- Digestive System
advertisement

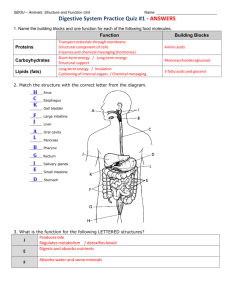
1 Anatomy & Physiology 34B Chapter 23 - Digestive System I. Overview A. Introduction to the Digestive System B. Serous Membranes & Tunics of the GI Tract C. Mouth, Pharynx, & Associated Structures D. Esophagus & Stomach E. Small Intestine F. Large Intestine G. Liver, Gallbladder, & Pancreas II. Introduction to the Digestive System A. The food we eat must be mechanically and chemically reduced to smaller molecules that can be 1. Absorbed through the intestinal wall 2. Transported to the cells by the blood B. The digestive system functions to process food, extract nutrients from it, and eliminate the residue. The stages include: 1. Ingestion - taking food into the mouth 2. Mechanical digestion - chewing food, churning it in the stomach and small intestine 3. Motility – movement of food through the alimentary canal; includes swallowing and peristalsis (wavelike contractions of the GI tract) 4. Chemical digestion - chemical hydrolysis of macromolecules to their absorbable monomers (proteins amino acids, carbohydrates monosaccharides, nucleic acids nucleotides, and fats fatty acids, & glycerol) 5. Glandular Secretion of enzymes, hormones and other products that carry out or regulate digestion. 2 6. Absorption - passage of food molecules through the small intestine mucous membrane into blood and lymph capillaries for distribution to cells 7. Defecation - discharge of indigestible wastes (feces) from the GI tract C. General Anatomy - the digestive system can be divided into two anatomical subdivisions 1. Alimentary canal (GI tract) - tubular structure composed of (from mouth to anus): a. oral cavity and pharynx b. esophagus and stomach c. small & large intestines 2. Accessory organs, which include the following: a. teeth, tongue, and salivary glands b. liver and gall bladder c. pancreas D. It takes about 24-48 hrs for food to pass through the GI tract. E. Each region of the GI tract has specific functions in preparing food for utilization 1. Oral cavity - grinds food and mixes it with saliva; initiates carbohydrate digestion and forms a food bolus which is swallowed and passed from pharynx to 2. Esophagus - transports bolus to stomach by peristalsis; lower esophageal (cardiac) sphincter prevents food backflow 3. Stomach - churns the bolus with gastric juices; initiates protein digestion; has some absorption; moves partially digested food (chyme) into the duodenum 4. Small intestine - mechanically & chemically breaks down chyme with secretions from the liver & pancreas; absorbs nutrients; transports wastes via peristalsis to the 3 5. Large intestine - receives undigested wastes, absorbs water & electrolytes; forms, stores, and expels feces 4 III. Serous membranes & Tunics of the GI tract A. Serous membrane characteristics 1. Is composed of simple squamous epithelium and some CT 2. Secretes serous fluid that lubricates the organs 3. Lines the abdominopelvic cavity and covers the organs a. Parietal peritoneum lines the wall of the cavity 1) Forms a double layered peritoneal fold called the mesentary in the posterior abdominal cavity 2) Mesocolon is part of the mesentary that supports the large intestine 3) Falsiform ligament attaches the liver to the diaphragm & anterior abdominal wall 4) Greater omentum - fatty peritoneum extension from stomach to transverse colon that covers, cushions, and protects the viscera 5) Lesser omentum - passes from the stomach & upper duodenum to the inferior liver 6) The omenta above also contain many nerves, blood and lymphatic vessels, and lymph nodes that fight abdominal infections b. Visceral peritoneum covers the intestinal organs 1) Peritoneal cavity is the space between the parietal and visceral peritoneum 2) Organs such as the kidneys, adrenal glands, and parts of the pancreas, duodenum, and abdominal aorta lie behind the peritoneum (retroperitoneal) 4. Peritonitis is an inflammation of the peritoneum, often caused by a burst appendix 5 B. Tunics of the GI Tract, from the inside out, include the mucosa, submucosa, muscularis externa, and serosa 1. Mucosa - thin layer that lines the GI tract lumen; consists mainly of simple columnar epithelium with goblet cells (except the mouth, esophagus and lower anus, which are lined with stratified squamous epithelium) plus a. Lamina propria - layer of aerolar or reticular CT that contains lymphoid tissue and lies deep to the epithelial layer b. Muscularis mucosa – deep to the lamina propria; smooth muscle layer; has many folds (plicae circularis) in the small intestine 2. Submucosa - thick, CT & vascular