C B -W G
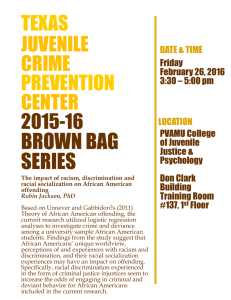
advertisement

CLOSING THE BLACK-WHITE GAP In the United States, Black infants have significantly worse birth outcomes than White infants. Over the past decades, public health efforts to address these disparities have focused primarily on increasing access to prenatal care, however, this has not led to closing the gap in birth outcomes. We propose a 12-point plan to reduce Black-White disparities in birth outcomes using a life-course approach. The first four points (increase access to interconception care, preconception care, quality prenatal care, and healthcare throughout the life course) address the needs of African American women for quality healthcare across the lifespan. The next four points (strengthen father involvement, systems integration, reproductive social capital, and community building) go beyond individual-level interventions to address enhancing family and community systems that may influence the health of pregnant women, families, and communities. The last four points (close the education gap, reduce poverty, support working mothers, and undo racism) move beyond the biomedical model to address the social and economic inequities that underlie much of health disparities. Closing the Black-White gap in birth outcomes requires a life course approach which addresses both early life disadvantages and cumulative allostatic load over the life course. (Ethn Dis. 2010;20 [Suppl 2]:s2-62–s2-76) Key Words: Life Course Perspective, Disparities, Birth Outcomes, Programming, Allostatic Load, Preconception Care, Prenatal Care, Quality, Father Involvement, Systems Integration, Social Capital, Maternity Leave, Childcare, Racism From the Departments of Obstetrics and Gynecology (MCL) and Pediatrics (NH), David Geffen School of Medicine at UCLA; the Department of Community Health Sciences and the Center for Healthier Children, Families and Communities, UCLA School of Public Health (MCL, NH) and Department of Maternal and Child Health, Boston University School of Public Health (MK) and Department of Maternal and Child Health, University of North Carolina at Chapel Hill (VH) and Healthy African American Families, Los Angeles, CA (LJ) and UCLA School of Nursing (KW). Address correspondence or reprint request to Michael C. Lu, MD, MPH; Department of Community Health Sciences; UCLA School of Public Health; Box 951772; Los Angeles, CA; 90095-1772; 310-825-5297; 310-794-1805 (fax); mclu@ucla.edu S2-62 IN BIRTH OUTCOMES: A LIFE-COURSE APPROACH Michael C. Lu, MD, MPH; Milton Kotelchuck, PhD, MPH; Vijaya Hogan, DrPH; Loretta Jones, MA; Kynna Wright, PhD, MPH; Neal Halfon, MD, MPH In the United States, Black infants are more than twice as likely to die within the first year of life as a White infant, a gap that has not substantially closed in over half a century.1,2 A significant portion of the disparity in infant mortality is attributable to the near two-fold increased rates of low birth weight (LBW) and preterm births, and the near three-fold increased rates of very low birth weight (VLBW) and very preterm births, among Black infants.3 The cause of racial disparities remains largely unexplained. Most studies focus on differential exposures to risk and protective factors during pregnancy, such as maternal behaviors,4 prenatal care utilization,5 psychosocial stress6 or infections.7 These factors however do not adequately account for the racial gap in birth outcomes.8,9 Lu and Halfon10 recently proposed an alternative approach to examining racial-ethnic disparities in birth outcomes using the life course perspective. The life course perspective conceptualizes birth outcomes as the end product of not only the nine months of pregnancy but the entire life course of the mother before the pregnancy. Disparities in birth outcomes, therefore, are the consequences of both differential exposures during pregnancy and differential developmental trajectories across the life span. The life course perspective synthesizes two longitudinal models: an early programming model and a cumulative pathways model.11,12 The early programming model posits that early life exposures influence future reproductive potential. For example, perinatal stress is associated with high stress reactivity that persists into adulthood.13–15,17,18 This, in turn, may be related to feedEthnicity & Disease, Volume 20, Winter 2010 back resistance from altered expression of glucocorticoid receptors in the developing brain.16 Exposure to stress hormones during sensitive periods of immune maturation in early life may also alter immune function, leading to increased susceptibility to infectious or inflammatory diseases later in life.19 Hypothetically, maternal stress during pregnancy could prime fetal neuroendocrine and immune systems with stress hormones, leading to higher stress reactivity and immune-inflammatory dysregulation that could increase a female offspring’s vulnerability for preterm labor and LBW later in life. Thus the increased risk of African American women to preterm birth and LBW may be traced to greater exposures to stress hormones during pregnancy, early life, and possibly even in utero. The cumulative pathways model proposes that chronic accommodation to stress results in wear and tear, or allostatic load,20 on the body’s adaptive systems, leading to declining health and function over time. Animals and humans subjected to chronic and repeated stress have elevated basal cortisol levels and exaggerated hypothalamic-pituitary-adrenal (HPA) response to natural or experimental stressors.21,22 This HPA hyperactivity may reflect the inability of a worn-out system for self-regulation, possibly due to loss of feedback inhibition via down-regulation of glucocorticoid receptors in the brain.21 Chronically elevated cortisol levels may also lead to immune suppression and immune-inflammatory dysregulation. 23 HPA hyperactivity and immune-inflammatory dysregulation are two of several possible mechanisms by which chronic and repeated stress over the life course may lead to increased vulnerability to preterm labor caused by stress or CLOSING GAP IN BIRTH OUTCOMES - Lu et al Table 1. A 12-point plan to close the Black-White gap in birth outcomes: A lifecourse approach 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Provide interconception care to women with prior adverse pregnancy outcomes Increase access to preconception care to African American women Improve the quality of prenatal care Expand healthcare access over the life course Strengthen father involvement in African American families Enhance coordination and integration of family support services Create reproductive social capital in African American communities Invest in community building and urban renewal Close the education gap Reduce poverty among African American families Support working mothers and families Undo racism infection. This model suggests the increased risk of African American women for preterm birth and LBW may be related to increased exposures to stress during pregnancy and possibly to increased weathering of stress over their life course, resulting in greater allostatic load which may already be present before pregnancy.24 The life course perspective suggests that closing the Black-White gap in birth outcomes requires more than improving access to prenatal care for African American women. From this perspective, it is not surprising that our national and state policies over the past two decades have not been more successful in closing the racial gap in birth outcomes. To expect prenatal care, in less than nine months, to reverse the lifelong, cumulative impact of social inequality on the health of African American mothers, may be expecting too much of prenatal care. Closing the racial gap in birth outcomes requires a life course approach, addressing both early life disadvantages and cumulative allostatic load. The purpose of this commentary is to propose this life course approach. We recognize we do not know all life course factors related to the disparities nor have all the answers to address them, but we believe we must do something. We present a platform of what we can do now – a 12-point plan building on previous work25 and a literature search for promising strategies. The 12 points are summarized in Table 1. The goals are to: 1) improve healthcare for African American women; 2) strengthen African American families and communities; and 3) address social and economic inequities that create a disproportionate toll on the health of African American women over their life course. This plan departs from current approaches to create a new paradigm for closing the racial/ethnic gap in birth outcomes. First, it goes beyond prenatal care and addresses healthcare needs of African American women from preconception to interconception and across the life course. Second, it goes beyond individual-level interventions and addresses family and community systems. Third, it goes beyond the medical model and addresses social and economic inequities that underlie much of health disparities. While a life course approach is needed to address health disparities in any community, we focus our discussion on its application in the African American community given the disproportionate burden of infant mortality and other poor maternal and child health (MCH) outcomes borne by that community. IMPROVING HEALTHCARE FOR AFRICAN AMERICAN WOMEN While health care alone cannot close the gap, it is a good place to start. Ethnicity & Disease, Volume 20, Winter 2010 Health care has a vital role, especially if provided over the woman’s life course, and not only during pregnancy. The right health care can promote positive development in early life and reduce cumulative allostatic load over the life course. Expanding access to interconception care, preconception care, quality prenatal care, and health care over the life course are important strategies in closing the racial gap in birth outcomes. Provide Interconception Care for Women with Prior Adverse Pregnancy Outcomes Interconception care allows for continuity of health care from one pregnancy to the next.26 Ideally interconception care should be provided to all women between pregnancies as part of comprehensive women’s health care. However, given resource constraints, it could be initially targeted to women with prior adverse pregnancy outcomes (ie, preterm birth, LBW, intrauterine growth restriction, fetal or infant death). Women with a poor pregnancy outcome are at substantial risk for having another poor pregnancy outcome.27,28 Many biobehavioral risk factors for preterm birth are carried from one pregnancy to the next. The interconception period offers an important window of opportunity for addressing