Gout
advertisement

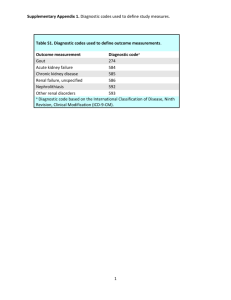
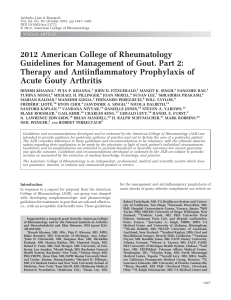
Gout Gout • The most common cause of inflammatory arthritis in US adults (3.9% of Americans; approx. 8.3 million people; 2007-2008) • Prevalence is greater in men (5.9%; 6.1 million) than women (2.0%; 2.2 million) • Prevalence has increased by 1.2% points over the past 2 decades • Incidence of gout 2x greater among black men than white men • Men with gout have been shown to have an increased risk of allcause mortality and cardiovascular disease mortality • Cost: 2.3 million ambulatory care visit annually from 2001-2005; multiple hospitalizations; $7.7 billion attributable to gout between 2005-2011 Pathophysiology • Caused by the deposition of monosodium urate crystals in tissues • Uric acid is a metabolic by-product of purine catabolism • Purineshypoxanthinexanthineuric acid • Reaction catalyzed by xanthine oxidase, found in the liver • When the balance of dietary intake, synthesis and rate of excretion are disrupted, hyperuricemia results – Overproduction (10%) – Underexcretion (90%) • Results in arthritis, soft tissue masses, nephrolithiasis and urate nephropathy Pathophysiology Rees, F. et al. (2014) Optimizing current treatment of gout Nat. Rev. Rheumatol. doi:10.1038/nrrheum.2014.32 Risk Factors • • • • • • • • • High Purine Diet (Red Meat, Fatty Poultry, High Fat Dairy, Seafood) Alcohol Consumption Trauma Osteoarthritis Surgery Starvation Dehydration Obesity Drugs (Allopurinol, uricosuric agents, thiazides, loop diuretics, low dose aspirin) • Renal Impairment • Genetic Mutations (SLC22A9, SLC22A12, ABCG2) Stages of Gout • • • • Asymptomatic tissue deposition Acute Gouty Arthritis Intercritical Gout Chronic Articular and Tophaceous Gout Acute Gout • Often presents as involvement of a single joint or multiple joints in the lower extremities: first metatarsophalangeal (podagra; 50% of people with gout), midtarsal, ankle and knee joints • Characterized by pain, erythema, swelling and warmth. Can have desquamation of skin. • Can even cause fever and leukocytosis • Maximal severity reached within 12-24 hours • Even without treatment, attacks subside within days to several weeks Chronic Gout • Characterized by chronic arthritis and tophi, resulting in chronic inflammatory and destructive changes Renal Complications • Nephrolithiasis – Risk factors: increase uric acid excretion, reduced urine volume, and low urine pH • Chronic urate nephropathy – Urate crystals can deposit in renal medullary interstitium producing inflammatory changes and fibrosis – Clinical features are non specific: renal function impairment, bland urinary sediment, mild proteinuria and serum urate concentrations often higher than expected for the degree of renal impairment. – Biopsy confirms diagnosis Diagnosis • DDX: Pseudogout and Septic Arthritis Diagnosis • 5 clinical classification criteria for gout currently exist: Rome, New York, ACR, Mexico and Netherlands • These classification criteria have not been extensively validated • Diagnosis should be based on combination of clinical, historical and laboratory data if arthrocentesis cannot be performed. Diagnosis is considered provisional. Diagnosis • Arthrocentesis should be done in patients in whom the diagnosis has not been previously established . • Labs: cell count with differential, gram stain, culture, examination for crystals under polarized light microscopy Treatment Treatment Treatment • When initiating urate lowering therapy, can precipitate acute gouty arthritis. Therefore, prophylaxis often given Diet Recommendations for Practice References • • • • Mayo Clinic UptoDate CDC Khanna,D., et. al. 2012 American College of Rheumatology Guidelines for Management of Gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care and Research, Vol. 64, No. 10, October 2012, pp 1431-1446 • Choi, H., et. al. Pathogenesis of Gout. Physiology in Medicine. Annals of Internal Medicine. Vol. 143, 2005, pp 499-516 • Eggebeen, A. Gout: An Update. American Academy of Family Physicians. 2007. http://www.aafp.org/afp/2007/0915/p801.html • Dalbeth, N. et al. New Classification criteria for gout: a framework for progress. Rheumatology (2013).