layer that serves the mucosa a. Absorbed food molecules pass through the mucosa into the blood vessels or lymph vessels of the submucosa b. Also contains glands & nerve plexuses, such as the submucosal (Meissner) plexus, that provides ANS innervation to the muscularis mucosa 3. Muscularis externa – consists of an inner circular & outer longitudinal layers of smooth muscle a. Rhythmic contraction of these muscles (peristalsis) moves, pulverizes, and churns food with digestive enzymes b. Myenteric plexus between the muscle layers provides the major ANS nerve supply to the GI tract 4. The outermost binding & protective layer may be the serosa or adventitia, depending on where it is located a. Serosa – is found on intraperitoneal organs & consists of 1) Simple squamous epithelium (visceral peritoneum) sandwiched between 2) Aerolar CT b. Adventitia is composed of fibrous CT and found on organs not associated with the peritoneal cavity (e.g.: esophagus) 6 c. Retroperitoneal organs have a serosa on their peritoneal side & an adventitia on their posterior abdominal cavity side C. Regulation of the digestive tract – motility and secretion is controlled by neural, hormonal, and paracrine mechanisms 1. Neural controls include autonomic reflexes called short reflexes and long reflexes a. Short reflexes involve stretching or chemical stimulation of the GI tract acting through the myenteric plexux to stimulate the muscularis externa for peristaltic contractions b. Long (vasovagal) reflexes act through ANS nerve fibers that carry sensory signals to the CNS and motor commands back to the GI tract. Digestive motility and secretion are stimulated 2. Hormones produced by the GI tract include gastrin and secretin, as well as paracrine secretions such as histamine and prostaglandins that stimulate digestive function 3. Paracrine secretions diffuse through the tissue fluids and stimulate nearby target cells IV. Mouth, Pharynx & Associated Structures A. The oral cavity (mouth) is formed by the cheeks, lips, hard & soft palates 1. Cheeks consist of skin, fat, muscles, and are lined with nonkeratinized stratified squamous epithelium 2. Lips are formed from the obicularis oris muscle, CT, and skin; a labial frenulum attaches each lip to the gum medially 3. The palate forms the roof of the oral cavity and consists of a. Hard palate - formed by the palatine bones and palatine process of the maxillae b. Soft palate - posterior skeletal muscle arch continuous with the hard palate anteriorly c. Uvula - cone-shaped medial projection of the soft palate; folds upward during swallowing to prevent food from entering the nasal cavity 7 d. Palatine tonsils are found on the lateral oropharynx walls between the palatoglossal and palatopharyngeal arches B. Tongue - moves food in the mouth for mastication and assists in swallowing 1. Is attached to the hyoid bone and consists of intrinsic skeletal muscle covered with a mucous membrane 2. Extrinsic tongue muscles move the tongue from side to side, in and out 3. Lingual tonsils are found on the root of the tongue 4. A lingual frenulum connects the tongue medially to the anterior floor of the mouth 5. Three types of papillae are on the tongue surface: filiform, fungiform, & circumvallate; all but the filiform have taste buds with chemoreceptors for the perception of taste C. Teeth (dentition) - involved in mechanical breakdown of food; the 32 permanent teeth and their associated structures include: 1. Incisors – 8 front teeth that cut and shear food 2. Canines – 4 pointed side teeth for holding and tearing; both canines and incisors have single roots 3. Premolars (8 bicuspids) & Molars (8) - posterior to the canines; have dental cusps for grinding & crushing food 4. 3rd Molars (4 “wisdom teeth) are the last to emerge, may become impacted is there is not enough room in the jaw 5. A tooth consists of: a. A crown, above the gingiva (gum = mucous membrane surrounding the alveolar processes) b. Neck supports the crown where the it meets the gingiva c. Roots extend through the gingiva and into the dental alveolus (socket) 1) Each socket is lined with a CT periosteum (periodontal ligament) 8 2) Roots are covered with bonelike cementum and attach to the periodontal membrane via the periodontal ligament 3) A root canal, continuous with the pulp cavity, opens to the CT surrounding the root via an apical foramen d. Layers of the tooth include: 1) outer enamel layer of the crown & neck, composed of calcium phosphate (toughest substance in the body) 2) middle bone-like dentin layer, secreted by odontoblasts that line the pulp cavity 3) inner