these risk factors and optimizing women’s health before their next pregnancy. However, present access to health care in the interconception period is limited for many African American women, particularly low-income women whose pregnancy-related Medicaid coverage generally terminates at sixty days postpartum.26 African American women would benefit more from interconception programs given their greater risk from prior adverse pregnancy outcomes and less access to health care during the interconception period. There have been several interconception care demonstration projects, most notably programs in Atlanta, Denver, Jacksonville, Philadelphia, and S2-63 CLOSING GAP IN BIRTH OUTCOMES - Lu et al several Healthy Start sites.29,30 Since 2005, Healthy Start programs are required to include an interconception care component. The interconception care program in Denver was shown to reduce the risk of recurrent LBW births by one-third, though this finding must be interpreted with caution because of potential selection bias. Most interconception programs consist of four components: risk assessment, health promotion, medical and psychosocial interventions, and outreach and case management. The initial risk assessment should be comprehensive to detect factors associated with adverse birth outcomes, including expert review of medical records. Risk assessment should be on-going throughout the interconception period, and help guide development of an individualized care plan for health promotion and medical/psychosocial interventions. Core services should include family planning,31,32 screening for maternal depression and intimate partner violence, assessing social support for the pregnant woman, smoking cessation and substance treatment programs, physical activity and nutritional education and intervention, management of chronic diseases, and education on back-to-sleep and parenting skills. The individualized interconception care plan should also address known biobehavioral pathways to a particular outcome. For example, in preventing recurrent preterm birth, interventions should consider neuroendocrine, infectious-inflammatory, vascular, and behavioral pathways to recurrence.33 Potential strategies may include those that reduce chronic stress and increase social support, 34,35 decrease chronic infections, 36,37 restore immune allostasis,38,39 address vascular causes40 and improve health-promoting behaviors.41 Arguably, many interventions could be adopted on the basis of promoting women’s health alone, even in the absence of data on their effectiveness in preventing recurrence of adverse birth S2-64 outcomes.42,43 The program should be multi-level and include communitylevel interventions promoting interconception care. Interconception care programs could be funded through a Medicaid waiver, expansion of State Children’s Health Insurance Program (SCHIP) to cover adult family members, increased scope of services for Title X or state family planning programs, or direct funding from Title V or non-governmental sources. While more work is needed to explore financing, content, and cost-benefit of interconception care, it is an important first step to move us beyond current focus on prenatal care and toward a more expanded, longitudinally-integrated approach for addressing disparities in birth outcomes. Increase Access to Preconception Care for African American Women As with interconception care, the goal of preconception care is to restore allostasis and optimize women’s health prior to pregnancy. Many pathophysiologic processes leading to adverse pregnancy outcomes may have their onset early in pregnancy. For example, an infection associated with preterm delivery may be present in the urogenital tract before pregnancy.43 If it is not cleared by midgestation, preterm labor or preterm premature rupture of membranes may ensue. Screening for and treating bacterial vaginosis (BV) with antibiotics during pregnancy may be less effective in preventing preterm birth. This may partially explain the disappointing results of several antibiotic trials in pregnancy.44,45 Even if the infection is treated, it may be too late to stop immune-inflammatory processes. Preconception care provides an important opportunity to treat ongoing infection and restore immune allostasis. Most models of preconception care were developed with the primary aim of preventing congenital anomalies.46 Further research is needed to develop Ethnicity & Disease, Volume 20, Winter 2010 preconceptional strategies for preventing preterm births and LBW by addressing stress reduction, social support, immune response, chronic infections, inflammation, and behavioral and nutritional risk factors. Recruiting women into preconception care programs without a specific intervenable event and a targetable time period may be difficult.47 Targeting preconception care to couples actively planning a pregnancy will miss about half of all live births unintended at conception.48 Therefore, preconceptional health promotion and disease prevention should be integrated into a continuum of care throughout the life cycle.48 Every routine visit by any woman who may become pregnant at some time should be viewed as an opportunity to provide preconception care.49 Public health efforts should focus on increasing access to, setting standards for, and assuring quality of preconception care. Since Medicaid covers about half (51%) of African Americans with family incomes below the poverty level and 17% of those between 100% and 199% of the poverty level (near-poor),50 expanding Medicaid to cover preconception care could substantially increase access for low-income African American families. Another 15% of the poor and nearly half (48%) of the near-poor African Americans have job-based insurance;50 mandating or subsidizing job-based health insurance coverage of preconception care could further increase access. These expansions will still leave out three in ten African American women who are uninsured.50 Strategies must also consider how to provide preconceptional education and services to adolescents (eg, school-based clinics or family planning programs). The surest way to increase access to preconception care is through a national health insurance program which provides coverage for comprehensive women’s health care. More work is still needed to explore the financing, standards, and quality CLOSING GAP IN BIRTH OUTCOMES - Lu et al assurance for preconception care. In 2005, the Centers for Disease Control and Prevention (CDC) issued recommendations to improve preconception health and health care.51 These recommendations begin to lay out a roadmap toward universal preconception care in the United States. We believe ‘‘preconception care, focusing on women’s overall health … prior to pregnancy, will serve as a key component of the next wave of low-birthweight and infant mortality reduction strategies – and may provide increased savings beyond those experienced from prenatal care alone.’’52 We join the call for this nation to make ‘‘a commitment to advance preconceptional services to a similar extent as it has prenatal care.’’52 Improve the Quality of Prenatal Care for African American Women The life course perspective sees prenatal care as vitally important, both as part of the continuum of health care for the mother, and as the starting point for the child’s developmental trajectory. It recognizes the potential contributions of prenatal care to optimal developmental programming of the baby’s vital organs and systems. For example, poor glycemic control in mothers with pregestational or gestational diabetes has been linked to suboptimal fetal development of pancreatic beta-cell structures and functions and greater adult susceptibility for insulin resistance and diabetes.53 By promoting optimal antenatal glycemic control, prenatal care may reduce intergenerational transmission of insulin resistance and diabetes. Thus prenatal care has an important role in closing the racial gap in not only birth outcomes but possibly in health and developmental outcomes over the life course and across generations. Over the past decade, the racial gap in access to prenatal care has been closing. Today nearly 95% of African American women access prenatal care at some point during pregnancy; three in four do so in the first trimester.3 However, little has been done to close the racial gap in the quality of prenatal care. More than one-third of US women reported receiving no advice on tobacco or other substance use during prenatal care.54 Black women were significantly less likely than White women to receive health behavior advice from prenatal care providers, and women who received insufficient health behavior advice were at higher risk of delivering a LBW infant.54,55 Other studies have documented similar racial gaps in the quality of prenatal care.56 Quality is also determined by the availability of services. Many ancillary services (eg, childbirth education classes, mental health or periodontal services, breastfeeding support), are often unavailable or in short supply in underresourced African American communities. One promising strategy for improving prenatal care quality is the Breakthrough Series (BTS), which uses a collaborative learning model and rapid Plan-Do-Study-Act (PDSA) cycles to bring about quality improvement.57 The effectiveness of the BTS for quality improvement has been demonstrated in other areas of healthcare,66,67 and is now being applied to prenatal care through on-going collaboratives in Vermont and Los Angeles.68 The BTS takes established, but not routinely implemented, clinical standards or best practices and brings together healthcare providers to examine care processes and make them better through rapid cycles of change. Already established clinical standards related to prenatal care include screening and referral for smoking,58 substance use,59 poor nutrition,60 intimate partner violence,61 and maternal depression,62 just to name a few. More research is needed to evaluate whether other practices, such as infection screening and treatment (eg, asymptomatic BV,63 periodontal disease37) or progesterone treatment64,65 can be recommended as clinical stanEthnicity & Disease, Volume 20, Winter 2010 dards. There is also a need to reconvene a national consensus meeting on the content of prenatal care, as none has been convened since the mid-1980s.69 Assuring availability of important ancillary services is another important step in prenatal care quality improvement. Expand Healthcare Access over the Life Course for African American Women Closing the Black-White gap in birth outcomes requires improving access to quality health care over the life course. Approximately one in five African American