ARDS and Ventilator Management
advertisement

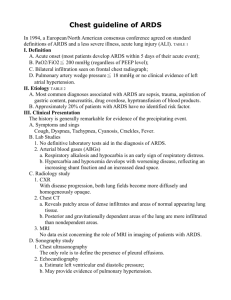
ARDS and Ventilator Management Behrouz Jafari, M.D. Pulmonary & Critical Care Section University of California-Irvine/VA Long Beach 27-year-old woman with dyspnea • 4 days s/p C-section • Gradual increase in dyspnea over 24 hours with fever of 101 • Evaluation – Crackles R > L – No peripheral edema – Hypoxia (7.25/67/41 on 40% VM) – Normal Echo 27-year-old woman with dyspnea • Clinical Course – FiO2 100%; PEEP 20 cm H2O – Peak and plateau airway pressures: 40s 27-year-old woman with dyspnea • Clinical Course – FiO2 100%; PEEP 20 cm H2O – Peak and plateau airway pressures: 40s • Key questions – What is the cause of acute respiratory failure? – How to oxygenate the patient? – How to save her life? Common Causes of Hypoxemic Respiratory Failure Acute lung injury (ALI) / ARDS Pulmonary Edema Diffuse alveolar Hemorrhage Pulmonary Embolism Interstitial lung disease Pneumonia Neoplasm Pulmonary contusion Atelectasis COPD Asthma Bronchiolitis ARDS: Berlin Definition Category Timing Criterion Within 1 week of clinical insult or new/worsening respiratory sx Bilateral opacities – not fully explained Chest Imaging by effusions, lobar/lung collapse, or nodules Origin of edema Not fully explained by cardiac failure or fluid overload. Objective measure to rule out hydrostatic edema Oxygenation: Mild 200 mm Hg < PaO2/FIO2 < 300 mm Hg* Oxygenation: 100 mm Hg < PaO2/FIO2 < 200 mm Moderate Hg** Oxygenation: PaO2/FIO2 < 100 mm Hg** Severe JAMA 2012;307:2526-33 * PEEP or CPAP > 5 cm H2O; ** PEEP > 5 cm H2O • Diffuse bilateral infiltrates – Patchy, confluent – Alveolar, ground-‐glass • In contrast to CHF, no prominence of.. – Cardiomegaly – Pleural effusion – Widened vascular pedicle ARDS: Chest Radiograph Criteria • Radiographic findings not attributable to: – Chronic changes – Atelectasis – Mass – Pleural effusion Lung Compliance in ARDS Volume Normal ARDS Pressure ARDS Triggers - primary vs secondary • Primary - Direct lung injury (eg aspiration, • pneumonia, contusion, inhalation) – Patchy – If it doesn’t evolve into SIRS/MODS, Outcome better than secondary ARDS Triggers - primary vs secondary • • Secondary - Lung is one of many organs involved in SIRS/MODS (sepsis, pancreatitis, hypotension) – Diffuse – Outcome worse than primary ARDS - clinical progression STAGE I DAYS XRAY Initiation Nl PATHOLOGY PMNs ARDS - clinical progression STAGE DAYS XRAY I Initiation Nl II 1-2 days Patchy PATHOLOGY PMNs PMNs, edema, Type I ARDS - clinical progression STAGE DAYS XRAY I Initiation Nl II 1-2 days Patchy III 2-10 days Diffuse PATHOLOGY PMNs PMNs, edema, Type I cell damage Exudate, Type II ARDS - clinical progression STAGE DAYS XRAY PATHOLOGY I Initiation Nl II 1-2 days Patchy III 2-10 days Diffuse cell damage Exudate, Type II IV >10 days Diffuse proliferation Lymph, PMNs PMNs, edema, Type I fibrosis ARDS Mortality Trend ARDS Management ARDS: Blocking the trigger •Appropriate infection management –Antibiotics –Surgical drainage –Foreign body removal ARDS - mediator modulation •Failed trials •Coagulation cascade •Immuno-nutrition ARDS - blocking manifestations •Goals are to “buy time” and avoid complications •Support gas exchange/lung protective ventilator strategies •Assure other components of DO2 are optimal •Altering lung fluid fluxes ARDS Management Mechanical Ventilation : • Low TV (ARDSNET protocol) • Unconventional approach: • APRV • HFV ARDS Management Mechanical Ventilation : • Low TV (ARDSNET protocol) General Measures: • Prone positioning • Nitric oxide • Unconventional approach: • APRV • HFV • NMBA • Fluid Management • ECMO Ventilator Management Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and Acute Respiratory Distress Syndrome 861 Patients 12 cc/kg 6 cc/kg 432 Patients 429 Patients ARDSNET N Engl J Med 2000;342:1301-8 ARDSNET: Setting the Ventilator FiO2 .3 .4 .4 .5 .5 .6 PEEP 5 5 8 .7 .7 .7 .8 .9 .9 .9 1 1 8 10 10 10 12 14 14 14 16 18 18 2024 http://hedwig.mgh.harvard.edu/ardsnet_old/justvent911/justvent911.html Hypothesis of ARDSnet 6 vs 12 Trial Brower et al, AJRCCM 2002;166:1515-17 Brower et al, AJRCCM 