Uttam G. Reddy, MD Medical Director, Kidney Transplant Program August 11 , 2015
advertisement

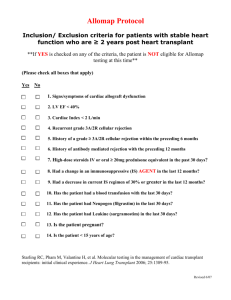
Uttam G. Reddy, MD Medical Director, Kidney Transplant Program August 11th, 2015 Background & Importance of Transplantation Basics of Kidney Transplant Management Immunosuppressive Medications Common Post Transplantation Issues Vaccinations Key drug-drug interactions Summary The first kidney transplant surgery was in December 1954 (over 60 years ago) at what is now Brigham and Women’s Hospital in Boston. The recipient, who received the kidney from his identical twin, lived for 8 more years. The lead surgeon, Dr. John Murray was awarded the Nobel Prize for his work in organ transplantation. Wolfe et al. NEJM 1999 Currently 123, 193 people waiting for lifesaving organ transplants in the US 101,662 are on the KIDNEY transplant waitlist In 2014, 17,105 kidney transplants took place in the United States. The Greater Los Angeles area is represented by the One Legacy Organ Procurement Organization. • O Blood Group: 10 Years • A Blood Group: 7- 8 years • B Blood Group: 8 -10 years • AB Blood Group: 5 - 6 years OPTN/SRTR 2013 Annual Data Report: Kidney AJT Jan 2015. “The Chain” Trailer from Documentary entitled “The Chain” in 2014 OPTN/SRTR Annual Report 2012 OPTN/SRTR Annual Report 2012 More priority for Younger ESRD patients. Active infection Recent Malignancy Uncontrolled psychiatric disorders Lack of social support Substance abuse Severe or Irreversible heart-lungliver disease Can be considered for dual organ transplant AGE????? Some centers have age <70. UCI will evaluate them on a case by case basis. Immunosuppressive drug coverage for 3 years post transplant for Medicare patients Continuation for payment requires either disability OR > 65 years of age Medical coverage 20% co payment beyond year 3 Compared to remaining on dialysis patient’s undergoing kidney transplantation Live longer Have a better quality of life Save on overall medical costs Kidney Transplantation is the optimal therapy for ESRD patients who can undergo transplantation Living Related Unrelated Deceased Directed KDPI < 85% KDPI > 85% Pediatric Dual Kidney Public Health Service (PHS) High Risk Death after Cardiac Death (DCD) Hepatitis C Complexity of Immunosuppressive medications Susceptibility Infection Malignancy CVD Multiple co-morbidities DM Peripheral Vascular Disease Frailty Followed closely by a Transplant specialist (nephrologist or surgeon) for the first 3-6 months.. Thereafter, they are often comanaged by the general nephrologist or primary care provider. Communication between transplant team and outside provider is KEY to post transplant management. Transplant Surgeons Transplant Nephrologists Social Worker Transplant pharmacist Dietician Nursing Coordinators Pre Transplant, Wait-List, Post-Transplant Internal Medicine (PCP, inpatient hospitalizations) General Nephrologists Cardiology (pre and post transplant) Endocrinology (post transplant diabetes) Infectious disease (pre and post transplant) Hematology/Oncology (pre and post) Interventional Radiology Pathology Administrative support Assuming no major post transplant issues, patients are followed up: Twice a week for the first month Once a week for the second month Every 2 weeks for the third month Every 1-3 months for the first year. After 1 year, some centers follow annually. At UCI, we follow every 3 months for the first 3 years. Primary nephrologist/PCP usually get involved in patients care after 3-6 months post transplantation. Dosing of immunosuppressive medications Tacrolimus/CsA, steroid tapering Assessing allograft function Creatinine Urine Protein Screening/Monitoring for infections CMV, BK virus Bone Mineral Disease PTH, Vitamin D, Ca, P Risk for malignancy Skin cancer