children are uninsured, and one in four non-elderly African American women are uninsured, rates nearly twice those for nonHispanic whites.50 Uninsured African Americans are more than three times as likely to be without a usual source of care, and more than twice as likely not to have met minimum standards for physician visits, compared to those with private or Medicaid coverage.50 Among uninsured African Americans, one in ten aged 0 to 5 years, one in five aged 6 to 17, and one in five women in fair or poor health fail to meet minimum standards for regular check-ups.50 The lack of access to preventive and primary care among the uninsured can cause delayed diagnosis and treatment of chronic diseases (eg, hypertension) or maintenance of risk behaviors (eg, cigarette smoking, poor nutrition), resulting in a greater cumulative physiologic toll over the life course and increased biobehavioral vulnerability to adverse perinatal outcomes. Low family incomes are the primary reason for the relative lack of health insurance coverage among African Americans.50 Medicaid covers only half of African Americans in poor households, and only 17% of African Americans in near-poor households. Only 16% of African American women ages 18 to 64 receive Medicaid despite that nearly one-fourth (23%) are poor and nearly one-half (45%) are near poor. S2-65 CLOSING GAP IN BIRTH OUTCOMES - Lu et al Thus expanding Medicaid coverage for poor and near-poor families can be an important strategy for increasing healthcare access for African American women. States have many options, though limited funding, to expand Title XIX Medicaid coverage for uninsured populations.50 The family coverage option of section 1931 of the Social Security Act allows states considerable flexibility in setting income eligibility for Medicaid to cover parents and children above the federal poverty level. Section 1115 allows states to obtain federal waivers to restructure Medicaid programs and enable uninsured adults without children, and families above the current income eligibility limits, to buy into the program on a sliding scale. African Americans are more likely to work in settings (ie, large businesses) that provide access to employment-based health insurance, but they are less likely than Whites in comparable settings to receive such coverage.50 An employer mandate to cover all employees and their dependents would substantially close the racial gap in job-based health insurance coverage. But neither Medicaid expansion nor an employer mandate will provide universal coverage, leaving a large number of African American women and families still uninsured or underinsured. We join the call for a national health insurance program to provide universal, comprehensive coverage to all Americans over their entire lifespan.70 Healthcare access is not all about health insurance. In an increasingly diverse nation, there is also need for increased diversity and linguistic and cultural competence in the health workforce.71–73 Cultural competency and respect for diversity are learned. The work of healthcare providers increasingly requires communication and interaction with people of diverse backgrounds. The training ground for acquiring the skills of an effective practitioner in a diverse society begins in medical, nursing, and other allied health schools, universities, or earlier. Increased diversity in the S2-66 faculty and student body of these schools would provide the level of interaction with diversity necessary to create a culturally competent health workforce.74 We support programs and opportunities that increase the diversity of the medical workforce. STRENGTHENING AFRICAN AMERICAN FAMILIES AND COMMUNITIES Families and communities can be important sources of support and resiliency, but also causes of stress and vulnerability, for pregnant women and their children. Being the head of a single-parent household with little or no father involvement, dealing with fragmented systems to get unfriendly family support services, living in neighborhoods where neighbors do not know or look after one another, and residing in communities with concentrated poverty, high crime rate, poor housing, no parks, limited bus services, and inadequate day care add to the daily wear and tear many African American mothers experience. Closing the racial gap in birth outcomes will take more than improving healthcare; it requires strengthening father involvement, enhancing service coordination and systems integration, creating reproductive social capital, and investing in community building and urban renewal. In short, it will take strengthening family and community support for African American mothers. Strengthen Father Involvement in African American Families Fathers can be a vital source of support for the mother and resiliency for the child. Yet today many African American men do not stay involved in the pregnancies they caused, nor in raising the children from these pregnancies. In 2006, more than 70% of African American infants were born to unmarried mothers, up from 22% in 1960.3 Ethnicity & Disease, Volume 20, Winter 2010 Among poor African American infants, approximately one-third are born into single-mother families with little or no father involvement.75 More than half (53%) are born into so-called fragile families. 75 While many unmarried fathers may be actively involved at birth, over time their involvement declines. Today nearly half (49%) of all poor African American children grow up in single-mother families with little or no father involvement.75 While father absence is not unique to the African American community, its toll on African American women and children is especially high. Studies have shown that, controlling for parental education, income and other confounding factors, children growing up in father-absent families are at greater risk for various educational or behavioral problems and poorer developmental outcomes.80 Father involvement is discussed in detail elsewhere in this issue.76 To strengthen father involvement in African American families, both an ecological approach81 and a life course perspective10 are needed. An ecological approach addresses barriers to father involvement at multiple levels. At the individual level, fathers need educational programs, employment-related services, and legal and social services.82 At the interpersonal level, efforts should focus on improving the relationships between African American men and women, including marriage counseling, family therapy or skills training in communication and conflict resolution. At the neighborhood and community level, interventions must address high rates of unemployment and incarceration among African American. At the institutional level, many African American churches, universities, and media have taken leadership roles in the fatherhood movement, but more need to do so.78 These institutions can help promote changes in norms, values and expectations that support marriage and strengthen the father-child bond. Healthcare providers also have an im- CLOSING GAP IN BIRTH OUTCOMES - Lu et al portant role in supporting fathers’ involvement in their family’s healthcare.83 At the policy level, public policy needs to support the ability of fragile families to stay together. Current policies often do the opposite. Policy reforms are needed to remove disincentives for father involvement in Temporary Assistance for Needy Families (TANF) (ie, eliminating the distinction between single- and two-parent families for eligibility), Earned Income Tax Credit (EITC) (ie. allowing a second-earner deduction), and child support (eg, establishing amnesty programs or extending TANF, EITC, and other support services to non-custodial fathers who pay child support).84,85 Most importantly, increasing economic opportunities by promoting full and consistent employment, job skills training and retraining, fair trade, and unionization will help restore Black fathers to Black families.77–79 The life course perspective recognizes that fathers have a life history of their own. Their involvement in their children’s lives is determined in part by their own life experiences, including their own father’s involvement in their childhood.76 The capacity to support and nurture needs to be cultivated over their life course. Thus, closing the Black-White gap in adverse birth outcomes requires strengthening father involvement through a multi-level approach addressing individual-level (eg, skills), interpersonal (eg, gender relations), neighborhood and community (eg, unemployment, incarceration), institutional (eg, cultural norms, racial stratification), public policy (eg, tax, welfare, and child support), and other life course factors. Enhance Systems Coordination and Integration for Family Support Services Presently there is a great deal of fragmentation in the delivery system for family support services. Enhancing ser- vice coordination and systems integration may help reduce stress and increase support for pregnant and parenting women and their families. Women needing multiple services often have to take time off from work on different days, arrange child care, find transportation to different appointment locations, fill out duplicative records, and still may not receive needed services because of missing referral paperwork or provider miscommunication. Fragmentation in service delivery deters access to care, particularly for low-income women with other competing needs. These women need help with service coordination. Programs like the Nurse Family Partnership86 or Black Infant Health program87 in California have demonstrated some success in providing service coordination for low-income pregnant and parenting women through case management and home visitation. Another possible strategy for service coordination and integration is a family resource center with one-stop shopping, which delivers a comprehensive, integrated portfolio of pregnancy and family support services at a single location or under one organizational umbrella.88 The Hope Street Family Center in Los Angeles and the Developing Families Center in District of Columbia offer promising models. Hope Street provides a full array of services, including prenatal care, wellbaby care, primary care, on-site child care, Early Head Start, child development and family literacy programs. Where it is not possible for all services to occur under one roof, different providers can work to coordinate services, conduct follow-up upon referrals, reduce duplication, and create a virtual family resource center. To develop a comprehensive, family resource center, a community must be able to knit together different categorical programs into an integrated funding mechanism. An on-going policy