2005;172:1241-5 General Measures Effect of Prone Positioning on Oxygenation Gattinoni, et al. N Engl J Med 2001; 345:568-573 prone supine Change in PaO2:FiO2 from baseline to 1h to end of period to next morning • Multicenter RCT comparing prone (n = 237) and supine (n = 229) positioning in severe (P/F <150) ARDS • Multicenter RCT comparing prone (n = 237) and supine (n = 229) positioning in severe (P/F <150) ARDS – > 16 hr / d prone positioning •Prone positioning associated with: – – – – Lower 28 and 90 day mortality More patients extubated at 90 days More ventilator-free days (at 28, 90 d) No difference in complications Guerin et al. N Engl J Med 2013 Inhaled Nitric Oxide • Endogenous vasodilator • Inhalation of 2 - 40 ppm produces selective dilation of pulmonary vessels • Rapidly inactivated by combining with hemoglobin and by oxidation What is the Role for Nitric Oxide in ARDS? • Oxygenation benefit for up to 4 days (5-‐20ppm) • No outcome benefit (survival, duration of mechanical ventilation, ICU LOS) • Routine use of inhaled NO is not supported • Potential role for inhaled NO as rescue therapy for severe refractory hypoxemia ECMO for ARDS • Venovenous (VV-‐ ECMO) for respiratory failure – Blood removed and pumped through oxygenator and returned to circulation; no cardiac support – Large vascular cannula, and coagulation, infection risk The Bottom Line • Identify ARDS using conventional parameters (predisposition / timing, CXR, ABG) • Use “lung protective approach” – 6 ml/kg PBW Vt • Avoid trans-alveolar pressure > 30 cmH2O; • Avoid cyclic alveolar collapse by applying PEEP, particularly for severe ARDS The Bottom Line • Conservative fluid management: aim for balanced I=O • Consider NMBA, prone positioning, NO, or ECMO for severe hypoxemia – moving from least invasive to most invasive. • Prove that it helps to continue rx •Randomized, blinded controlled trial of methylprednisilone vs. placebo for ALI persisting > 7 days •2 mg/kg/day x 14 days; then 1 mg/kg/day x 7 days then tapered over 4 days. Methylprednisilone vs. placebo results Pressure vs Volume-‐Targeted Ventilation in ARDS? • No large, recent (low Vt) RCTs comparing only pressure vs volume-‐targeting • Potential advantages of pressure-‐targeting – Easily adjust inspiratory time – Better patient-‐ventilator synchrony – Avoid regionally excessive transalveolar pressure • Potential advantages of volume-‐targeting – Avoid high tidal volume, simplify implementation MacIntyre & Sessler. Respir Care 2010; 55:43-55 Marini & MacIntyre Chest 2011; 140:286-294 Mortality according to % of recruitable lung RM Techniques CCM 2004:32:2371 Mechanical Ventilation in ARDS: Prolonged Inspiratory Time • Methods – Inspiratory Pause – Decreased PIFR – Prolonged TI • Potential benefits – Higher mean pressure – Autopeep Mechanical Ventilation in ARDS: Prolonged Inspiratory Time • Impaired DO2 • Barotrauma • Need for heavy sedation • Doesn’t work Extended Inspiratory Time and Oxygenation in ARDS Mercat A. et al., Crit Care Med 2001; 29:40 Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and Acute Respiratory Distress Syndrome Male IBW = 50 + 2.3(ht(in) - 60) Female IBW = 45.5 + 2.3(ht(in) - 60) ARDSNET N Engl J Med 2000;342:1301-8 ARDSNET: Setting the Ventilator: Subtleties • RR can be increased to correct pH • VT can be increased for – Dyspnea and breath stacking (if PPl < 30) – PPl < 25 and VT < 6 ml/kg • VT may go as far as 4 ml/kg if needed to keep PPl <30 cmH20 • Paralysis rarely needed (~6%) • Vast majority complied with protocol http://hedwig.mgh.harvard.edu/ardsnet_old/justvent911/justvent911.html Eisner MD et al., Am J Resp Crit Care Med 2001; 164:225 Causes of Death in ARDS (%) n=67 35 30 25 20 15 10 5 0 * MOF/ Sepsis Resp Card Neur Heme Ferring M, Vincent JL. Eur Respir J 1997; 10:1297-1300 Ca Mortality (%) ARDS: Organ Failure(s) and Mortality 100 80 60 40 20 0 0 1 2 3 Ferring M, Vincent JL. Eur Respir J 1997; 10:1297-1300 4 5 Inflammatory Cytokines in ARDS (D1) Survivors Nonsurvivors pg/mL 20 15 10 5 0 TNF IL-1 Headley et al., Chest 1997; 111:1306 IL-8 PFT's > 1 year after ARDS 110 n=16 100 90 80 70 60 FVC Elliot, C.G. et al., ARRD 