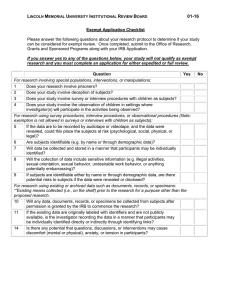
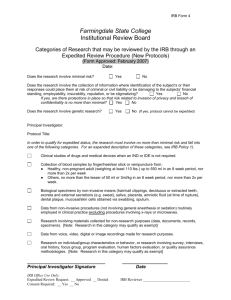
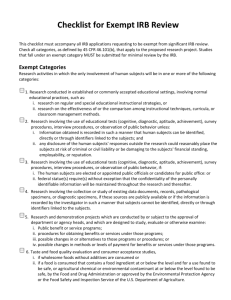
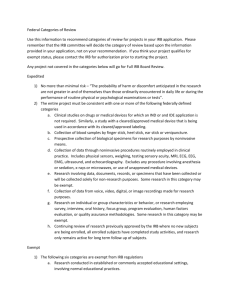
Summary Table of Review Types and Review Type Algorithm: Exempt, Expedited, Full Board
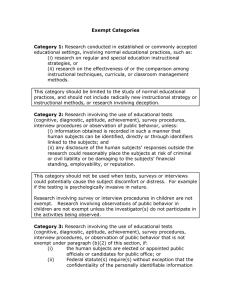
advertisement

Review Type Overview of Non-Human Subject Research, Exempt Research, Non Engaged in Human Subject Research and Expedited Research For Researchers Criteria apply if research is conducted, supported or otherwise subject to regulation by any federal department or agency OR FWA states institution will follow regulations regardless of funding. Non-Human Subject Research Exempt 45 CFR46.102 21CFR50 45 CFR 46.101 21CFR56.104 (a-d) NOT considered Human Subject Research under DHHS regs or a Clinical Investigation via FDA regs Determination of Human Subject Research Form is optional IRB Submission Required Considered Human Subject Research Non Engaged in Human Subjects Research OHRP Guidance on Engagement of Institutions in HSR This is a DHHS guidance. Does NOT apply for FDA regulated research. IRB Submission Required Considered Human Subject Research Apply only if protocol involves humans subjects and does not meet exempt criteria Need outside IRB approval under which data/ specimens were collected if data/ specimens come from outside UVa. If FDA regulated research, and samples/data come from outside of UVa, the UVa researchers must be included as personnel on IRB protocol at outside institution- need an IRB Reliance Agreement. Expedited 45 CFR 46.110 and 21 CFR 56.110. IRB Submission Required Considered Human Subject Research Apply only if protocol does not meet exempt or not engaged criteria Page 1 of 4 Version Date: 02/06/16 Non-Human Subject Research Criteria Project does not meet both definitions below: (1) Research means a systematic investigation, including development, testing, and evaluation, designed to develop or contribute to generalizable knowledge. Activities which meet this definition constitute research for the purposes of this policy, whether or not they are supported under a program which is considered research for other purposes. Exempt Criteria Must meet one of the Exempt Criteria below: Additional exempt criteria exist for nonbiomedical research (1) Research involving the collection of existing data, documents, records, pathological specimens, or diagnostic specimens (2) Human subject means a living individual about whom an investigator conducting research obtains (1) data through intervention or interaction with the individual, or (2) identifiable private information. Existing data means all the data, documents, records or specimens are in existence prior to IRB-HSR review; therefore cannot be obtained prospectively (future) OR (2) These sources (data, specimens, records etc..) are publicly available OR the information is recorded by the investigator without identifiers directly or indirectly linking back to the subject Criteria met from OHRP Guidance on Research Involving Coded Private Information or Biological Specimens Criteria #1 and #2 must BOTH apply: (1) The private information or specimens were NOT collected specifically for the currently proposed research project through an interaction or intervention with living individuals AND (2) The investigator(s) cannot readily ascertain the identity of the individual(s) to whom the coded private information or specimens pertain. ( see LINKS below) Links If a link to individually identifying information is kept one of the following must apply The consultants or collaborators and the holder of the key enter into an agreement prohibiting the release of the key to the consultants or collaborators under any circumstance. The releasing institution has IRB-approved written policies and operating procedures applicable to the research project that prohibit the release of the key to the consultants or collaborators under any circumstance; or There are other legal requirements prohibiting the release of the key to the consultants or collaborators Both # 1 and 2 must be met in order for the project to be exempt. (3) Research involving the use of educational tests, survey, interview or observation of public behavior. If doing research involving the use of educational tests, survey, interview or observation of public behavior, identifiers can be recorded, however, if subjects can be identified directly or through links/codes AND any disclosure of the subject’s responses would place the subject at risk of criminal or civil liability or be damaging to the subject’s financial standing, employability or reputation, the study would NOT qualify for exempt approval Non Engaged in Human Subjects Research Criteria #1 and #2 must BOTH apply: (1) Process includes a non-engaged scenario AND does not include an engaged scenario ( see application form) (2) If scenario # 7 is chosen- the investigator(s) cannot readily ascertain the identity of the individual(s) to whom the coded private information or specimens pertain. ( see LINKS below) Links If a link to individually identifying information is kept one of the following must apply The key must be destroyed before the research begins or Signed agreement is required between the person releasing the data and the investigator receiving it stating the code will never be released or Confirmation from another IRB for a repository or data center states that the release of the code is strictly prohibited Expedited Criteria #1 and #2 must BOTH apply: (1) No more than minimal risk to human subjects, and (2) Involve only procedures listed in one or more of the following categories: 1. Clinical studies of drugs and medical devices only when condition (a) or (b) is met. (a)Research on drugs for IRB-HSR an IND application is not required. (Note: Research on marketed drugs that significantly increases the risks or decreases the acceptability of the risks associated with the use of the product is not eligible for expedited review.) (b)Research on medical devices for IRB-HSR (i) an IDE is not required; or (ii) the medical device is cleared/approved for marketing and the medical device is being used in accordance with its cleared/approved labeling. 