Venous Thromboembolism Prophylaxis for Medical Inpatients Dennis Whang 4/2/12
advertisement
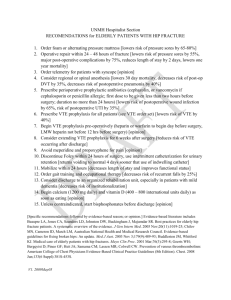
Venous Thromboembolism Prophylaxis for Medical Inpatients Dennis Whang 4/2/12 DSR2 Mini Lecture Objectives • Recognize the morbidity and mortality with venous thromboembolism of inpatients • Determine the risk of VTE for each nonsurgical inpatient admitted • Decide the VTE prophylaxis for each nonsurgical inpatient admitted Background • Most medical inpatients are at risk for venous thromboembolism (VTE): – Deep venous thrombosis (DVT) – Pulmonary embolus (PE) • 25% of all VTE cases occur during hospitalization – 50-75% of VTE cases occur on medical service • 5-10% of inpatient deaths are due to PE • Heparin prophylaxis has NOT shown to decrease risk for inpatient mortality • However it has shown to decrease the incidence of PE Deciding VTE Prophylaxis • Must weigh TWO factors before deciding ppx – VTE Risk – Bleeding risk VTE Prophylaxis Guideline Low Patient admitted Early ambulation Determine risk of VTE Moderate Or High Risk of VTE Low risk if all 3: • Younger than 40 • Mobile • No thrombotic risk factors Moderate risk: All other patients High risk: ICU patients Low Anticoagulant prophylaxis High Intermittent pneumatic compression Determine bleeding risk High Bleeding Risk • Active gastroduodenal bleed • Bleeding within 3 months prior to admission • Platelet count of < 50 Thrombotic Risk Factors for VTE • • • • • • • • • Obesity: BMI > 30 Smoking Immobility Malignancy Previous VTE Placement of central venous catheter Inherited or acquired hypercoagulable states Oral contraceptives/Hormone replacement therapy/tamoxifen Admission diagnosis of: – – – – – – Congestive heart failure (NYHA III/VI) Acute COPD exacerbation Acute infectious disease or sepsis Acute myocardial infarction Stroke with lower limb paralysis Inflammatory bowel disease Mechanical VTE Prophylaxis • Intermittent pneumatic compression – Contraindicated in leg ischemia from peripheral vascular disease • Ineffective in prevention of VTE – Graduated compression stockings – Venous foot pumps Pharmacological VTE Prophylaxis • Low dose unfractionated heparin (UFH) – 5,000 units SQ TID • Low molecular weight heparin (LMWH) – Enoxaparin (Lovenox) 40 mg SQ daily – Do NOT use if CrCl < 30 ml/min What VTE prophylaxis would you use? • A 62 yo F is admitted for community acquired pneumonia. No prior history of VTE, bleeding, hepatic, or renal failure. Her platelet count is 200. • Moderate risk of VTE • Low risk of bleeding • VTE ppx: unfractionated heparin or enoxaparin What VTE prophylaxis would you use? • A 35 yo M is admitted for acute gout. He is ambulatory. He has no prior VTE, GI bleed, thrombophilia, or malignancy. BMI 23. His platelet count is 240. • Low risk of VTE • Low risk of bleeding • VTE ppx: early ambulation What VTE prophylaxis would you use? • 21 yo F admitted to ICU for DKA from poor insulin compliance. She is ambulatory. She has no prior VTE, GI bleed, thrombophilia, or malignancy. Platelet count is 300. • High risk of VTE • Low bleeding risk • VTE ppx: unfractionated heparin or enoxaparin What VTE prophylaxis would you use? • A 65 yo F is admitted for treatment of an active malignancy. CrCl is 20 ml/min. She has a history of prior VTE but no history of bleeding, hepatic failure. Her platelet count is 250. • Moderate risk for VTE • Low bleeding risk • VTE ppx: unfractionated heparin VTE Prophylaxis Guideline Low Patient admitted Early ambulation Determine risk of VTE Moderate Or High Risk of VTE Low risk if all 3: • Younger than 40 • Mobile • No thrombotic risk factors Moderate risk: All other patients High risk: ICU patients Low Anticoagulant prophylaxis High Intermittent pneumatic compression Determine bleeding risk High Bleeding Risk • Active gastroduodenal bleed • Bleeding within 3 months prior to admission • Platelet count of < 50 Summary • Be aware of VTE in all hospitalized patients • Assess risk of VTE with every admission • Use pharmacologic prophylaxis with heparin for patients with moderate to high risk of VTE • If pharmacologic prophylaxis is contraindicated due to high risk of bleeding, use intermittent pneumatic compression • Do not use compression stockings References • Guyatt GH, et al. Executive Summary : Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141;7S-47S. • Francis, CW. Prophylaxis for Thromboembolism in Hospitalized Medical Patients. N Engl J Med 2007;356:143844. • Pineo GF. Prevention of venous thromboembolic disease in medical patients. UpToDate, Mar 2012. • Qaseem A, et al. Venous Thromboembolism Prophylaxis in Hospitalized Patients: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2011;155:625-632.