Acute Kidney Injury - Mini Lecture Updated 02/2013

TEACHING · RESEARCH · PUBLIC SERVICE
Acute Kidney Injury - Mini Lecture
Updated 02/2013
Objectives
• Quickly and easily identify and workup acute kidney injury.
Background
• The incidence of AKI is estimated at 1% of patients that present to the hospital and 7-50% of patients in the ICU.
• Part of the initial history should be determining every patients baseline Cr.
• May present as Uremia (malaise, anorexia, nausea, vomiting), but is usually asymptomatic.
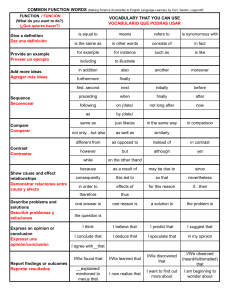
• Acute Kidney Injury Network (AKIN) Criteria
Stage Cr Criteria
1
2
3
Cr ↑by 1.5-2x baseline or
Cr ↑by 0.3 mg/dl
Cr ↑by 2-3x
UOP Criteria
< 0.5 ml/kg/hr for 6hr
< 0.5 ml/kg/hr for 12hr
Cr ↑by more than 3x or Cr↑by
0.5 if baseline >4mg/dl
< 0.3 ml/kg/hr for 24hr
Or anuria for 12h
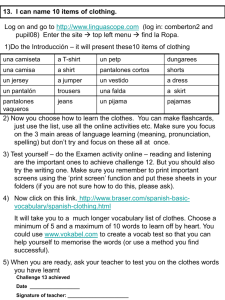
AKI can be Prerenal, Intrinsic or Postrenal
Acute Kideny Injury
Prerenal
Uosm > 5000 mosm/kg
Una < 20meq/L
FEna < 1%
Microscopy - bland
Intrinsic Renal Diseases
Postrenal
Uosm: variable
Una: low early, high late
FEna: variable
Microscopy - bland
Ischemic / Toxic ATN
Uosm ~ 300 mosm/kg
Una > 40meq/L
FEna > 2%
Microscopy – dark pigment cast
Acute Interstitial Nephritis
Uosm: variable, ~300 mosm.kg
Una > 40 meq/L
FEna > 2%
Microscopy – leukocytes, erythrocyts, leukocyte casts
Acute Glomerulonephritis
Uosm: variable (>400 in early GN)
Una: variable (<20meq/l in early GN)
FEna: variable, <1% in early GN
Microscopy
– hematuria, proteinuria
Erythrocyte casts (dysmorphic)
Prerenal Azotemia
• Prerenal azotemia is the most common cause of acute kidney injury in the outpatient setting
– Look for patients with decreased PO, diarrhea, vomiting, tachycardia, orthostasis….
– Order: UA, Uosm, Una, Ucr, BMP, Uurea (if on diuretics)
• The kidney functions properly in patients with prerenal azotemia.
– True volume depletion can be treated with normal saline.
– Decreased effective arterial blood volume can be present in CHF, Cirrhosis or nephrotic syndrome.
Treatment should focus on the underlying disease.
Intrinsic Kidney Diseases
• ATN - Acute Tubular Necrosis
– Usually occurs after an ischemic event or exposure to nephrotoxic agents.
– Look for muddy brown casts and FeNa>2%
• AIN - Acute Interstitial Nephritis
– Classic presentation is fever, rash, eosinophilia and Cr bump 7-
10 days after drug exposure.
– Urine may show leukocytes, leukocyte casts and erythrocytes, cultures will be negative.
• CIN - Contrast Induced Nephropathy
– Increased Cr of 0.5mg/dl or 25% 48hrs after contrast administration.
– Prevent with NS or isotonic fluid+sodium bicarb, hold NSAIDs, metformin and diuretics (in patients without fluid overload).
• Others – Glomerular Disease, Pigmented Nephropathy,
Thrombotic Microangiopathy
Postrenal Disease
• Obstruction anywhere in the urinary tract
– Bladder outlet obstruction can be seen with bladder scan and relieved with catheterization
– Ureteral obstruction and hydronephrosis may be seen on ultrasound and noncontrast CT
– Order: Order: UA, Uosm, Una, Ucr, BMP, Uurea (if on diuretics)
• Patients often have a history of pelvic tumors, irradiation, congential abnormalities, kidney stones, genitourinary, procedures or surgeries, and prostatic enlargement.
AKI can be Prerenal, Intrinsic or Postrenal
Acute Kideny Injury
Prerenal
Uosm > 5000 mosm/kg
Una < 20meq/L
FEna < 1%
Microscopy - bland
Intrinsic Renal Diseases
Postrenal
Uosm: variable
Una: low early, high late
FEna: variable
Microscopy - bland
Ischemic / Toxic ATN
Uosm ~ 300 mosm/kg
Una > 40meq/L
FEna > 2%
Microscopy – dark pigment cast
Acute Interstitial Nephritis
Uosm: variable, ~300 mosm.kg
Una > 40 meq/L
FEna > 2%
Microscopy – leukocytes, erythrocyts, leukocyte casts
Acute Glomerulonephritis
Uosm: variable (>400 in early GN)
Una: variable (<20meq/l in early GN)
FEna: variable, <1% in early GN
Microscopy
– hematuria, proteinuria
Erythrocyte casts (dysmorphic)
Practice Question
A 74 year old man was hospitalized 3 days ago with cellulitis. He has a history of HTN, HLD, PVD and has been non-compliant with his medications. At presentation, his vitals were T-37, BP-170/90, HR-90, RR-20 and Cr was
1.5. He was started on Cefazolin and his home meds
(Lisinopril, Metoprolol, HCTZ, Amolodipine, Pravastatin and
ASA) were restarted.
Today, his vitals are T-37, BP-110/55, HR-60, RR-16 and his Cr is 2.7, FeNa-2.3%, FeUrea-51%, UA shows trace protein and occasional Granular casts. UOP has been stable.
What is the most likely cause of his AKI?
A. Acute Interstitial Nephritis
B. Benign Prostate Hypertrophy
C. Acute Tubular Necrosis
D. Prerenal Azotemia
Take Home Points
• Identify AKI early on
– Monitor serum Cr for at risk patients
– Make sure I/Os are recorded correctly
• Diagnose as Prerenal, Intrinsic or Postrenal
– Detailed history
– Order routine labs including BMP, UA, Uosm, Ucr,
Una (Urine Urea if on diuretics)
– Imaging studies as necessary
• Begin appropriate treatment
– Stop offending agent
– Fluids if appropriate
– Relieve obstruction
– Renal dosing of meds