1987; 135:634 TLC DLCO PFT's In ARDS Survivors 90 80 70 60 FVC 50 TLC 40 DLCO 0 3 6 9 Months After Extubation McHugh, L.G. et al., AJRCCM 1994; 150:90-94 12 ARDS: AECC Consensus Definition Criticism •Problems with the definition: –PEEP not specified –CXR criteria vague • ALI vs ARDS: Does it matter? ALI vs ARDS: Does it Matter? Characteristic ALI (n=66) ARDS (n=221) P/F 239.8 ± 27.1 130.7 ± 37.5 Age 55.0 ± 19.8 61.3 ± 16.5 APACHE II 17.2 ± 7.9 19.2 ± 7.9 Quadrants on CXR 2.8 ± 0.8 3.0 ± 0.9 Mortality (90 d) 42.2% 41.2% Lure, O.R. et al., Am J Respir Crit Care Med 1999; 159:1849 Lung protection tradeoffs: PO2 Crs also better in the HIGH Vt group Lung protection tradeoffs: pH ARDSnet rules allowed pH values as low as 7.15 Unconventional vent. approach ARDS –Unconventional approaches: •Long I time strategies (APRV) •HFOV APRV APRV Concerns: AutoPEEP & Tidal Volume Creep pressure flow Tidal volume 700 650 600 550 500 450 400 6 ml/kg IBW 350 300 10pm 2am 6am 10am Incomplete emptying (i.e. autoPEEP) HFOV – CPAP with a “wiggle” HFOV for Severe ARDS • Multicenter RCT of 548 patients of HFOV vs LTVV (Vt 6 ml/kg, high PEEP) for ARDS (PaO2:FiO2 < 200 mmHg) • Stopped early for harm • HFOV associated with: – Higher mortality (ICU, hosp) – More sedation, NMBA – More vasopressors – Less refractory hypoxemia Ferguson et al. N Engl J Med 2013 HFOV for Severe ARDS • Multicenter RCT of 548 patients of HFOV vs LTVV (Vt 6 ml/kg, high PEEP) for ARDS (PaO2:FiO2 < 200 mmHg) •• Multicenter RCT of 795 UK patients of HFOV vs usual care for ARDS (PaO2:FiO2 < 200 mmHg) • – Vt = 8.3 ml/kg, PEEP 11 cm H2O • Stopped early for harm • No difference in: • HFOV associated with: – 30 day all cause mortality – Higher mortality (ICU, hosp) – ICU, Hosp LOS – More sedation, NMBA – Vent-‐free days – More vasopressors – Less refractory hypoxemia Ferguson et al. N Engl J Med 2013 Young et al. N Engl J Med 2013 ECMO for ARDS • Extracorporeal Life Support (ECLS) • Large RCT in UK : • lower mortality and/or disability in group (but many other Rx differences) Peek et al. Lancet 2009 What PEEP should we choose? High or Low? Pressure vs Volume-‐Targeted Ventilation in ARDS? • No large, recent (low Vt) RCTs comparing only pressure vs volume-‐targeting • Potential advantages of pressure-‐targeting – Easily adjust inspiratory time – Better patient-‐ventilator synchrony – Avoid regionally excessive transalveolar pressure • Potential advantages of volume-‐targeting – Avoid high tidal volume, simplify implementation MacIntyre & Sessler. Respir Care 2010; 55:43-55 Marini & MacIntyre Chest 2011; 140:286-294 ARDS outcome •Long term mortality depends on underlying health status (11% mortality in 1st year) NEJM 2003; 348: 8 ARDS outcome •Long term mortality depends on underlying health status (11% mortality in 1st year) •At one year: – 6 MW 49%, VC 85%, DLCO 72% – PTSD like syndrome –Are these long term effects of hypoxemia? hypotension? drugs ? NEJM 2003; 348: 8 Controversies in VILI Overdistention •Is it “maximal” stretch or “tidal” stretch (or both) that causes VILI? –If “maximal” , goal is to keep Pplat <30 with any VT •Pplat < 30 is “safe” –If “tidal”, goal is to reduce VT and Pplat to minimums •No Pplat is “safe” Stretch injury - Is it max stretch or tidal stretch? Controversies in VILI - Overdistention •Is it “maximal” stretch or “tidal” stretch (or both) that causes VILI? –If “maximal” , goal is to keep Pplat <30 with any VT •Pplat < 30 is “safe” –If “tidal”, goal is to reduce VT and Pplat to minimums •No Pplat is “safe” Steroids in ARDS: • Use of low dose, longer duration steroids is associated with more rapid recovery and may be associated with reduced mortality risk – But, small studies, methodological quality issues Steroids in ARDS: • Use of low dose, longer duration steroids is associated with more rapid recovery and may be associated with reduced mortality risk – But, small studies, methodological quality issues • If use steroids in ARDS – Avoid starting after day 14 – Avoid NMBA – Infection surveillance – Methylprednisolone 2m g/kg/d, taper over 4 weeks Lower Tidal Volumes and Survival in ARDS ARDSNET N Engl J Med 2000;342:1301-8