Point of Injury Burn Care Anil Menon, MD, MS
advertisement

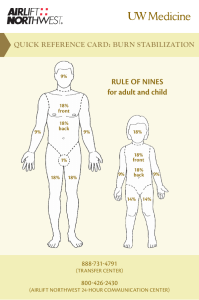
Point of Injury Burn Care Anil Menon, MD, MS UTMB/NASA-JSC Aerospace Medicine Residency Aerospace Medicine Grand Rounds August 23rd 2011 Disclosures • None Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases 26 SEP 1983 / Soyuz T-10-1 19 APR 2008 / Soyuz TMA‐11 Space Related Burns and Fires • Bondarenko - 1961 Space Related Burns and Fires • Apollo 1 – 1967 Space Related Burns and Fires • Apollo 12 – 1969 Space Related Burns and Fires • STS-9 - 1983 Space Related Burns and Fires • STS-41D – 1984 Space Related Burns and Fires • MIR – 1997 Space Related Burns and Fires • Robertson - 2001 Question? What one factor might account for the reduction of burn related deaths from 12,000 per year in 1979 to 6000 in 1990 in the United States? Prevention • Primary – Fire-retardant clothes, materials, fuel tank • Secondary – Extinguishers, fire response • Tertiary – Immediate and long-term burn care Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases Pathophysiology • Zone of coagulation – Cell/proteins destroyed – no blood flow • Zone of stasis – Cell/proteins damaged – decreased blood flow • Zone of hyperemia – Inflammation area Physiology • • • • Emergent phase Fluid shift phase Hypermetabolic phase Resolution phase Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases Depth Superficial Partial Thickness Classification of Burn Depth Full Thickness Full Thickness (3rd Degree) – Destruction of all epidermal and dermal elements – Burn into subcutaneous fat or deeper – Skin is charred and leathery Pearly-white sheen / waxy – Generally not painful Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases PHTLS • Scene safety • Source control • Patient safety Kandahar POLYTRAUMA • MOST BURN PATIENTS NEED A RAPID TRAUMA ASSESSMENT, NOT A FOCUSED BURN ASSESSMENT • Remember PHTLS and ATLS POLYTRAUMA Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases Outline • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs – Airway – Intubation / Inhalation – Breathing – Escharotomy / Ventilation – Circulation – Fluid resuscitation Airway – Thermal – Cyanide – CO – Smoke Smoke Inhalation CASE • 54 yo male working on gas stove when it exploded • In house • Singed nasal hairs, facial burns, intubated in ED Inhalation Injury CASE • 29 yo male working a deionizing machine at coal plant • Difficulty in breathing • Intubated in the field Breathing Ventilation • Tracheobronchial and pulmonary edema – Fluids – ARDS – PNA • 1-3 days high risk period • ARDSnet 6ml/kg • • • • Pressure-limited, time-cycled, 5 Hz 362 -> 31 per arm, RCT Severe hypoxemia and hypercapnia LTV 29% vs HFPV 6% Circulation • Fluids – Rule of 9’s – Rule of hand – Lund-Browder • Insensible loss • Third spacing Lund‐B Circulation Circulation • Parkland (modified brooke use 2ml) – 4 ml * kg * %TBSA/24 hours – 50% over 1st 8 hours since time of burn – 50% over next 16 hours • 40 year old healthy female weighs 70 kg and 50% burned at 1300 hours • 4*70*50 =14000ml/2 =7000ml/8 =875ml/hr Rule of 10s • Estimate burn size to nearest 10 – %TBSA x 10 = initial rate mL/hr (for adult weights) – Increase 100 mL/hr for every 10kg above 80kg • Previous patient – 50*10 = 500ml/hr • Insufficient data to support standard of care (Brooke / Parkland / Pre-hospital ) • > 20 % TBSA require fluid resuscitation • Use 2-4 ml/kg/%TBSA/24 hours • Titrate to UOP of 0.5-1 ml/kg/hr • Increase volume for full thickness, delayed care, inhalation injuries Monitoring Response • If UOP < target for 1-2 hours increase infusion by 20-25% • If UOP > target for 1-2 hours decrease infusion by 20-25% • Diuretics are NEVER indicated to establish UOP – Can be used when gross pigmenturia is present