pulp cavity with pulp containing loose CT, blood & lymph vessels, and nerves D. Salivary Glands 1. Secrete saliva, a solvent to cleanse teeth and dissolve food particles. Solutes include a. Salivary amylase - enzyme that hydrolyzes starches to disaccharides b. Lingual lipase - enzyme that is activated by stomach acid and digests fats after food is swallowed c. Mucus, which lubricates the food mass and aids swallowing d. Lysozyme – enzyme that kills bacteria e. Immunoglobulin A (IgA), an antibody that inhibits bacterial growth f. Electrolytes, including Na+, K+, Cl-, phosphate, and HCO3g. pH is about neutral 2. Salivary glands include: a. Numerous intrinsic minor glands in the mucous membranes of the palatal region of the mouth keep the mouth moist b. Glands outside the mouth produce most saliva and transport it to the oral cavity via salivary ducts. These glands include 1) Parotid gland - largest, found below and in front of the ear auricle between the skin and masseter muscle; drains 9 through the parotid duct into mouth. Mumps, caused by a virus, is an inflammation of this gland 2) Submandibular gland - located inferior to the mandible body and covered by the mylohyoid muscle; drains through the submandibular duct 3) Sublingual gland - under the mucous membrane in the floor of the mouth; contains several small ducts that empty into the floor 3. Two types of secretory cells are found in all salivary glands a. Serous cells produce a watery fluid containing digestive enzymes b. Mucus cells secrete thick, stringy mucus c. Cuboidal epithelia cells line salivary gland duct lumina 4. Food stimulates receptors in the mouth, which transmit signals to salivary nuclei in the medulla oblongata and pons, which signal salivary glands to secrete saliva via cranial nerves VII and IX a. Parasympathetic nerves stimulate the production of abundant, thin saliva rich in enzymes b. Sympathetic nerves cause the glands to produce less abundant, thicker saliva with more mucus E. Pharynx (throat) - has both digestive and respiratory functions; composed of skeletal muscle lined with mucous membrane 1. The deeper muscle layer is longitudinally oriented 2. The superficial layer is circular muscle, which is divided into superior, middle, and inferior pharyngeal constrictors that force food downward during swallowing V. Esophagus & Stomach A. Esophagus - portion of the GI tract that connects the pharynx to the stomach. Features: 1. A collapsible tube, about 10 in long, containing smooth and/or skeletal muscle lined with stratified squamous epithelium, 10 2. Starts at the laryngopharynx, posterior to the trachea 3. Is located in the mediastinum and passes through the esophageal hiatus (opening in the diaphragm) just above the stomach 4. Lower esophageal (cardiac) sphincter between esophagus & stomach usually prevents regurgitation of food from stomach 5. Gastroesophageal reflux disease (GERD) involves weakness of the cardiac sphincter; allows stomach acids into the esophagus 6. Deglutition (swallowing) - the swallowing center of the medulla oblongata and pons coordinates and integrates the pharyngeal and esophageal muscles involved. The two phases are a. Buccal phase – tongue collects food, forms a bolus, then pushes it into the oropharynx b. Pharyngeal-esophageal phase – the bolus is driven downward by gravity, pharyngeal muscle contractions and esophageal peristalsis mediated by the myenteric nerve plexus B. Stomach - continuous with the esophagus superiorly and with the duodenum inferiorly. Features are: 1. Receives food bolus from the esophagus, churns it with gastric secretions (e.g.: pepsin & HCl) to form chyme, which then moves it to the duodenum 2. Major regions of the stomach include: a. Cardia - narrow upper region below the cardiac sphincter b. Fundus - dome-shaped region to the left of and in contact with the diaphragm c. Body (corpus) - large central portion d. Pyloris - funnel-shaped terminal portion; a pyloric sphincter regulates the passage of chyme from the stomach into the duodenum 3. Borders of the stomach are: a. Anterior and posterior borders 11 b. Lesser curvature - medial concave border c. Greater curvature – left lateral convex border 4. Stomach walls have all 4 GI tract tunics plus 2 additions: a. An extra oblique muscle layer in the muscularis externa b. Gastric folds (rugae) in the mucosa, which permit stomach distension. The mucosa also contains gastric pits and 5 types of cells in gastric glands within the pits: 1) Mucous cells – found in the neck of the gland; secrete mucous 2) Parietal cells – found mostly in the upper gland; secrete