experiment, the Monroe County (New York) Child and Family Health InitiaEthnicity & Disease, Volume 20, Winter 2010 tive, works to create an integrated service delivery system driven by family needs rather than categorical funding requirements.88 This initiative blends funds from six different funding streams into one master contract with one set of reporting mechanisms and a greater focus on results. Integration of funding streams may help promote service integration and multidisciplinary, multi-level, and multisector collaboration. Evaluation of the Monroe County Initiative is currently ongoing. Create Reproductive Social Capital in African American Communities In recent years, social capital has emerged as a possible protective factor against the detrimental effects of stress on health. Social capital describes the degree of social connectedness within a community or society and refers to features of social organization (eg, networks, norms, social trust) that facilitate coordination and cooperation for mutual benefit.89,90 Social capital is characterized by: 1) the existence of community networks; 2) civic engagement; 3) local identity and a sense of solidarity and equity with other community members; and 4) trust and reciprocal help and support. Several studies link social capital to health disparities, including disparities in infant mortality.90 A related concept is reproductive social capital – defined as features of social organization that facilitate coordination and cooperation to promote reproductive health within a community.91 With respect to pregnancy, it describes the degree of social connectedness of the pregnant woman to her community. Presently little is known about how to build reproductive social capital in a community;92 this issue of Ethnicity & Disease provides an instructive example from a community-based program in Los Angeles.91 One Hundred Intentional Acts of Kindness toward a Pregnant Woman was created S2-67 CLOSING GAP IN BIRTH OUTCOMES - Lu et al by Healthy African American Families to increase reproductive social capital for pregnant women. In local focus groups, pregnant or postpartum women were asked to identify specific actions that families, friends, and strangers could take to help make their pregnancies better. From families and friends, women primarily wanted acts demonstrating emotional and instrumental support; from strangers they wanted acts of respect for personal space and common courtesy. Based on their responses, One Hundred Intentional Acts of Kindness toward a Pregnant Woman was created, printed on fans, and distributed in churches, barber shops, nail salons, and other locations. While the effectiveness of the One Hundred Acts program is currently being evaluated, it provides an example of how a community can create reproductive social capital to increase daily social support for pregnant women. The program took on a life course approach as One Hundred Intentional Acts of Kindness toward a New Mother and One Hundred Intentional Acts of Kindness to Yourself (for self-support) were also developed. While these activities do not address structural inequities, they exemplify things a community (under the leadership of communityor faith-based organizations) can readily do to support pregnant and parenting women and families. Invest in Community Building and Urban Renewal As much as it takes a village to raise a child, it takes a community to grow a healthy baby. A growing body of evidence suggests that neighborhood or community characteristics may be important determinants of birth outcomes. Increased risk of VLBW births occurred among African American women rating their neighborhoods unfavorably in eight characteristics: police protection, property protection, personal safety, friendliness, municipal service delivery, cleanliness, quietness, and schools.93 S2-68 Urban African-American women were more likely to deliver LBW infants when they lived in socioeconomically disadvantaged area, regardless of individual level poverty and other risk factors.94 Several potential pathways linking neighborhood and community characteristics to adverse birth outcomes have been suggested. First, because of the history of residential segregation, African Americans are more likely to live in concentrated poverty neighborhoods where daily life is more stressful.95 Second, these neighborhoods are more likely to be located near freeways, industrial parks, and toxic waste dumps, exposing residents to greater amounts of pollutants, which increase the risks of adverse birth outcomes.96–100 Third, these neighborhoods are more likely to include a higher proportion of individuals with maladaptive coping behaviors, including violence, drug and alcohol abuse, and smoking. Women living in concentrated poverty neighborhoods are, therefore, more likely to be exposed to these negative influences. Fourth, there is less access to places to exercise safely or to purchase fresh fruits and vegetables. In many disadvantaged communities, there are more liquor stores than grocery stores, and more fast food restaurants than healthy restaurants. The typical cost of food is approximately 15%–20% higher in poor neighborhoods than in affluent neighborhoods, while the quality of food available is poorer.101 Fifth, these neighborhoods are typically underserved by healthcare and social service providers.102 As long as large numbers of African American women grow up and reside in neighborhoods and communities that put them at early-life disadvantages and under greater cumulative allostatic load, racial disparities in birth outcomes will likely persist, even with the best health care. Closing the Black-White gap in birth outcomes requires building stronger and healthier communities that Ethnicity & Disease, Volume 20, Winter 2010 promote not only healthy pregnancy, but the life course health development of women and families. Because over half (52%) of all African Americans live in a central city within a metropolitan area, and nearly 90% live in a metropolitan area, a good starting place is America’s cities.103 Community building must begin with economic development; it is difficult to build and sustain a healthy, vibrant community when over half of its African American male residents are jobless or underemployed, as in many large cities. Community building also requires infrastructure development, such as affordable and decent housing, good schools, safe neighborhood, accessible parks and recreation, clean air and water, and competent healthcare. The Smart Growth 104 and New Urbanism 105 movements provide innovative models of urban development that could also promote population health. And while MCH advocates are not directly in the business of building housing, schools or parks, they need to partner with those who can. Community building requires political development. This involves building community networks and mobilizing civic participation, two important dimensions of social capital. A promising model is the Healthy Births Learning Collaboratives (HBLCs) of the Los Angeles County Best Babies Network. An HBLC is a network of providers, consumers, researchers, public health professionals, community leaders, advocates, and other stakeholders whose primary aim is to improve birth outcomes in their local communities. The collaboration is guided by the principles of community-based participatory research.106,107 The goal is to bring MCH and non-MCH partners together on a regular basis for networking and resource sharing. The HBLC provides a forum for community voices to be heard and creates a platform for civic engagement, grassroots advocacy, and social and human capital development by CLOSING GAP IN BIRTH OUTCOMES - Lu et al facilitating MCH leadership development and community building. ADDRESS SOCIAL AND ECONOMIC INEQUITIES Closing the Black-White gap in birth outcomes also requires changing social institutions and public policies with the goals of reducing early life disadvantages and cumulative allostatic load over the life course.108 We believe closing the education gap, reducing poverty, supporting working mothers and families, and undoing racism are important in eliminating racial disparities in birth outcomes. This is a new paradigm for MCH partners. Maternal and child health advocates are not exempt from addressing disparities outside traditional boundaries; it is imperative that we understand how cumulative social and economic inequities contribute to health disparities in MCH. Close the Education Gap More than 50 years after Brown v Board of Education, the Black-White gap in education persists. Despite school desegregation, today many of our schools, particularly in inner cities, remain separate and unequal. The Black-White education gap actually starts before children enter school. On average, African American children enter kindergarten with substantial deficits in reading and math skills, perhaps reflecting early life disadvantages.109 The education gap widens between first and twelfth grades.110 African American children, particularly from low-income families, are more likely to attend schools with fewer resources, poorer quality teachers and lower expectations. The gap grows after school and during summer months, as African American children have fewer opportunities for learning enrichment outside of school.111 African American children are also more likely to experience health problems (eg, vision, hearing, oral health, asthma) but less likely to receive adequate health services for those problems.108 Because of housing and job instabilities in the family, African American children are more than twice as likely as White children to have attended at least three different schools by third grade.112 Both health problems and residential mobility could create stress and interfere with learning. As a result of all these factors, African American students are significantly less likely to graduate from high school and to complete college.103 Lower educational attainment predicts lower earnings (and less health insurance coverage and access to health care, fewer resources, greater job strains and insecurity, and poorer housing and neighborhoods). Lower educational attainment also predicts poorer reproductive health and poorer pregnancy outcomes,3 possibly mediated through greater cumulative allostatic load over the life course. The solutions to closing the BlackWhite gap in birth outcomes require closing the education gap and are neither easy nor cheap.108 Children cannot learn well without a healthy brain and so early childhood development must begin before birth, or even conception. None of us are born ready to parent and so parenting education must also begin before the child’s