AND patient has been appropriately resuscitated – euvolemic • HR is a very poor indicator of volume status – Significant systemic inflammation with burns • Consider BP/CVP/SvO2/HCT/BE Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases Question? In general, moderate to severe burns should be cared for with: A. B. C. D. E. moist occlusive dressings dry sterile dressings cool water immersion plastic wrap covered by a soft dressing warm water immersion Topical • • • • • • • • Bacitracin (bad gram neg and yeast) Polymyxin (bad gram pos) Muprocin (MRSA) Neomycin (strong gram neg only) Silver sulfadiazene (Broad coverage) Mafenide (Broad coverage) Nanocrystals Use only if transfer time is > 12 hours Silver Sulfadiazine (Silvadene) • Effective Against GPC, GNR, and Fungus • Soothing • Poor Eschar Penetration • May cause a transient leukopenia (5-15%), anemia Mafenide Acetate (Sulfamylon) • Effective against GPC and GNR but NOT effective against fungus • Good Eschar Penetration Painful • Metabolic Acidosis can result from use (Carbonic Anhydrase Inhibition) • Cream or 5% solution ISS Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases Fluid Creep • Retrospective studies 40% overresuscitation • Average volumes administered 5-7 ml/kg/TBSA • Excess fluid administration causes – Overestimation of size, EGDT, opioids, not UOP • Life-threatening results Abdominal Compartment Syndrome Resuscitation Under-resuscitation Over-resuscitation • Worsening acidosis • Renal Failure • Hemodynamic Instability • Multisystem organ failure • Cardiac Dysrhythmia • Death • Airway Obstruction • Extremity compartment syndromes • Abdominal compartment syndrome • Multisystem organ failure • Death Difficult Burn Resuscitation Decreased Urine Output • Invasive central pressure monitoring – Goal CVP 8-10 mm Hg – Goal ScVO2 60-65% • Bladder pressures every 4 hours • 5% Albumin Protocol If CVP not at goal • Increase crystalloid/5% albumin rate If ScVO2 not at goal and HgB <10 • Transfuse PRBC If CVP and ScVO2 at goal then • • Vasopressin 0.04 Units/min Dobutamine 5-20 µg/kg/min (Norepi 520 µg/min) Difficult Burn Resuscitation Decreased Urine Output • Hypotension must be individualized – MAP > 55 mm Hg likely adequate to maintain UOP/end organ perfusion – Burn with head injury vs No head injury Outline • • • • • • • • Introduction and background Pathophysiology Classification Point of injury treatment considerations Initial stabilization and ABCs Topical care Advanced and difficult management Cases Case Race driver suffers superficial partial thickness burns to the hands one-week prior to the race, how can you treat? Blister • Evidence supports leaving blisters intact – Barrier to infection – Moist environment promotes reepithelialization – Enhanced angiogenesis – Healing enhanced by blister fluid cell mediators (calmodulin, IL-1, FGF) • Tension can cause pain Burn Classification CCATT Transport considerations • Decision to fly (pre-treat or test) • Decompress Foley / NGT / ETT • Contact destination burn center • Avoid infection risk (transport time?) • Protect lungs • Monitor resuscitation goals Conclusion • Polytrauma – Scene safety, A…B…C… • Calculate fluid requirements – then watch clinical response • Over-resuscitation – BAD • Under-resuscitation – BAD • Prophylactic IV/PO antibiotics – Bad • Topical antibiotics – Good > 12 hrs • Remember: – Early intubation – Escharotomy – Chest wall and extremities – Fasciotomy – If escharotomy fails to restore circulation • Resuscitation Guidelines Acknowledgments • • • • • • • • • Walter Ingram, MD (Chief Grady Burn Unit) Richard Jennings, MD Shannan Moynihan, MD Jim Cushman, MD Melinda Hailey, RN Julie Wells, RN Bob Patlach Chris Robinson (Global Rescue) Warren Dorlac, MD (USAF/CSTARS)