PTLD Age appropriate cancer screening Every Visit: Basic chemistry panel (includes Mg,Phos,Ca) CBC (with diff is recommended) Urinalysis Immunosuppression drug level ▪ ▪ ▪ ▪ Tacrolimus (Prograf) Cyclosporine (Neoral) Sirolimus (Rapamune) Everolimus (Zortress) Occasional: CMV DNA PCR, BK PCR HgA1c, Vitamin D, PTH, Lipid Panel Urine protein/creatinine ratio (if proteinuria) Induction Agents Thymoglobulin ▪ Rabbit antithymocyte globulin Basilixumab (Simulect) ▪ Chimeric mouse-human Ab (CD-25) of IL-2 Receptor High dose steroids (tapered) Maintenance Agents Calcineurin Inhibitors: Tacrolimus or Cyclosporine Anti-metabolite: Mycophenolate or Azathioprine Steroids: Prednisone mTOR inhibitors: Sirolimus, Everolimus Belatacept (newer medication) – CD80/86 antagonist ▪ Used in place of Tacrolimus or Cyclosportine Outcomes of Renal Allografts 100 80 96 • Radiation • Prednisone • 6-MP 85 90 80 65 Percent 90 65 60 60 60 40 40 20 • AZA •ATGAM • Cyclosporine Emulsion • Tacrolimus • MMF • Dicluzimab • Basiliximab • CY-A • OKT3 45 45 • Thymoglobulin • Sirolimus 35 25 Rejection <12 mo 1 Year Survival 15 0 ‘60 ‘65 ‘70 ‘75 ‘80 ‘85 Year ‘90 ‘95 ‘00 Adapted from Stewart F, Organ Transplantation, 1999 OPTN/SRTR 2013 Annual Data Report: Kidney AJT Jan 2015. General Guidelines to Tacrolimus Dosing Months After Transplant Tacrolimus Goal 0-3 months 8-12 ng/ml 3-6 months 7-9 ng/ml 6-12 months 5-8 ng/ml > 12 months 4-7 ng/ml Dosing is based on checking TROUGH levels of Tacrolimus. IMPORTANT to check Trough levels at 7-8am on all inpatients with kidney transplant. Half life (t ½) is on the order of 12 hours in a steady state for most patients. Strong correlation between AUC and whole blood trough levels. Good estimate of systemic exposure CNI TOXICITY INFECTION REJECTION Allograft dysfunction Elevated Creatinine or Proteinuria Side effects of immunosuppression Co-morbidities DM, HTN, Recurrent disease Infectious disease Anemia Cardi0vascular Disease Malignancy Following transplantation, baseline creatinine tends to be higher than 1.1, which is equivalent to a GFR of less than 60 ml/min per 1.73m2 Single Kidney Ischemic injury (deceased donor) Quality of the Kidney (Elevated KDPI) Use of Calcineurin inhibitors – Vasoconstriction, ATN Size mismatch Pre Renal Over-diuresis or under hydration Diarrhea/GI issues Post Renal Obstruction CNI Toxicity Allograft rejection Recurrent Glomerulonephritis De Novo Renal Diseases (ATN, toxins) Drug induced AIN Renal Artery Stenosis Infection Pyelonephritis BK nephropathy Two Categories of Acute Rejection Cellular (ACR) and Antibody mediated (AMR) Acute Cellular Rejection Interstitial infiltration with mononuclear cells and occasionally eosinophils, and disruption of the tubular basement membranes by the infiltrating cells (lymphocytes, plasma cells, etc) Tubulitis and intimal arteritis are the primary lesions. Antibody Mediated Rejection Capillary endothelial swelling, peritubular capillaritis, arteriolar fibrinoid necrosis, fibrin thrombi in glomerular capillaries, and frank cortical necrosis in severe cases. Donor Specific Ab C4d staining on biopsy – highly suggestive of AMR ACUTE CELLULAR REJECTION AB-MEDIATED REJECTION Acute Cellular Rejection For simple ACR, treatment is pulse dose steroids x 3 days, followed by oral steroid taper If rejection is more severe (significant tubulitis, vascular involvement), treat with Thymoglobulin x 5-7 days. Goal Tacrolimus increases to 8-10 ng/ml during rejection. Antibody Mediated Rejection Plasmapheresis and IVIG If severe, can consider Rituximab More recent studies looking into Eculizumab Monitor Donor Specific Antibodies Recurrent Disease FSGS – 30% IgA Nephropathy – 10-30% Membranous 10-30% Diabetes De Novo Disease Transplant Glomerulopathy Secondary FSGS Diabetes Gallon L, et al. NEJM, 