2. Collection of blood samples by finger stick, heel stick, ear stick, or venipuncture as follows: 2(a) from healthy, non-pregnant adults who weigh at least 110 pounds; amounts drawn may not exceed 550 ml in an 8 week period and collection may not occur more frequently than 2 times per week; or \ 2(b) from other adults and children, the amount drawn may not exceed the lesser of 50 ml or 3 ml per kg in an 8 week period and collection may not occur more frequently than 2 times per week. 3. Prospective collection of biological specimens for research purposes by noninvasive means. Examples: hair and nail clippings in a non-disfiguring manner; 4. Collection of data through noninvasive procedures (not involving general anesthesia or sedation) routinely employed in clinical practice, excluding procedures involving x-rays or microwaves. Examples: MRI; ECHO, Doppler blood flow,; moderate exercise, muscular strength testing, 5. Research involving materials (data, documents, records, or specimens) that have been collected, or will be collected solely for non-research purposes (such as medical treatment or diagnosis). 6. Collection of data from voice, video, digital, or image recordings made for research purposes. 7. Research on individual or group characteristics or behavior Note: If done under an FDA application must have an IRB AA in place confirming outside IRB approval of the original collection of the specimens/ data Page 2 of 4 Version Date: 02/06/16 Non-Human Subject Research Exempt Non Engaged in Human Subjects Research Expedited Examples include: Research with data/ specimens from cadavers Case Reviews ( up to 3) Cell lines Specimens purchased from commercial supplier. No intervention/interaction and #1 and #2 both must apply Examples include: Questionnaires or surveys that do collect information in a way that the subject can be identified. Research being conducted in educational settings involving normal curriculum, Research on archival data Research involving an investigational test article under Emergency Use Chart review of data from medical records of year 2004-2007 and data will be recorded in a way that the subject cannot be identified Examples include: Researcher working on the same research study with a colleague from another institution. All subjects are enrolled and seen at outside institution. Our researcher is sent coded samples for analysis. Analysis results returned to primary institution. Our researcher will never be given the identity of the subjects. Examples include: Prospective chart review and recording identifiers Blood draw (meets additional criteria required by expedited category) from peripheral needle stick ECGs use of otherwise discarded tissue obtained for clinical purposes during a clinical procedure (no extra tissue, fluid etc. taken for the research) use of banked specimens for minimal risk research (e.g. no testing of polymorphisms) database is being developed that contains data gathered from existing sources such as the medical record and data has identifiers (1) Material/data was collected for purposes OTHER than this research project (e.g., normal discarded tissue) or for unrelated research project with no extra material collected for this project (2) Material/data is given to the investigator WITHOUT A CODE and NO CODE is kept by the receiver or sender. NOTE: Must also review HIPAA regulations: need DUA if LDS or Waiver of HIPAA Authorization if collecting identifiable information. If sharing identifiable data outside of UVa must do tracking. – Protocol may be approved under exempt review if data/ specimens are not considered Identifiable per HIPAA regulations. May also be approved under exempt review if data/ specimens meet the criteria of a Limited Data Set. No intervention/ interaction by researcher #1 and #2 both must apply (1) Material/data was collected FOR purposes of the research project in question and NOT collected for purposes other than this research project. (2) Material/data is given to the investigator WITH A CODE; however, the investigator receiving the data/material will NEVER have access to the key to the code OR the key cannot be derived from or related to information about the subject-if there is a key. Our institution performing commercial services for the researchers Our institution providing clinical trial related medical services as dictated by the protocol that are part of routine clinical care. Informing patients about other clinical trials, providing consent form but NOT obtaining consent. More scenarios found in OHRP guidance. Page 3 of 4 Version Date: 02/06/16 Not allowed: Any examples found in all subsequent columns. Not allowed: Collecting identifiable info from two different sources (medical record, pharmacy log) since this would require HIPAA identifiers to link info from both sources. Surveys or interview collecting information that may be of risk to a subject and are collected in a manner that a subject may be identified. Observation of minors Deception Not allowed: Data/ specimens were collected for other non- related research Data/ specimens will be given to the researcher along with the key to the code The researcher is working on both studies: the protocol collecting the data/ specimens and the new study Not allowed: small amount of additional fluid, tissue is being collected for research purposes and the collection method itself presents greater than minimal risk (collection of additional CSF, biopsy tissue etc) randomization to one of several approved drugs/devices throat swab unless full board determines the study is minimal risk (board may determine throat swab is minimal risk if swab obtained by a licensed health care professional) oral glucose tolerance test induced sputum, skin biopsy imaging studies ( except MRI without contrast) collection of identifiable sensitive information without a certificate of confidentiality anything is being introduced into an orifice solely for research, Examples: pap smears, ear probes that are inserted further into the ear than the entrance of the auditory canal; rectal swabs, anything being placed into the nose farther than a finger could go blood samples for research are being collected from a central or arterial line or an existing peripheral line ( unless Full Board determines study is minimal risk) additional CSF is being collected from an existing shunt or externalized CSF drain. assessments, surveys or questionnaires of a sensitive nature where HIPAA identifiers will be retained databases that contain sensitive information that is identifiable and NO Certificate of Confidentiality will be sought Page 4 of 4 Version Date: 02/06/16