a) HCl a strong acid with a pH as low as 0.8 b) Intrinsic factor, which is necessary for vit. B12 absorption in the small intestine 3) Chief (zymogenic) cells – in lower glands; secrete pepsinogen, the precursor to protein-digesting pepsin 4) Enteroendocrine cells – in lower glands; secrete several hormones, including gut-brain peptides, which coordinate different parts of the GI tract with each other 5) Regenerative (stem) cells – divide to replace cells that die c. B12 deficiency or deficient gastric intrinsic factor leads to pernicious anemia due to insufficient RBC production 5. Gastric secretions produced by the gastric glands total 2-3 L per day, and are composed mostly of water, HCl and pepsin a. HCl is produced with H+ ions liberated from H2CO3 and Clions exchanged for HCO3- ions during a Cl- ion shift. Four functions of HCl are 1) Activates pepsin and lingual lipase 2) Breaks up connective tissues and plant cell walls 3) Converts ingested iron ions to a form that can be absorbed 4) Destroys ingested bacteria and other pathogens b. Pepsinogen is converted to protein digesting pepsin by HCl 12 c. Chemical messengers produced by gastric enteroendocrine cells include 1) Gastrin – stimulates gastric glands to secrete HCl and enzymes 2) Seratonin - stimulates gastric motility 3) Somatostatin – inhibits gastric secretion and motility 6. Gastric motility – stomach movements have two phases a. Receptive-relaxation response – arriving food stretches the stomach, causing it to relax b. Peristaltic contractions of the smooth muscle churns the bolus and mixes it with gastric juices, then moves the chyme through the pyloric sphincter into the duodenum 7. A small amount of digestion and absorption occur in the stomach a. Salivary and gastric enzymes partially digest protein and some starch and fat in the stomach, but most digestion and nutrient absorption occurs in the small intestine b. The stomach does absorb aspirin and some lipid soluble drugs 8. Protection of the stomach is accomplished by 3 mechanisms a. Mucous coat lining the stomach resists acids and enzymes b. Epithelial cell replacement – cells are replaced every 3-6 days c. Tight junctions between the epithelial cells prevent gastric juices from seeping between them and digesting the CT 9. Peptic ulcers can occur if HCL and pepsin erode the stomach wall. The most common cause is infection by the bacterium Heliobacter pyloris, which invades the stomach mucosa 10. Regulation of gastric function is accomplished by the nervous and endocrine systems during three phases a. Cephalic phase – mental and sensory stimuli lead to gastric secretion and motility via the hypothalamus, medulla oblongata, and vagus nerves 13 b. Gastric phase – swallowed food and semidigested protein stimulate gastric activity through short and long reflexes; ACh, histamine, and gastrin stimulate the release of HCl, intrinsic factor, and pepsin c. Intestinal phase – chyme in the duodenum stimulates hormonal and nervous reflexes that 1) Initially stimulate the stomach, then 2) Activate an enterogastric reflex that inhibits the stomach 3) Duodenal enteroendocrine cells secrete secretin, cholecystokinin, and gastric inhibitory peptide, which inhibit gastric activity to slow gastric emptying into the duodenum VI. Liver, Gall Bladder, & Pancreas (accessory organs) A. Liver - largest organ of the body, located beneath the diaphragm 1. The liver is composed of 4 lobes & 2 ligaments a. Falciform ligament separates left & right lobes b. Caudate lobe is near the inferior vena cava c. Quadrate lobe is adjacent to the gallbladder d. Ligamentum teres (round ligament = fetal vein remnant) extends from the falciform ligament to the umbilicus 2. Hepatocytes form hepatic plates that are 1-2 cells thick and separated by capillary spaces (sinusoids) a. Sinusoids are lined with Kupffer cells, macrophagic cells that remove bacteria and debris from the blood b. The plate structures and highly permeable sinusoids allow each hepatocyte to be in direct contact with the blood 3. Hepatic plates form functional units called liver lobules a. At the periphery of each lobule are branches of the hepatic portal vein and hepatic artery; blood from each mixes in the sinusoids and passes from the lobule periphery to the central vein 14 b. The hepatic portal vein carries nutrient rich blood from the digestive organs to the liver lobules, where the blood is processed 1) After a meal, the liver removes glucose, amino acids, iron, vitamins and other nutrients from the blood for metabolism or storage 2) It also removes and degrades hormones, toxins bile pigments, and