2012; 366,: 1648 Childhood onset of initial FSGS disease. Rapid progression of initial disease. White race. Hx of recurrence in a prior allograft. FSGS Less frequent in African American populations. White recipients of African American kidneys at a higher risk. Histological subtype does not predict recurrence. Family history of FSGS - low risk of recurrence Concern for rejection Unexplained rise in creatinine Concern for BK nephropathy Evaluate for recurrent disease Proteinuria exceeding 1 gram/day Protocol Biopsy Risk of biopsy Bleeding, Damage to other organs, infection, loss of allograft. Complication rate on the order of 0.4-1% Graft loss occurs in 1/2500 biopsies. Furness PN, et al. Transplantation, 2002 Magnesium wasting associated with CNI use. Down-regulation of renal expression of TRPM6 Thought to play a role in NODAT, and CNI toxicity Risk of cardiac arrhythmias. Treat with Mg supplements. New Onset Diabetes after Transplant (NODAT) Insulin metabolism and excretion Hidden Diabetes Transplanted kidney – gluconeogenic Immunosuppression increase blood sugars Tacrolimus Steroids Pre-existing risk factors predispose to DM Develops within the first few months Continued risk for life of patient & allograft Monitor fasting blood sugars and check HgBA1C accordingly Some Centers check HgBA1c at 3, 6, and 12 months, and annually thereafter. Treat with diet modifications, exercise, weight loss, pharmacological options Major cause of graft loss and death Common Infections Opportunistic Infections Higher risk in months 1-3 given that’s when immunosuppression is at its maximum. Can occur anytime, as long as immunosuppressed. Upper respiratory tract infections Common Cold, Pharyngitis, Influenza Similar to general population Urinary tract infections Most common bacterial infection post transplant Avoid prolonged catheterization Could be related to reflux in transplanted kidney High incidence of complicated UTIs Recurrent UTI s Imaging of Transplanted and Native kidneys Cystoscopy Preventive behavioral changes Vitamin C, Hiprex ESBL E.Coli Infection Treatment with IV Carbapenem, Cefepmine Oral treatment with Fosfomycin Please do NOT treat with Macrobid (despite what sensitivites show) Important to keep in mind that many transplant patients have a ureteral stent placed at time of transplant that is typically removed by Urology 4-6 weeks after transplant. Any UA from these patients will show up as positive, so keep this in mind before jumping to start IV Abx in the ER if patient comes in for other complaints in the early post transplant period. Cytomegalovirus (CMV) Hepatitis, Retinitis, PNA, encephalitis, GI Ulcerations Polyomavirus (BK and JC virus) Viruria, Viremia BK Nephropathy Pneumocystis jirovecci pneumonia (PCP) All transplant patients receive prophylaxis for CMV and PCP. CVD remains the major cause of death and graft loss in diabetic renal transplant patients. USRDS 2007 Annual Report Risk Factors: ESRD Anemia DM HTN Obesity Immunosuppressive medications can worsen some of these USRDS Annual Report – Transplantation, 2014 Most patients with ESRD are anemic at time of transplant Transplant factors can perpetuate anemia Surgical blood loss Inflammation Delayed graft function Induction/Immunosuppression agents Antiviral agents Discontinuing of erythropoietin stimulating agents. Typically resolve 6-12 months post transplant Sooner if good allograft function If the patient is not iron deficient Can re-develop later in transplant life with progressive allograft dysfunction, infections, use of ACE/ARB. Persistently elevated HgB/Hct following transplantation Hct >51% (HgB > 17) Occurs in 8-15% of renal transplant patients Typically occurs 8-24 months after transplantation. Treatment: ACE/ARB, and in severe cases phlebotomy. 