birth. Presently, most Head Start programs do not begin until age 3 or 4. To narrow the education gap in early life, children from low-income households should be offered optional full-day, year-round early childhood programs starting as early as six months of age and full-day, year-round pre-school at ages 3 and 4. These programs should be staffed with professional teachers and nurses, and provided curricula emphasizing literacy and appropriate social and emotional growth. Optimally they should attend K through 12 schools with small class size, good teachers, high expectations, standards, accountability, after-school and summer programs, and full-service Ethnicity & Disease, Volume 20, Winter 2010 school-community clinics. The costs of adding these programs to all US schools with at least 40% low-income children is estimated at $156 billion a year, or $12,500 per pupil.109 That is the level of commitment our nation must make to close the Black-White gap in education. Reduce Poverty among African American Families A disproportionate number of African Americans live below the poverty level, accounting for about one-quarter of the US population in poverty in 2001.103 One in four (25%) Black women are poor, a rate nearly three times that for non-Hispanic White women (9%). Nearly one in three (30%) African American children live in a poor household, a rate three times that for non-Hispanic White children (10%). The poverty rate is highest among single-parent households headed by African American women; one in three (35%) such households are poor, and more than half (58%) report an annual income of less than $25,000.103 Poverty predicts poorer health,108 perhaps reflecting greater cumulative allostatic load over the life course and resulting in increased biobehavioral vulnerability during pregnancy. Public policy can help reduce poverty among African American families. First, raising the minimum wage, expanding EITC, strengthening collective bargaining, and adopting pay equity policies will substantially increase incomes for working families. Raising the minimum wage by one dollar will impact nearly 30% of working African American women who work for minimum or low wages.113 Expanding EITC may be more effective in moving families over the poverty line than any other government programs.114 An innovative proposal, the ‘‘Universal Unified Child Credit,’’ combines both expanded EITC with child tax credits.115 Unions raise wages and benefits of unionized workers by about 28%.116 S2-69 CLOSING GAP IN BIRTH OUTCOMES - Lu et al Second, investing in a social safety net of programs, such as food stamps, Section 8 vouchers for housing and Medicaid, will help poor African American families meet basic needs. In 2000, low-income single mothers earned, on average, about $8,000, but after the EITC and other public assistance their average income nearly doubled, to about $16,000.117 Third, an economy that delivers on full employment, living wages, fair trade, job training and retraining, and health insurance coverage will help reduce poverty among African American families.117 Support Working Mothers and Families Most African American mothers work. Two areas will serve as examples of where public policy can better support working mothers: parental leave and child care. Leave policies give working parents the right to take time off from work without the risk of losing their jobs. Before the 1993 Family and Medical Leave Act (FMLA), the United States had no national maternity (or paternity) leave legislation,118 in contrast to most developed nations (most with paid leave). While FMLA dramatically increased both maternity and paternity leave coverage, it is not universal. Part-time employees, employees in small businesses, and employees with short job tenure are often not covered or eligible. As a result, only 45% of parents working in the private sector have guaranteed unpaid parental leave through FMLA. African Americans have higher coverage under FMLA because they are proportionately more likely to work in the public sector and for large establishments; nonetheless, nearly 30% of working African Americans parents do not have guaranteed leave. Women with leave coverage are more likely to take leave and to take longer leaves.118 FMLA is also limited in that it provides only 12 weeks of unpaid parental leave. Less than 5% of parents working in the private sector S2-70 have access to paid parental leave.118 This lack of paid leave is a barrier to women’s taking leave or taking as much leave as needed; many women face substantial loss of income by taking an unpaid leave.119 As a result, nearly a third of women on maternity leave returned to work in less than 6 weeks; over 70% returned to work in less than 12 weeks.119 Clearly public policy can do more to support working parents so they can care for their newborn or sick child without the risk of losing their jobs or pay.118 Some have begun to call for expanding parental leave coverage, extending the duration of leave allowed, providing more opportunities for parents of young children to return to work part time, and making provisions for income replacement during leave.118 With respect to the latter, public financing options include using: 1) unemployment insurance, 2) temporary disability insurance programs, 3) a new social insurance program, and 4) a new cash benefit program.118 In July 2004, California became the first state to provide paid leave for up to six weeks for parents with a newborn or for employees with an ill family member. Small businesses (less than 50 employees) are exempt. The program is funded from employee payroll tax. In contrast, most European countries provide for longer paid parental leaves largely financed through social insurance programs.118 One of the most dramatic transformations in the American family over the past 30 years has been the increased labor force participation rates of mothers with young children.118 The majority (57%) of mothers with children aged 0 to 3 years work. This trend is particularly striking for low-income families with single parents. Prior to the 1996 Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA), Aid to Families with Dependent Children (AFDC) provided cash assistance to low-income single Ethnicity & Disease, Volume 20, Winter 2010 mothers to allow them to remain at home and care for their children. The Temporary Assistance for Needy Families now requires mothers to work or seek employment or training as a condition of receiving cash assistance. When single mothers or both parents are working, child care is needed. In 2001, 48% of African American children aged 0 to 2 years, 74% aged 3 to 6, and 66% in grade school are in nonparental care; the majority in centerbased programs.120,121 Two major concerns of working mothers are child care costs and quality. While working families that pay for child care spend, on average, about 9% of their earnings on child care, that burden is higher for low-income families (16% of earnings), and for singleparent low-income families (19% of earnings).122 While low-income families are more likely to receive help (eg, relatives, government subsidies) for child care, 40% of low-income families that pay for child care spend, on average, $1 of every $6 in earnings for that care.122,123 And much of the quality of child care available for young children is mediocre or worse. Children in lower-income families often receive lower quality care than children in higher-income families.118 Long-term follow-up studies of low-income children randomly assigned to a treatment group receiving high-quality child care versus a control group without any special services revealed lower rates of crime, welfare dependency, and teen pregnancy, and higher educational attainment, employment, and earnings among those receiving high-quality child care.118,124 Public policy can assist working parents, particularly single mothers and low-income families, so they can afford high-quality child care.118 Presently, child care for low-income families is supported primarily through subsidies to parents or private market providers. While this approach increases parental choice, it creates challenges in ensuring CLOSING GAP IN BIRTH OUTCOMES - Lu et al access and quality. One option is to provide vouchers with a reimbursement rate that increases with the developmental quality of child care purchased. This would give parents an incentive to seek higher quality child care and providers an incentive to improve quality. Public early education programs like Head Start and Early Head Start also need expansion. Head Start is mostly a part-day, part-year program for poor families, serving about 50% of eligible children aged 3 or 4 years-old. Early Head Start serves only a small share of eligible children under 3 years old. These high-quality programs need to be expanded to serve more children from birth to 5 years old and for more hours to meet the full-day, year-round needs of working families. Another option is to expand prekindergarten and other early education programs delivered in community-based child care programs, and to link prekindergarten funding to higher standards, teacher qualifications, and curriculum requirements. An Institute of Medicine report estimates that expanding child care subsidies through quality-related vouchers for eligible children would cost $54 billion, expanding and increasing access to full-day, full-year Head Start and Early Head Start would cost $25 billion, and expanding prekindergarten and other early education programs would cost $25 to $35 billion.118 Despite their high costs, we believe these programs will pay great dividends in the long run and pay for themselves many times over. Undo Racism Increasing evidence suggests racism may be the ‘‘cause of the cause’’ of health disparities in the United States. The experience of racial discrimination in pregnancy or over the life course by African American women is associated w i t h i n c r e a s e d r is k o f V L B W births.125,126 A greater Black-White gap in infant mortality was found in more racially segregated cities.127,128 Camara Jones proposed a theoretical framework for understanding racism on 3 levels – internalized, personallymediated, and institutionalized racism – and introduced an allegory about a gardener with 2 flower boxes, with either rich or poor soil, to illustrate the differences in and remediation of these.129 Institutionalized racism, or differential access to the goods, services, and opportunities of society by race, is the soil – and this is the most fundamental level to address for change. Our 12-point plan is essentially about enriching the soil with better healthcare, education, child care and other social supports