drugs 3) The liver secretes albumin, lipoproteins, clotting factors, angiotensinogen and other products into the blood 4) Between meals, the liver breaks down glycogen to release glucose into circulation 5) Bile is produced, stored in the gall bladder, the released into the duodenum to emulsify fats after eating d. Bile produced by hepatocytes is secreted into bile canaliculi, then drains into bile ducts at the periphery of each lobule, then into hepatic ducts that carry bile to the gall bladder e. A hepatic triad is formed by a bile duct, hepatic portal vein branch, & hepatic artery branch f. A central vein is in the center of each lobule; central veins of each lobule merge to form the hepatic vein, which carries blood from the liver to the inferior vena cava B. Gallbladder - saclike organ attached inferiorly to the liver. Features include: 1. Bile is secreted by the liver through the hepatic ducts common hepatic duct bile duct ampulla of Vater sphincter of Oddi duodenum after a meal 2. When chyme from the stomach enters the duodenum, bile is secreted there via the bile duct 3. When the small intestine empties, the sphincter of Oddi leading into the duodenum constricts, and bile is forced up the bile duct 15 to the cystic duct and into the gallbladder, which stores and concentrates the bile until it is needed 4. Bile is a greenish fluid containing minerals, cholesterol, fats, phospholipids, bile pigments (e.g., bilirubin), and bile acids (salts). Bile acids emulsify fats in the duodenum 5. Gallstones (biliary calculi) sometimes form & block the bile duct, causing jaundice and poor fat digestion. The gallbladder may require surgical removal (cystectomy) C. Pancreas - positioned transversely along the posterior abdominal wall, between the stomach and duodenum. Features are: 1. The pancreas has 3 sections: a. Head - expanded portion near the duodenum b. Body - central portion inferior and posterior to the stomach c. Tail - tapered part near the spleen d. All but the tail are retroperitoneal 2. It’s a mixed gland, with both endocrine & exocrine functions a. Endocrine hormones are secreted by the pancreatic islets 1) Alpha cells secrete glucagon 2) Beta cells secrete insulin b. Exocrine functions are performed by the pancreatic acini cells 1) Each acinus consists of a single layer of epithelial acinar cells surrounding a lumen into which pancreatic digestive enzymes are secreted 2) Secreted digestive enzymes move through the pancreatic duct to the ampulla of Vater, past the sphincter of Oddi, into the duodenum 3. Pancreatic juice is an alkaline mixture of water, enzymes, sodium bicarbonate, and other electrolytes. Enzymes include a. Trypsinogen, which is converted to trypsin, an enzyme that breaks down proteins to amino acids b. Pancreatic amylase digests starches to monosaccharides c. Pancreatic lipase breaks down fats to fatty acids and glycerol 16 d. Ribonuclease & Dexoyribonuclease digest RNA and DNA D. Regulation of the secretion of bile and pancreatic juice is in response to 1. Sympathetic nerves inhibit secretion 2. Parasympathetic nerves, and the hormones cholecystokinin (CCK), gastrin, and secretin all stimulate secretion a. CCK is secreted by the duodenum in response to acid and fat arriving from the stomach, which triggers 3 responses 1) Gallbladder contracts, forcing bile into the bile duct 2) Pancreatic enzymes are secreted 3) Sphincter of Oddi relaxes, allowing bile and enzymes into the duodenum b. Gastrin from the stomach and duodenum also stimulates gallbladder contraction and pancreatic juice release c. Secretin from the duodenum stimulates the bile duct and pancreatic duct to secrete bicarbonate, which neutralizes stomach acid in the duodenum VII. Small Intestine - located in the abdominal cavity between the stomach pyloric sphincter & ileocecal valve leading into the large intestine A. Mesentery supports the SI and contains blood vessels, nerves, & lymphatic vessels that supply the intestine B. The living small intestine is about 12 ft. long (in a cadaver, it is about 20 ft. long) C. The SI is the main site of nutrient absorption 1. It contains digestive enzymes such as peptidase, sucrase, lipase, amylase, nuclease, & enterokinase 2. It receives digestive enzymes from the salivary glands, gastric glands, and pancreas, as well as bile from the liver D The 3 major regions of the SI are: duodenum, jejunum, & ileum 17 1. Duodenum - first 10 in., from the pyloric sphincter to the duodenojejunal flexure; this is the main site of chemical digestion a. Bile duct delivers bile here from the liver & gall bladder b. Pancreatic