50% of transplant patients may be categorized as obese or morbidly obese. Gore JL, Danovitch GM. AJT 2006. Weight gain may be related to: Appetite improves after transplant. Effect of steroids may play a part in weight gain. Feeling better in general by being off dialysis Lifestyle modifications, dietary control, and weight loss are frequently emphasized. Cancer after transplantation is 3x more likely than general population. These cancers have 5 fold or > increase in transplant patients Kaposi Sarcoma Skin Cancer Non-Hodgkin Lymphoma Liver Anus/Lip/Vulva Malignancy represents the 3rd most common cause of death in renal transplant recipients. Highest risk is for skin cancer Recommended to screen yearly in most patients and in some high risk patients, every 3-6 months by dermatology. Minimize sun exposure and use UV blocking agents. Consider switching immunosuppression or decreasing immunosuppression Reduction in Trough goal, and MMF dosing Switching CNI to Rapamune (Sirolimus) July 2012 Conclusion: Switching from CNI to Sirolimus had an anti-tumoral effect in kidney transplant patients with previous squamous cell carcinoma. Overall level of immunosuppression appears to be related to post transplant malignancy. Induction Agents Buell JF. Transplantation, 2005 Increased Cancer Risk with T-Cell Depleting Antibody therapy such as Thymoglobulin Reddy U. Nature Reviews Nephrology, 2014 Coexisting Viral Infection associated with Malignancy: EPV, HHV-8, HPV, Merkel Cell Polyomavirus Post Transplant Lymphoproliferative disease Lymphoid and/or plasmacytic proliferations related to immunosuppression that can occur in transplant patients. Most common malignancy after skin cancer in solid organ transplants Usually EBV+ [most common in EBV-(R)/EBV+(D)] Related to B-cell proliferation induced by EBV infection. Host derived (multisystem) or donor derived (allograft) 62 year old male ESRD due to HTN s/p DDRT in July 2013. Induction: Simulect. 7 months after transplantation, presented with nausea, malaise, and found to have AKI with creatinine of 1.8. Ultrasound of his allograft was done which revealed a soft tissue mass at the hilum of his kidney. Reduction in Immunosuppression Stop Mycophenolate Decrease trough Prograf levels Consider switching Prograf to Sirolimus Referral to Hematology-Oncology If lesion is Cd20+ Rituximab Chemotherapy (EPOCH) In certain cases: Surgery, XRT SIMPLE RULE OF THUMB: “Do NOT give patients LIVE or LIVE ATTENUATED VACCINES after transplantation” Do Not Give these: Varicella Zoster Intranasal Influenza Bacillus Calmette-Guerin (BCG) Live oral typhoid Measles Mumps Rubella Oral polio Live Japanese B encephalitis vaccine Yellow fever Smallpox Okay to give INACTIVATED vaccines. Influenza (type A and B) – yearly Pneumovax (Prevnar-13)– every 3-5 years Haemophilus influenza B Hepatitis B Typhoid Vi Inactivated polio Meningococcus Hepatitis A A transplant patient on the same tacrolimus dose for 5 years started on a health food diet and over-the-counter herbal products. The transplant center noted that his tacrolimus levels have abruptly decreased to unacceptably low levels, putting him at risk for rejection. The nurse coordinator accused him of being noncompliant, but the patient insisted he was taking his medication as prescribed. What is your assessment? A. This patient is becoming noncompliant after 5 years and is in denial; he needs an immediate psychiatry consult B. This patient is taking grapefruit extracts, which are preventing the absorption of his tacrolimus. C. This patient is taking St. John’s Wort. D. This patient is taking creatine supplements, which increase the activity of Pglycoprotein, leading to enhanced tacrolimus excretion E. This patient is taking echinacea, which activates renal tubular excretion of tacrolimus. CYP1A2 CYP2C9 CYP2C19 