Peripheral Endocrine Glands are those found outside of the brain A. The hypothalamus and pituitary gland are the “master” endocrine glands in the brain - they control peripheral endocrine glands B. Peripheral endocrine glands include the adrenal glands, thyroid and parathyroids, gonads, and pancreas 1. Adrenal, gonad, and thyroid functions are influenced by the hypothalamus and anterior pituitary gland 2. Pancreas and parathyroid glands are influenced by humoral (blood borne) products other than hormones 3. Endocrine functions of the gonads will be discussed during the Reproductive System unit C. Hormones can be secreted in response to other hormones, to humoral substances, or to nervous system stimulation 1. Stimulated by the hypothalamus, the anterior pituitary releases trophic hormones that affect the adrenals, gonads, and thyroid a. ACTH stimulates the adrenal cortex to secrete corticoid steroids b. FSH & LH cause the gonads to secrete sex steroids c. TSH stimulates thyroid hormone release 2 2. Humoral products, such as glucose and calcium can influence hormone release a. Glucose plasma concentration affects the pancreas 1) High glucose levels cause the pancreas to release insulin, which decreases glucose levels 2) Low glucose levels stimulate pancreatic release of glucagon, which increases glucose levels 3) Pancreatic hormone effects will be discussed during “Metabolism and Energy Balance” b. Calcium plasma concentration influences the thyroid and parathyroid glands 1) High calcium levels cause the thyroid gland to secrete calcitonin, which decreases Ca2+ levels 2) Low calcium levels stimulate the parathyroid glands to release PTH, which increases Ca2+ levels 3. Nervous system stimulation influences the posterior pituitary and adrenal medulla a. Neurons in the hypothalamus produce neurohormones that are stored in the post. pituitary until needed b. Nerve impulses during “fight or flight” reactions stimulate the adrenal medulla to release epinephrine and norepinephrine c. Catecholamines will be discussed in the nervous system III. Adrenal Corticoids A. The adrenal cortex secretes steroid hormones, including mineralo, gluco-, and gonadocorticoids. All are made from cholesterol 1. Mineralocorticoid (i.e., aldosterone) affects mineral uptake a. Are secreted from the cortex’s outer zona glomerulosa b. Aldosterone influences sodium and potassium uptake in the kidney tubules. This will be discussed with the Urinary system 2. Gonadocorticoids (i.e., sex hormones) are released by the cortex’s inner zona reticularis 3. Glucocorticoids (e.g., cortisol) a. Are secreted by the mid cortex zona fasciculata b. Increase plasma glucose levels 3 B. Cortisol secretion is controlled by ACTH 1. CRH is sent from the Hypothalamus to the ant. Pituitary, which causes it to release 2. ACTH, which stimulates the adrenal cortex to secrete 3. Cortisol, which increases blood glucose levels (esp. during stress), and feeds back to inhibit ACTH and CRH release a. Cortisol is secreted continuously in a diurnal rhythm – it peaks in the morning and diminishes at night b. Cortisol is bound to corticosteroid-binding globulin (CBG) in the blood c. Cortisol diffuses into a cell and binds to a glucocorticoid receptor d. The cortisol-receptor complex bind to DNA and alter gene expression, which results in several responses C. Cortisol is essential to life 1. Cortisol has a permissive effect – it’s required for glucagon and the catecholamines to have their full effects 2. The effects of cortisol are mainly catabolic, and include a. Promotes gluconeogenesis in the liver b. Causes the breakdown of skeletal muscle proteins c. Enhances lipolysis d. Suppresses the immune system e. Causes negative calcium balance – decreases blood Ca2+ levels by decreasing Ca2+ absorption and increasing excretion f. Influences brain function – excess or deficiency cause mood changes and alteration in memory and learning D. Cortisol is a useful therapeutic drug 1. Cortisol suppresses the immune system by a. Prevents cytokine release and antibody production by WBCs b. Inhibits the inflammatory response by decreasing WBC mobility 4 2. Immunosupression allows cortisol to be used to treat allergic reactions and inflammatory conditions (e.g., rheumatoid arthritis) 3. Due to cortisol’s side