to grow healthier mothers and babies. What are the specific roles of MCH professionals in undoing racism? Maternal and child health is a field consisting of people from diverse backgrounds and disciplines, including researchers, service providers, public health professionals, and community advocates. Each has a role in undoing racism. Researchers need to develop better measures of racism, identify causal pathways linking racism to health disparities, design longitudinal studies of both current racism and racism over the life course and across generations, and develop intervention studies to address multiple levels of racism including institutionalized racism. Healthcare providers and other service providers need to critically examine their personal attitudes and behaviors, and institutional practices and policies, to assure all patients or clients, regardless of race and ethnicity, receive equitable care.130 Public health professionals need to make racism a leading public health issue, including collecting data on racism in population and community health assessments, assuring equal access to quality healthcare, monitoring for discriminatory practices, and making policies (or collaborating with other public agencies to make policies) to assure equal access to goods, services, and opportunities vital to maternal and Ethnicity & Disease, Volume 20, Winter 2010 child health. In all these efforts, community voices must be heard. They have been telling us that racism is a main cause of disparities in birth outcomes; now the community must be included as partners in collaborative efforts to undo racism. Many of our social institutions and public policies create early life disadvantages and disproportionate allostatic load on the health of African American women over their lifespan. We cannot eliminate racial disparities in birth outcomes without addressing racial disparities in education, healthcare, housing, employment, the criminal justice system and the built environment. While MCH advocates are not expected to solve all these problems, we can do a number of things to address social and economic inequities. First, we need to educate ourselves about disparities in other domains of life and their impact on maternal and child health. We need to see how disparities in their fields impact ours and to champion their causes as much as we need them to champion ours. Second, we need to partner with people from other walks of life who also address racial disparities. They need to see how disparities in MCH affect the disparities they address. In too many of our meetings, we are preaching only to the choir. We can begin by inviting unusual partners from other sectors, such as education, community development, city planning, and the criminal justice system to our meetings. Third, we need to join forces with these non-MCH partners in advocacy. All these require transformative leadership that brings people together to see a common vision and work for a common cause. The common vision is the life course perspective; the common cause – social justice. CONCLUSIONS We outlined a 12-point plan to close the Black-White gap in birth outcomes S2-71 CLOSING GAP IN BIRTH OUTCOMES - Lu et al using a life course approach. Collectively these points represent a new approach to an old problem. They go beyond prenatal care to address the healthcare needs of African American women over the life course. They go beyond individual-level interventions that are often short-lived (eg, during pregnancy or a funding grant) to address strengthening family and community systems that may have a broader, more lasting impact on the health of pregnant women, families, and communities. And they go beyond the biomedical model to address the social and economic inequities that create disproportionate allostatic load on African American women’s health. Two more things are needed for real change – a greater knowledge base and a stronger political will.131 We need to build on our knowledge base with not only more research, but better research. Current MCH research is limited by 3 major disconnects: disconnect between the perinatal period and the rest of the life course (longitudinal disconnect), disconnect between the individual and her environments (contextual disconnect), and disconnect across disciplines and between academic and community researchers (intellectual disconnect). Longitudinal integration is needed to better understand life course influences on perinatal outcomes and perinatal influences on life course outcomes. This requires more longitudinal birth cohort studies and databases linkages across the lifespan. Contextual integration is needed to better understand influences of neighborhood and community characteristics on individual health and behaviors, and to delineate how these contextual factors become embedded in pregnancy physiology and developmental biology (ie, how social inequality gets under the skin). This requires the development of better measures (eg, for institutionalized racism) and methodologies for contextual analyses. Intellectual integration is needed to break out of disciplinary and institutional silos S2-72 and bridge the academic-community divide that has limited our research. This requires building infrastructure (eg, training programs, research networks) to support transdisciplinary research and community-academic partnerships. Most importantly, we need more praxis – the integration of knowledge and practice. Research cannot help if it is not translated into effective interventions. This requires a new approach to designing intervention studies and evaluating their impact from multi-level, life-course perspectives. It requires collaboration among researchers from diverse fields (eg, health, education, housing, criminal justice) and among funders to support largescale social experimentation using a comprehensive, life-course approach. We will not close the Black-White gap in birth outcomes without political will to do so. Political will is the ability to command resources to make things happen (ie, implement the 12 points). There are several things we can do to create political will. First, we need evaluation research to demonstrate the effectiveness and cost-benefit of these broadened concepts of health care. The impetus for expanding public coverage of prenatal care in the late 1980’s came largely from studies demonstrating costsavings in postnatal infant care with the provision of prenatal care. Now we need to make an equally compelling case for the cost-benefit of interconception and preconception care, with benefits measured in terms of immediate birth outcomes and long-term health and developmental outcomes, and cost savings accrued in the healthcare, education, criminal justice, welfare, and other systems. Second, we need to increase demand for comprehensive women’s health care before and between pregnancies and over the life course. We must make the case to the American public that preconception care, interconception care, and access to quality health care over the lifespan are as important, if not Ethnicity & Disease, Volume 20, Winter 2010 more than, as prenatal care is to the health and wellbeing of mothers and infants. We need to create this demand not just among White middle-class women (critical for creating political will), but especially among African American women. Third, we need leadership. Currently there is growing political will to support father involvement (eg, federal Fatherhood Initiative) and systems integration (eg, federal Community Integrated Service System projects). Ideas such as the One Hundred Acts are met with great receptivity in communities because they demonstrate what communities can do for themselves to increase social support and social capital for pregnant women and families. Partisan politics aside, we can all agree that father involvement, family-centered care, and strong social capital are good for the African American community, or any community. What we need is leadership to make it happen. Community- and faith-based organizations can take the lead in creating reproductive social capital. County and state governments can encourage service integration by blending categorical funding streams. Maternal and child health professionals can play a leadership role in consensus building – bringing people together to see a common vision and to work on a common cause. Fourth, we need creativity in building linkages and partnerships. We need linkages to on-going efforts to address disparities in other domains of life, such as broadening the vision of No Child Left Behind to include a health component. We need to develop partners from education, community development, city planning, and the criminal justice system. We need to make the case to businesses and industries to support more mother-friendly workplaces and leave policies – in terms of reduced medical costs, lower absenteeism, and a more stable and productive workforce. Lastly, we need to renew the public discourse on health disparities in the CLOSING GAP IN BIRTH OUTCOMES - Lu et al terms of social justice. This is primarily a moral issue; in what kind of America do we want our children to grow up? An America where a Black baby has twice the chance of dying within the first year of life as a White baby, three times the chance of being born to a single mother, three times the chance of growing up in a poor household, twice the chance of going without health insurance, half the chance of completing college, and a life expectancy 5.5 years shorter? Or an America where all men and women are created equal and are afforded equal rights and equal opportunities, and where we treat our fellow Americans as we want to be treated, or we wish our children to be treated? Institutionalized racism is often evident as inaction in the face of need. Continuing to do the same old things that do not work in the face of persisting disparities in birth outcomes perpetuates institutionalized racism. For too long we have looked for a quick fix to close the gap. Elimination of racial disparities in birth outcomes is attainable if we make the life course, perhaps intergenerational, social investments it will take. The 12 points are a beginning. The health of our nation tomorrow depends on the choices we make today. ACKNOWLEDGMENTS Support for this work was provided in part by the National Institute of Health Women’s Reproductive Health Career Development Fellowship #HD01281-03, the National Institute of Child Health and Development Community Child Health Network #U01-HD044245, the Centers for Disease Prevention and Health Promotion Division of Reproductive Health, and the Los Angeles Best Babies Collaborative, a program of First 5 LA. The opinions expressed in this paper are the authors’ and do not necessarily reflect the views or policies of the institutions with which the authors are affiliated. REFERENCES 1. Mathews TJ, MacDorman MF. Infant mortality statistics from the 2004 period linked birth/infant death data set. Natl Vital Stat Rep. 2007;55(14):1–32. 