CYP2D6 CYP2E1 CYP3A4 Tylenol Caffeine Theophylline Diclofenac Fluvastatin Phenytoin Tolbutaminde Warfarin Diazepam Ibuprofen Mephenytoin Omeprazole Phenytoin Proguanyl Amitriptyline Codeine Flecainide Imipramine Metoprolol Nortriptyline Propafenone Propanolol Thioridazine Tylenol Ethanol Halothane Amiodarone Atorvastatin Timolol CYTOCHROME P450 ISOENZYMES Metabolize many clinically relevant drugs Clarithromycin Cyclosporine Diltiazem Erythromycin Everolimus Itraconazole Ketoconazole Lovastatin Midazolam Nefazodone Nifedipine Protease Inhib. Quinidine Sildanefil Simvastatin Sirolimus Tacrolimus Terbinafine Verapamil Warfarin Class Inhibiting Drugs Antibacterial (macrolide) Clarithroymycin, Erythromycin Antidepressants Fluvoxamine, Nefazodone Azole Antifungals Fluconazole, Voriconazole, Itraconazole etc Calcium Channel Blockers Diltiazem, Verapamil Foods Grapefruit, pomegranate Protease Inhibitors (Hep C) Boceprevir, Telaprevir Protease Inhibitors (HIV) Atazanavir, darunavir Fosamprenavir, indinavir Nelfinavir, ritonavir, saquinavir Others Amiodarone, Dalfopristin Statins Tacrolimus/Cyclosporine Class Inducing Drug Antiseizure Medications Carbamazepine Fosphenytoin Oxcarbazepine Phenobarbital Phenytoin Anittuberculosis Rifabutin Rifampin Antiviral Efavirenz Others Bosentin Modafanil St. John Wort A transplant patient on the same tacrolimus dose for 5 years started on a health food diet and over-the-counter herbal products. The transplant center noted that his tacrolimus levels have abruptly decreased to unacceptably low levels, putting him at risk for rejection. The nurse coordinator accused him of being noncompliant, but the patient insisted he was taking his medication as prescribed. What is your assessment? A. This patient is becoming noncompliant after 5 years and is in denial; he needs an immediate psychiatry consult B. This patient is taking grapefruit extracts, which are preventing the absorption of his tacrolimus. C. This patient is taking St. John’s Wort. D. This patient is taking creatine supplements, which increase the activity of Pglycoprotein, leading to enhanced tacrolimus excretion E. This patient is taking echinacea, which activates renal tubular excretion of tacrolimus. Transplant Nephrology service is here to serve you for ALL Kidney Transplant patients Consists of Renal Fellow on Service, and myself. All day, everyday. We have clinics - 4 days a week – soon to be 5 days a week. Please check Prograf/CsA/Everolimus/Sirolimus levels EVERYDAY at 7-8am (TROUGH levels) for any inpatient transplant patient who remains on immunosuppression. Please page Transplant Nephrology IMMEDIATELY for all admitted patients or any patient in the ER who there is a question on. Consult Transplant Nephrology on ALL Kidney, and Kidney-Pancreas transplant patients All patients within the first year of K/KP transplant will be admitted to Transplant Surgery team (unless otherwise indicated) Think twice before considering PICC line in a transplant patient. Discuss PICC lines with Transplant Nephrology BEFORE ordering them. Placing a PICC jeopardizes future AV access by the dilation of vein by PICC line placement. Hoggard J, et al. Semin Dial, 2008 Home health can alternate IVs to avoid PICC Slightly longer hospital stay Oral Antibiotic alternatives Close follow up Kidney transplant is the treatment of choice in terms of renal replacement therapy for a majority of ESRD patients. Multi-disciplinary approach Only Inactivated Vaccines are okay after transplant. Increased comfort level in dealing with kidney transplant patients, their immunosuppression, and common post transplant management issues. Transplant Nephrology Service is here to happily SERVE you for all your Kidney Transplant patients. Uttam G. Reddy, MD Pager = 714-506-0846 Email = ureddy@uci.edu