duct delivers pancreatic digestive enzymes c. Both ducts unite to form a common entry called the hepatopancreatic ampulla (ampulla of Vater), which drains into the duodenum via the duodenal papilla d. The duodenal papilla is opened and closed by the sphincter of Oddi e. Duodenal (Brunner’s) glands in the submucosa secrete bicarbonate rich mucus and are found only in the duodenum 2. Jejunum - is about 3 ft. long & extends from duodenum to ileum, and has a histological structure like the ileum; this is the main region of absorption of digested food molecules into the blood stream 3. Ileum - terminal small intestine is about 6 ft. long and empties into the cecum through the iliocecal valve. Walls contain many Peyer’s patches lymph nodules, which produce lymphocytes to combat bacteria in the ileum E. Structural Modifications & Microscopic Anatomy of the SI 1. Digested products are absorbed rapidly across the epithelial linings of the intestinal mucosa, primarily in the jejunum, due to modifications that increase the internal surface area a. Plicae circulares are large macroscopic folds of the mucosa b. Villi are fingerlike macroscopic projections of the mucosa that extend into the lumen of the SI 1) Simple columnar epithelium(absorptive cells) & goblet cells cover the villi 2) The lamina propria contains lymphocytes, capillaries (that absorb monosaccharides & amino acids), and lymphatic lacteals (that absorb fatty acids) 18 c. Microvilli (brush border) are microscopic extensions formed by the folding of each epithelial cell membrane 2. Brush border enzymes are integral proteins in the microvilli membrane. a. Enterokinase is one enzyme that activates pancreatic enzymes b. Other enzymes carry out the final stages of enzymatic digestion 3. Intestinal crypts (of Liberkuhn), similar to gastric glands, are found on the floor of the SI, between the bases of the villi a. The upper half of the crypts consists of absorptive and goblet cells b. The lower half contains dividing stem cells, which replace sloughed off epithelial cells every 3-6 days F. Intestinal Motility – 1. Movements of the SI include segmentation and peristalsis a. Segmentation is the formation of ringlike constrictions in the intestine that churns the contents to assist digestion b. Peristalsis is rhythmic contractions of the smooth muscle layers that moves the contents toward the large intestine 2. Contractions of the SI serve three functions a. Mixes chyme the intestinal juice, bile, and pancreatic juice, allowing the fluids to neutralize acid and digest the nutrients b. Churns chyme to bring it into contact with the brush border enzymes for digestion and absorption c. Moves the undigested residue toward the colon VIII. Chemical Digestion & Absorption are complete by the time the food residue leaves the SI and enters the cecum. Carbohydrates, proteins, and fats are degraded and absorbed in the following manner A. Carbohydrate (starch) digestion is accomplished by the following enzymes 1. Salivary amylase begins starch digestion in the mouth and stomach 19 2. Pancreatic amylase continues starch digestion in the small intestine, hydrolyzing it into oligosaccharides and maltose 3. Brush border enzymes dextrinase, glucoamylase, and maltase finish digesting the breakdown products of starch; sucrase and lactase break down sucrose and lactose, respectively B. Carbohydrate absorption of the resulting monosaccharides (glucose, fructose, and galactose) is accomplished in the following manner 1. Monosaccharides can be transported across the apical membrane via the sodium-glucose transport protein (SGLT), facilitated transport, or by solvent drag, in which the molecules are pulled between the cells with water 2. Once inside the epithelial cells, monosaccharides are transported through the basal membrane via facilitated diffusion into the blood capillaries of the villus 3. The nutrients are then delivered to the liver in the hepatic portal vein C. Protein digestion 1. Pepsin begins protein (polypeptide) digestion in the stomach 2. Trypsin and chymotrypsin from the pancreas continue digestion in the SI 3. Brush border enzymes called peptidases (proteases) disassemble the resulting peptides one amino acid at a time D. Amino acid absorption is accomplished in a manner similar to that of monosaccharides (sodium cotransport facilitated diffusion blood capillaries hepatic portal vein liver). E. Fat digestion 1. Begins with lingual lipase in saliva, activated in the stomach 2. Most fat (triglyceride) is digested by pancreatic lipase in the SI 3. Bile acids and lecithin help break fat into emulsification