2. Arias E, Anderson RN, Kung HC, et al. Deaths: final data for 2001. Natl Vital Stat Rep. 2003;52(3):1–115. 3. Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2005. Natl Vital Stat Rep. 2007;56(6):1–103. 4. Kramer MS, Seguin L, Lydon J, et al. Socioeconomic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000;14(3):194–210. 5. Institute of Medicine. Preventing low birth weight. Washington DC: National Academy Press; 1985. 6. Paarlberg KM, Vingerhoets AJ, Passchier J, et al. Psychosocial factors and pregnancy outcome: a review with emphasis on methodological issues. J Psychosom Res. 1995;39(5): 563–595. 7. Fiscella K. Race, perinatal outcome, and amniotic infection. Obstet Gynecol Surv. 1996 January;51(1):60–66. 8. Goldenberg RL, Cliver SP, Mulvihill FX, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175(5):1317–1324. 9. Shiono PH, Rauh VA, Park M, et al. Ethnic differences in birthweight: the role of lifestyle and other factors. Am J Public Health. 1997; 87(5):787–793. 10. Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003; 7(1):13–30. 11. Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. 2002;80(3):433–479, iii. 12. Kuh D, Ben-Shlomo Y. A Life Course Approach to Chronic Disease Epidemiology. Oxford: Oxford University Press; 2004. 13. Seckl JR. Physiologic programming of the fetus. Clin Perinatol. 1998;25(4):939–962, vii. 14. Hertzman C. The biological embedding of early experience and its effects on health in adulthood. Ann NY Acad Sci. 1999;896:85–95. 15. Suomi SJ. Early determinants of behaviour: evidence from primate studies. Br Med Bull. 1997;53(1):170–184. 16. Meaney MJ, Aitken S, Sharma S, et al. Postnatal handling increases hippocampal type II glucocorticoid receptors and enhances adrenocortical negative-feedback efficacy in the rat. J Neuroendocrinol. 1989;5: 597–604. 17. Gunnar MR, Nelson CA. Event-related potentials in year-old infants: relations with emotionality and cortisol. Child Dev. 1994;65(1):80–94. 18. Heim C, Newport DJ, Heit S, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical Ethnicity & Disease, Volume 20, Winter 2010 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. abuse in childhood. JAMA. 2000;284(5): 592–597. Coe CL. Psychosocial factors and psychoneuroimmunology within a lifespace perspective. Developmental Health and the Wealth of Nations: Social, Biological and Educational Dynamics. New York: Guilford Press, 1999;201–219. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998; 338(3):171–179. Sapolsky RM. Social subordinance as a marker of hypercortisolism. Some unexpected subtleties. Ann NY Acad Sci. 1995; 771:626–639. Kristenson M, Kucinskiene Z, Bergdahl B, et al. Increased psychosocial strain in Lithuanian versus Swedish men: the LiVicordia study. Psychosom Med. 1998;60(3):277–282. Chrousos GP. The stress response and immune function: clinical implications. The 1999 Novera H. Spector Lecture. Ann NY Acad Sci. 2000;917:38–67. Geronimus AT. Black/White differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42(4): 589–597. Hogan VK, Richardson JL, Ferre CD, et al. A public health framework for addressing Black and White disparities in preterm delivery. J Am Med Womens Assoc. 2001;56(4):177–180, 205. Lu MC, Kotelchuck M, Culhane JF, et al. Preconception care between pregnancies: the content of internatal care. Matern Child Health J. 2006 September;10(5 Suppl):S107–S122. Bloom SL, Yost NP, McIntire DD, et al. Recurrence of preterm birth in singleton and twin pregnancies. Obstet Gynecol. 2001;98(3): 379–385. Adams MM, Elam-Evans LD, Wilson HG, et al. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596. The Interconception Health Promotion Initiative Team. Interconception Health Promotion Initiative Final Report. Denver: Colorado Trust. 2003. Available at: http://www. coloradotrust.org/attachments/0000/3168/ IHPIFinalReport04.pdf. Last accessed January 25, 2010. Biermann J, Dunlop AL, Brady C, et al. Promising practices in preconception care for women at risk for poor health and pregnancy outcomes. Matern Child Health J. 2006;10(5 Suppl):S21–S28. Committee on Unintended Pregnancy, Institute of Medicine. The Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. Washington DC: National Academy of Sciences; 1995. S2-73 CLOSING GAP IN BIRTH OUTCOMES - Lu et al 32. Rawlings JS, Rawlings VB, Read JA. Prevalence of low birth weight and preterm delivery in relation to the interval between pregnancies among White and Black women. N Engl J Med. 1995;332(2):69–74. 33. Wadhwa PD, Culhane JF, Rauh V, et al. Stress and preterm birth: neuroendocrine, immune/inflammatory, and vascular mechanisms. Matern Child Health J. 2001;5(2): 119–125. 34. Kondwani KA, Lollis CM. Is there a role for stress management in reducing hypertension in African Americans? Ethn Dis. 2001;11(4): 788–792. 35. Klima CS. Centering pregnancy: a model for pregnant adolescents. J Midwifery Womens Health. 2003;48(3):220–225. 36. Smaill F. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev, 2001;(2):490. 37. Jeffcoat MK, Hauth JC, Geurs NC, et al. Periodontal disease and preterm birth: results of a pilot intervention study. J Periodontol. 2003;74(8):1214–1218. 38. Reid G, Bocking A. The potential for probiotics to prevent bacterial vaginosis and preterm labor. Am J Obstet Gynecol. 2003; 189(4):1202–1208. 39. Olsen SF, Secher NJ, Tabor A, et al. Randomised clinical trials of fish oil supplementation in high risk pregnancies. Fish Oil Trials In Pregnancy (FOTIP) Team. BJOG. 2000;107(3):382–395. 40. Kupferminc MJ, Eldor A, Steinman N, et al. Increased frequency of genetic thrombophilia in women with complications of pregnancy. N Engl J Med. 1999;340(1):9–13. 41. Fiscella K, Franks P, Kendrick JS, et al. Risk of preterm birth that is associated with vaginal douching. Am J Obstet Gynecol. 2002; 186(6):1345–1350. 42. Desvarieux M, Demmer RT, Rundek T, et al. Relationship between periodontal disease, tooth loss, and carotid artery plaque: the Oral Infections and Vascular Disease Epidemiology Study (INVEST). Stroke. 2003;34(9):2120–2125. 43. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342(20):1500–1507. 44. Carey JC, Klebanoff MA, Hauth JC, et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. N Engl J Med. 2000;342(8):534–540. 45. King J, Flenady V. Antibiotics for preterm labour with intact membranes. Cochrane Database Syst Rev, 2000;(2):246. 46. Korenbrot CC, Steinberg A, Bender C, et al. Preconception care: a systematic review. Matern Child Health J. 2002;6(2):75–88. 47. Kotelchuck M. Building on a life-course perspective in maternal and child health. Matern Child Health J. 2003;7(1):5–11. S2-74 48. Moos MK. Preconceptional health promotion: progress in changing a prevention paradigm. J Perinat Neonatal Nurs. 2004; 18(1):2–13. 49. American College of Obstetricians and Gynecologists. ACOG technical bulletin. Preconceptional care. Int J Gynaecol Obstet. 1995;50(2):201–207. 50. Brown ER, Ojeda VD, Wyn R, et al. Racial and ethnic disparities in access to health insurance and health care. Los Angeles: UCLA Center for Health Policy Research, 2000; Available at: http://www.healthpolicy.ucla. edu/pubs/files/racialandethnicdisparitiesreport. pdf. Last accessed January 26, 2010. 51. Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care–United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55(RR-6):1–23. 52. Alan Guttmacher Institute. Preconceptional and prenatal care can improve birth outcomes. New York: Alan Guttmacher Institute; 1993. 53. Persaud ODD. Maternal diabetes and the consequences for her offspring. J Devel Disabilities. 2007;13(1):101–133. 54. Kogan MD, Alexander GR, Kotelchuck M, et al. Relation of the content of prenatal care to the risk of low birth weight. Maternal reports of health behavior advice and initial prenatal care procedures. JAMA. 1994; 271(17):1340–1345. 55. Kogan MD, Kotelchuck M, Alexander GR, et al. Racial disparities in reported prenatal care advice from health care providers. Am J Public Health. 1994;84(1):82–88. 56. Brett KM, Schoendorf KC, Kiely JL. Differences between Black and White women in the use of prenatal care technologies. Am J Obstet Gynecol. 1994;170(1 Pt 1):41–46. 57. Kilo CM. Improving care through collaboration. Pediatrics. 1999;103(1 Suppl E):384–393. 58. Fiore MC, Bailey WC, Cohen SJ, et al. Treating tobacco use and dependence. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services Public Health Service; 2000. 59. Chasnoff IJ, Neuman K, Thornton C, et al. Screening for substance use in pregnancy: a practical approach for the primary care physician. Am J Obstet Gynecol. 2001;184(4): 752–758. 60. Institute of Medicine, Committee on Nutritional Status During Pregnancy and Lactation, Food and Nutrition Board. Nutrition during Pregnancy and Lactation: An Implementation Guide. Washington DC: National Academy Press, 1992; Available at: http:// www.nap.edu/catalog.php?record_id51984. Last accessed January 26, 2010. Ethnicity & Disease, Volume 20, Winter 2010 61. American College of Obstetricians and Gynecologists. Domestic violence. Washington DC: American College of Obstetricians and Gynecologists, 1999;Report No. 257. 62. American College of Obstetricians and Gynecologists. Depression in women. ACOG technical bulletin number 182. Int J Gynaecol Obstet. 1993;43(2):203–211. 63. Ugwumadu A, Manyonda I, Reid F, et al. Effect of early oral clindamycin on late miscarriage and preterm delivery in asymptomatic women with abnormal vaginal flora and bacterial vaginosis: a randomised controlled trial. Lancet. 2003;361(9362):983– 988. 64. Meis PJ, Klebanoff M, Thom E, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. 65. American College of Obstetricians and Gynecologists. ACOG Committee Opinion. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2003 November;102(5 Pt 1):1115–1116. 66. Daniel DM, Norman J, Davis C, et al. A state-level application of the chronic illness breakthrough series: results from two collaboratives on diabetes in Washington State. Jt Comm J Qual Saf. 2004;30(2):69–79. 67. Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Saf. 2001;27(2):63–80. 68. Cherouny PH, Ustianov JR, Shaw J, et al. Improving prenatal care in Vermont: A community-based learning collaborative. American Public Health Association Annual Conference; Washington DC 2004. 69. Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991 May;77(5):782–787. 