effects, NSAIDs are prescribed more frequently 4. Exogenous cortisol feeds back to the ant. Pituitary and shuts down ACTH production E. Cortisol pathologies result from too much or too little hormone 1. Hypercortisolism is excess cortisol in the blood, which causes Cushing’s syndrome a. Symptoms - hyperglycemia, muscle weakness, hypertension, moodiness, and fatty deposits in the trunk & face b. Causes are 1) Adrenal tumor that secretes xs cortisol 2) Pituitary tumor that secretes xs ACTH 3) Iatrogenic (physician-caused) due to cortisol medication 2. Hypocortisolism is too little adrenal steroid hormones in the blood, which causes Addison’s disease a. Symptoms - hypoglycemia, hypotension, electrolyte imbalance, skin bronzing, dehydration, weight loss, weakness F. CRH and ACTH have additional physiological functions 1. CRH and ACTH have multiple receptor types in numerous tissues, thus have many effects 2. Effects of CRH a. Suppresses immune response b. Decreases food intake c. Influences mood disorders 3. Effects of ACTH & Melanocortins a. Pro-opiomelanocortin (POMC) is used to synthesize ACTH as well as other peptide hormones b. β-endorphin is a POMC opiate that binds to and blocks pain receptors c. POMC is also used to make melanocyte-stimulating hormone (MSH) that acts on melanocytes that influence skin color 5 IV. Thyroid Hormones A. Thyroid hormones are produced by two cell types in the thyroid gland in the throat 1. C cells secrete calcitonin 2. Follicular cells release thyroid hormones (TH) B.Thyroid hormones (TH) contain iodine 1. Thyroid follicles are filled with colloid containing a protein precursor to TH called thyroglobulin, and enzymes 2. THs are made from the amino acid tyrosine and iodine a. Iodine (I-) from food is actively transported into follicular cells b. Enzymes attach I- to tyrosine on the thyroglobulin molecule in the colloid to make T3 and T4 (thyroxine) c. Thyroglobulin is endocytosed into follicular cells, where enzymes free T3 and T4 from the protein d. T3 and T4 are lipid-soluble, thus diffuse out of the cells into the plasma and bind to thyroid-binding proteins e. T3 and T4 bind to nuclear receptors and initiate protein synthesis e. T4 is converted by enzymes to T3, the active hormone, in target tissues C. Thyroid hormones affect the quality of life 1. Thyroid hormones are not essential, but they do influence a. Metabolic rate – TH is thermogenic, increasing oxygen consumption in mitochondria b. Protein, carbohydrate, and fat metabolism 2. In children, thyroid hormone is necessary for the full expression of growth hormone, and neurological development 3. Hyperthyroidism results in a. Warm, sweaty skin, heat intolerance b. Weight loss due to protein catabolism c. Psychological disturbances d. Rapid heartbeat (tachycardia) 6 4. Hypothyroidism results in a. Cool skin, intolerance to cold b. Myxedema – fluid under the skin, brittle nails, thinning hair c. Fatigue and slowed mental processes d. Slowed heartbeat (bradycardia) e. Cretinism (mental retardation) in infants D. TSH controls the thyroid gland 1. TRH from the hypothalamus triggers the release of 2. TSH from the ant. Pituitary, which stimulates the release of 3. TH from the thyroid gland 4. Goiters (a bulge in the neck), are a result of over stimulation of the thyroid by excess TSH caused by a. Primary hypothyroidism due to a lack of iodine in the diet 1) Because less TH is made, negative feedback is removed 2) More TSH is secreted causing thyroid hypertrophy 3) Hypothyroidism is treated with oral thyroxine b. Hyperthyroidism leads to Graves’ disease 1) Thyroid-stimulating antibodies combine with thyroid TSH receptors and activate them, resulting in thyroid enlargement 2) Exopthalamus (bulging eyes) may also occur 3) Hyperthyroidism is treated by removal or destruction of all or part of the thyroid gland, or by drugs that block conversion of T4 to T3 V. Growth Hormone A. Normal growth depends upon 1. Growth hormone (GH), TH, insulin, and sex hormones 2. A diet that includes protein, vitamins, and minerals 3. Absence of excess stress 4. Genetic inheritance 7 B. Growth hormone (somatotropin) is anabolic 1. GHRH and GHIH (somatostatin) from the hypothalamus promote or inhibit the release of 2. GH from the ant. Pituitary, which stimulates anabolic activity