droplets 20 4. Lipase hydrolyzes the fats into free fatty acids and monoglycerides, which collect with cholesterol and fat soluble vitamins in bile-coated droplets called micelles. F. Fat absorption 1. Micelles transport the lipids into the intestinal absorptive cells 2. The absorptive cells repackage the fats into chylomicron droplets coated with phospholipid and protein 3. Chylomicrons are secreted from the absorptive cells and taken into the lacteal in the villus 4. Chylomicrons travel in lymph in the lymphatic vessels and enter the bloodstream at the subclavian veins G. Dietary DNA & RNA are 1. Hydrolyzed into nucleotides (composed of sugar, phosphate, and nitrogenous base) by pancreatic nucleases, then by brush border nucleosidases and phosphatases 2. Ribose, deoxyribose, phosphate, and nitrogenous bases are transported across the cell membrane and into the blood capillaries of the villus H. Vitamins are not digested; they are absorbed unchanged 1. Fat-soluble vitamins (A, D, E, K) are absorbed with other lipids 2. Most water-soluble vitamins (B complex and C) are absorbed by simple diffusion; 3. Vitamin B12 binds to intrinsic factor, and is then absorbed by receptor mediated endocytosis I. Minerals (electrolytes) are absorbed by 1. Na+ is cotransported with sugars and amino acids 2. Cl- & Fe2+ are absorbed by active transport 3. K+ & Ca2+ are absorbed via simple diffusion 21 J. Water is absorbed by osmosis, following an osmotic gradient established by the absorption of salts and organic nutrients IX. Large Intestine A. About 5 ft. long, it begins at the ileocoecal valve, and ends at the anus B. Functions to absorb water & electrolytes; form, store, & expel feces C. The Large Intestine is divided structurally into the cecum, colon, rectum, and anal canal 1. Cecum is a dilated pouch slightly below the ileocoecal valve; the fingerlike appendix extends from the inferior medial cecum 2. The colon extends from the cecum and consists of 4 parts: a. Ascending colon - ascends from the cecum along the right abdominal wall to the liver b. Transverse colon - extends across the body from the right colic (hepatic) flexure to the left colic (splenic) flexure c. Descending colon - descends along the left abdominal wall to the pelvic region d. Sigmoid colon - S-shaped colon from the descending colon to the rectum 3. Rectum - about 7.5 in. terminal portion of the GI tract. The last inch is called the 4. Anal canal, which has the anus opening regulated by two sphincters a. Internal anal sphincter - composed of smooth muscle b. External anal sphincter - composed of skeletal muscle 5. The large intestine has the 4 GI tract tunics with some modifications: 22 a. Lacks villi but has many goblet cells in the mucosal layer b. The longitudinal muscle layer forms 3 bands called taeniae coli that run the length of the LI c. Bulges in the LI walls form sacculations (haustra) d. Fat-filled pouches called epiploic appendages are attached to the taeniae coli D. Bacterial Flora & Intestinal Gas 1. The large intestine contains numerous species of bacteria, collectively called bacterial flora 2. Bacteria ferment cellulose, other undigested carbohydrates, and fats; they also synthesize B vitamins and vitamin K, necessary for blood clotting 3. The average person expels about 500 ml of flatus (gas) per day E. Defecation is facilitated by the following reflexes 1. Stretching of the rectum triggers the intrinsic defecation reflex, mediated by the nyenteric nerve plexus, which drives feces downward and relaxes the internal anal sphincter 2. A stronger parasympathetic defecation reflex involves a reflex arc through the spinal cord and parasympathetic fibers of the pelvic nerve 3. These reflexes cause defecation, although voluntary control of the external anal sphincter can prevent defecation IX. Disorders of the Digestive System A. Viral Hepatitis – long term liver inflammation; 3 major types: 1. Hepatitis A – spread by fecal-oral route; does not usually cause permanent damage; preventive vaccines available 2. Hepatitis B – transmitted by infected blood or body fluids; infection can lead to liver cancer; preventive vaccine available 3. Hepatitis C – transmitted by body fluids; no short term symptoms; can lead to cirrohosis and liver cancer; no vaccine 23 B. Pancreatitis – inflammation of the pancreas C. Diverticulitis – inflammed herniations (diverticula) of the colon, which can rupture. Associated with low fiber diets D. Crohn disease – inflammation of the small and large intestines, producing granular lesions and fibrosis of the intestines, diarrhea, and lower abdominal pain