70. Woolhandler S, Himmelstein DU, Angell M, et al. Proposal of the Physicians’ Working Group for Single-Payer National Health Insurance. JAMA. 2003;290(6):798–805. 71. Grumbach K, Odom K, Moreno G, et al. Physician Diversity in California: New Findings from the California Medical Board Survey. San Francisco CA: Center for California Health Workforce Studies; 2008. 72. González-Rivera C, Middleton K. Representing the new majority. Part III: A Status Report on the Diversity of the University of California Medical Student Body. Berkeley CA: The Greenlining Institute, 2008. Available at: http://tinyurl.com/cgkbd7. Last accessed January 26, 2010. 73. Saha S, Arbelaez JJ, Cooper LA. Patientphysician relationships and racial disparities in the quality of health care. Am J Public Health. 2003 October;93(10):1713–1719. CLOSING GAP IN BIRTH OUTCOMES - Lu et al 74. Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Aff (Millwood). 2002;21(5):90–102. 75. Sorensen E, Mincy R, Halpern A. Redirecting welfare policy toward building strong families. Washington DC: The Urban Institute, 2000;Available at: http://www.urban. org/UploadedPDF/310263_sf_3.pdf. Last accessed January 26, 2010. 76. Lu MC, Jones L, Bond M, et al. Where is the F in MCH? Father involvement in African American families. Ethn Dis. 2010;20(1, Suppl 2):S2-49–S2-61. 77. Hewlett SA, West C. The War Against Parents: What We Can Do for America’s Beleaguered Moms and Dads. Boston: Houghton Mifflin; 1998. 78. Turning the corner on father absence in Black America. Morehouse Conference on African American Fathers. Atlanta: Morehouse Research Institute & Institute for American Values; 1999. 79. Wilson WJ. When Work Disappears: The World of the New Urban Poor. New York: Knopf; 1996. 80. McLanahan SS, Sandefur G. Growing Up with a Single Parent: What Hurts, What Helps. Cambridge MA: Harvard University Press; 1994. 81. Bronfenbrenner U. Ecology of Human Development: Experiments by Nature and Design. Cambridge MA: Harvard University Press; 1979. 82. Bloom D, Sherwood K. Matching opportunities to obligations: lessons for child support reform from the Parents’ Fair Share Pilot Phase. 2000. Available at: http://fatherhood. hhs.gov/pfs94. Last accessed January 26, 2010. 83. Moore T, Kotelchuck M. Predictors of urban fathers’ involvement in their child’s health care. Pediatrics. 2004;113(3 Pt 1):574–580. 84. Sorensen E. Obligating dads: Helping lowincome noncustodial fathers do more for their children. Washington DC: The Urban Institute, 2000. Available at: http://www. urban.org/url.cfm?ID5309214. Last accessed January 26, 2010. 85. Wheaton L. Low-income families and the marriage tax. Washington DC: Urban Institute, 1998. Available at: http://www. urban.org/UploadedPDF/marriage_tax.pdf. Last accessed January 26, 2010. 86. Kitzman H, Olds DL, Sidora K, et al. Enduring effects of nurse home visitation on maternal life course: a 3-year follow-up of a randomized trial. JAMA. 2000;283(15): 1983–1989. 87. Willis WO, Eder CH, Lindsay SP, et al. Lower rates of low birthweight and preterm births in the California Black Infant Health Program. J Natl Med Assoc. 2004;96(3):315– 324. 88. Waddell B, Shannon M, Durr R. Using family resource centers to support California’s young children and their families. In: Halfon N, Shulman E, Hochstein M, eds. Building Community Systems for Young Children. Los Angeles: UCLA Center for Healthier Children, Families and Communities; 2001. 89. Putnam RD, Leonardi R, Nanetti RY. Making Democracy Work: Civic Traditions in Modern Italy. Princeton NJ: Princeton University Press; 1993. 90. Kawachi I, Kennedy BP, Lochner K, et al. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491– 1498. 91. Jones L, Lu MC, Lucas-Wright A, et al. One hundred intentional acts of kindness toward a pregnant woman: Building reproductive social capital in Los Angeles. Ethn Dis. 2010;20(1, Suppl 2):S2-36–S2-40. 92. Putnam RD, Feldstein LM. Better Together: Restoring the American Community. New York NY: Simon & Schuster; 2003. 93. Collins JW, Jr., David RJ, Symons R, et al. African-American mothers’ perception of their residential environment, stressful life events, and very low birthweight. Epidemiology. 1998;9(3):286–289. 94. O’Campo P, Xue X, Wang MC, et al. Neighborhood risk factors for low birthweight in Baltimore: a multilevel analysis. Am J Public Health. 1997;87(7):1113–1118. 95. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. 96. Woodruff TJ, Parker JD, Kyle AD, et al. Disparities in exposure to air pollution during pregnancy. Environ Health Perspect. 2003;111(7):942–946. 97. Ritz B, Yu F. The effect of ambient carbon monoxide on low birth weight among children born in southern California between 1989 and 1993. Environ Health Perspect. 1999;107(1):17–25. 98. Ritz B, Yu F, Chapa G, et al. Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology. 2000;11(5):502– 511. 99. Bove F, Shim Y, Zeitz P. Drinking water contaminants and adverse pregnancy outcomes: a review. Environ Health Perspect. 2002;110 Suppl 1:61–74. 100. Sharara FI, Seifer DB, Flaws JA. Environmental toxicants and female reproduction. Fertil Steril. 1998;70(4):613–622. 101. Emmons KM. Health behaviors in a social context. In: Berkman L, Kawachi I, eds. Social Epidemiology. Oxford: Oxford University Press, 2000;242–266. Ethnicity & Disease, Volume 20, Winter 2010 102. Mullings L, Wali A, McLean D, et al. Qualitative methodologies and community participation in examining reproductive experiences: the Harlem Birth Right Project. Matern Child Health J. 2001;5(2):85–93. 103. McKinnon J. The Black population in the United States: March 2002. Washington DC: US Census Bureau, 2003;Report No.: Series P20–541. 104. Geller AL. Smart growth: a prescription for livable cities. Am J Public Health. 2003;93(9): 1410–1415. 105. Steuteville R, Langdon P. New Urbanism: Comprehensive Report and Best Practice Guide. 3 ed. Ithaca NY: New Urban Publications; 2004. 106. Minkler M. Using participatory action research to build healthy communities. Public Health Rep. 2000;115(2–3):191–197. 107. Viswanathan M, Ammerman A, Eng E, et al. Community-Based Participatory Research: Assessing the Evidence. Rockville MD: Agency for Healthcare Research and Quality, 2004 Jul.;Report No.: Evidence Report/ Technology Assessment No. 99. AHRQ Publication 04-E022-2. 108. Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325–334. 109. Rothstein R. Class and Schools: Using Social, Economic, and Educational Reform to Close the Black-White Achievement Gap. Washington DC: Economic Policy Institute; 2004. 110. Phillips M. Understanding ethnic differences in academic achievement: Empirical lessons from national data. In: Grissmer DW, Ross JM, eds. Analytic Issues in the Assessment of Student Achievement. Washington DC: US Department of Education, 2000;103–132. 111. Hauser RM. Response: Two studies of academic achievement. In: Grissmer DW, Ross JM, eds. Analytic Issues in the Assessment of Student Achievement. Washington DC: US Department of Education; 2000. 112. US General Accounting Office. Elementary school children: Many change schools frequently, harming their education. Washington DC: US General Accounting Office, 1994;Report No.: GAO/HEHS-94-45. 113. Bernstein J, Schmitt J. The impact of the minimum wage: Policy lifts wages, maintains floor for low-wage labor market. Washington DC: Economic Policy Institute, 2000; Available at: http://epi.3cdn.net/1b3d426ead29a5c032_ h4m6b54u4.pdf. Last accessed January 26, 2010. 114. Greenstein R, Shapiro I. New research findings on the effects of the Earned Income Tax Credit. Washington DC: Center on Budget and Policy Priorities, 2000;Report No.: #98022. Available at: http://www.cbpp.org/cms/ index.cfm?fa5view&id51649. Last accessed January 26, 2010. S2-75 CLOSING GAP IN BIRTH OUTCOMES - Lu et al 115. Cherry R, Sawicky MB. Giving tax credit where credit is due: A ‘Universal Unified Child Credit’ that expands the EITC and cuts taxes for working families. Washington DC: Economic Policy Institute, 2000;Report No.: #91. 116. Mishel L, Walters M. How unions help all workers. Washington DC: Economic Policy Institute, 2003. Available at: http://www.epi. org/page/-/old/briefingpapers/143/bp143. pdf. Last accessed January 26, 2010. 117. Mishel L, Bernstein J, Boushey H. The State of Working America 2002/2003. Ithaca NY: Cornell University Press; 2000. 118. National Research Council, Institute of Medicine, Committee on Family and Work Policies. Working families and growing kids: Caring for children and adolescents. Washington DC: The National Academies Press; 2003. 119. Cantor D, Waldfogel J, Kerwin J, et al. Balancing the needs of families and employers: Family and medical leave surveys. Rockville MD: Westat; 2001. 120. Capizzano J, Tout K, Adams G. Child care patterns of school-age children with employed mothers. Washington DC: The Urban Institute, 2000. Available at: http:// www.urban.org/UploadedPDF/occa41.pdf. Last accessed January 26, 2010. S2-76 121. Capizzano J, Adams G, Sonenstein FL. Child care arrangements for children under five. Washington DC: The Urban Institute, 2000. Available at: http://www.urban.org/ UploadedPDF/anf_b7.pdf. Last accessed January 26, 2010. 122. Giannarelli L, Barsimantov J. Child care expenses of America’s families. Washington DC: The Urban Institute, 2000;Available at: http://www.urban.org/UploadedPDF/ 310028_occa40.pdf. Last accessed January 26, 2010. 123. Giannarelli L, Adelman S, Schmidt SR. Getting help with child care expenses. Washington DC: The Urban Institute, 2000. Available at: http://www.urban.org/ UploadedPDF/310615_OP62.pdf. Last accessed January 26, 2010. 124. NICHD Early Child Care Research Network. Child-care structureRprocessRoutcome: direct and indirect effects of child-care quality on young children’s development. Psychol Sci. 2002;13(3):199–206. 125. Collins JW, Jr., David RJ, Symons R, et al. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology. 2000;11(3):337–339. Ethnicity & Disease, Volume 20, Winter 2010 126. Collins JW, Jr., David RJ, Handler A, et al. Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination. Am J Public Health. 2004;94(12):2132–2138. 127. Polednak AP. Trends in US urban black infant mortality, by degree of residential segregation. Am J Public Health. 1996;86(5): 723–726. 128. Laveist TA. Segregation, poverty, and empowerment: health consequences for African Americans. Milbank Q. 1993;71(1):41– 64. 129. Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212–1215. 130. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: The National Academies Press; 2003. 131. Richmond JB, Kotelchuck M. Political influences: Rethinking national health policy. In: McGuire CH, Foley RP, Gorr A, Richard RW, eds. Handbook of Health Professions Education. San Francisco: Jossey-Bass, 1983; 384–404.