in endocrine and nonendocrine cells. In response to GH: a. The liver secretes Insulin-like Growth Factors (IGFs), which act with GH to stimulate bone, cartilage, and muscle growth b. IGFs direct energy and amino acids into protein synthesis c. Fat breakdown and liver glucose output are increased C. Growth hormone is necessary for a child’s growth 1. Deficient GH, or defective GH receptors in a child leads to dwarfism 2. Excess GH production in children causes gigantism 3. In adults, excess GH leads to acromegaly – jaw lengthening, coarse facial features, and growth of hands and feet VI. Tissue & Bone Growth A. Tissue growth requires GH, TH, and insulin 1. GH , TH, and IGFs are needed for protein synthesis and cell division, which lead to a. Hypertrophy – increase in cell size b. Hyperplasia – increased cell number 2. Insulin supports tissue growth by stimulating protein synthesis and providing glucose for energy B. Bone growth requires adequate dietary calcium 1. Bone is composed of hydroxyapatite (CaPO4) crystals attached to a collagen support network a. CaPO4 provides rigidity in the bone b. Collagen allows bone flexibility 8 2. Bone is a dynamic, living tissue, constantly being remodeled by bone and cartilage cells a. Osteoblasts secrete bone osteoid matrix; bone diameter increases as the matrix is deposited on the outer bone surface b. Linear bone growth occurs at epiphyseal (cartilage) plates in the ends (epiphyses) of long bones 1) Cartilage cells multiply, elongate, then degenerate, leaving spaces that osteoblasts invade 2) Osteoblasts lay down bone matrix over the cartilage, causing the bone to lengthen at each end 3) When osteoblasts complete their work, they become osteocytes 4) Sex hormone secretion at puberty initially stimulates bone growth, then gradually cause the epiphyseal plates to ossify, ceasing their linear growth c. Osteoclasts are bone cells that break down (reabsorb) bone tissue VII. Calcium Balance A. The majority of calcium is concentrated in bones, but the small amount in the blood plasma is crucial to life processes, including 1. Intracellular 2nd messenger signaling 2. Exocytosis of materials from cells 3. Muscle contraction 4. Blood coagulation 5. Neural function a. Hypocalcemia increases neural activity, causing sustained contraction (tetany) of respiratory muscles, resulting in suffocation b. Hypercalcemia decreases neuromuscular activity B. Blood calcium concentrations are closely regulated 1. Calcium homeostasis follows the principle of mass balance: Total body calcium = intake – output a. Ca2+ intake is from the diet and uptake from the small intestine 9 b. Ca2+ output occurs mainly in the kidneys, and a bit in the feces c. Total body Ca2+ is divided among three compartments 1) Extracellular fluid/plasma; [Ca2+] is about 2.5 mM 2) Intracellular Ca2+– free in the cytosol, in mitochondria, and in the sarcoplasmic reticulum of muscle cells 3) Extracellular matrix in bones – the largest Ca2+ reservoir (about 2.5 lbs) 2. Osteoblasts take Ca2+ from plasma and deposit it into bones 3. Osteoclasts secrete acid and enzymes to dissolve (reabsorb) bone and increase Ca2+ plasma levels C. Three hormones control Ca2+ balance: PTH, vit. D, and calcitonin 1. Parathyroid gland receptors sense declining Ca2+ levels and secrete PTH, which travels to a. Bones, where osteoclasts are stimulated to reabsorb Ca2+ b. Kidneys, where Ca2+ is reabsorbed into the blood, rather than excreted in the urine c. Small intestines, where Ca2+ uptake is increased via PTH’s influence on vit. D (calcitriol) 2. Calcitriol (vit. D) is ingested or made in the skin, liver, and kidneys in response to UV radiation. Calcitriol facilitates a. Uptake of Ca2+ from the intestines and kidneys b. Mobilization of Ca2+ out of bone into the ECF 3. Calcitonin is secreted by thyroid C-cells in response to increasing blood Ca2+ levels, and stimulates Ca2+ deposition in bones D. Calcium and phosphate homeostasis are linked 1. Factors that affect Ca2+ uptake, also affect phosphate uptake 2. Phosphate is needed for ATP, DNA & RNA, and enzymes E. Osteoporosis is a disease of bone loss that occurs when bone resorption exceeds bone deposition 1. Occurs in about 75% of women after menopause 2. Risk factors include thiness, age, smoking, and low Ca2+ intake