2/21/2012
advertisement

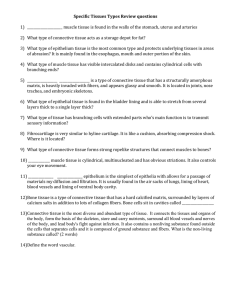
2/21/2012 Connective Tissue – What is it? Connective Tissue??? • It Binds, It Supports, It Strengthens, It Protects, It Insulates, It Compartmentalizes, It helps us move, It helps transport stuff, It is a site for storing energy, It is involved in our immune system, It helps heat us when we were itty bitty babies!!! • All Connective tissue is: • Living cells within a non-living extracellular matrix - Extracellular Matrix (stuff between cells): 1. Protein Fibers 2. Ground substance 3-1 3-2 2. Connective Tissue • Cells rarely touch due to extracellular matrix • Matrix: Protein fibers & ground substance secreted by cells • Consistency varies from liquid, gel to solid • Good nerve & blood supply (except cartilage & tendons) • Most abundant, widely distributed, and histologically variable of the primary tissues Components of Connective Tissue 1. Cells 2. Non-living matrix - Protein fibers - Ground substance 1. Cells: 2. blast type cells = 1) can divide & 2) secrete matrix (fibroblasts, chondroblasts, & osteoblasts) • cyte type cells = mature cells: reduced ability to divide or produce matrix (chondrocytes & osteocytes) 5-4 3-3 Components Connective Tissue Components of Fibrous Connective Tissue more cells: 2. Non-living matrix • leukocytes or white blood cells - Types of Connective Tissue Fibers: • Macrophages (develop from WBC) – engulf bacteria & debris by phagocytosis 1. • Plasma cells (develop from WBC) – produce antibodies (proteins) that help attack foreign substances • Mast cells produce heparine & histamine Collagen (25% of protein in your body) - tough, resistant to pull, yet pliable – tendons, ligaments, and deep layer of the skin are mostly collagen 2. Elastic (protein elastin) – can stretch and return to shape! – very thin fibers 3. Reticular (spleen and lymph nodes) – Support and strength – thin collagen fibers coated with glycoprotein • Adipocytes store fat 3-5 3-6 1 2/21/2012 Components of Fibrous Connective Tissue 2. Non-living matrix - ground substance: – usually gelatinous to rubbery consistency resulting from three classes of large molecules – glycosaminoglycans (GAG) – proteoglycan – adhesive glycoproteins – • Regulate H2O balance • Slippery lubricant • Adhesive 5-7 3-8 Types of connective tissue 1. 2. 3. 4. 5. 6. 7. Loose Connective Tissues • Loose connective tissue (2) Dense connective tissue (2) Adipose tissue Cartilage (3) Bone (2) Blood Lymph? Loosely woven fibers throughout tissues 2 Types of loose connective tissue 1. areolar connective tissue 2. reticular tissue 3-9 3-10 Areolar Tissue Areolar Connective Tissue Ground substance • Gelatinous ground substance • Few random protein fibers (all 3 types) • All 6 cell types • Below our epithelial layer ! (a) Collagenous fibers Fibroblasts (b) Figure 5.14a 3-11 Elastic fibers Figure 5.14b,i 5-12 2 2/21/2012 Reticular Tissue Reticular Connective Tissue Reticular fibers Leukocytes (a) (b) a: The McGraw-Hill Companies, Inc./Al Telser, photographer Figure 5.15a Figure 5.15b,i • Network of fibers & cells that produce framework to hold some organs together 5-14 3-13 1. Dense Regular Connective Tissue Dense Connective Tissue • More fibers present but fewer cells • Types of dense connective tissue: 1. dense regular connective tissue 2. dense irregular connective tissue • Collagen fibers in parallel bundles with fibroblasts 3-16 3-15 2. Dense Irregular Connective Tissue Dense Irregular Connective Tissue Bundles of Gland collagen fibers ducts • Collagen fibers are irregularly arranged (interwoven) • Tissues can resist tension from any direction • Very tough tissue e.g., dermis of skin 3-17 (a) Fibroblast Ground nuclei substance (b) a: © The McGraw-Hill Companies, Inc./Dennis Strete, photographer Figure 5.17a Figure 5.17b,i 5-18 3 2/21/2012 Adipose Tissue Adipose Tissue Blood vessel (a) • • • • • Adipocytes (store triglycerides) Peripheral nuclei Deeper layer of skin, organ padding, yellow marrow Reduces heat loss, energy storage, protection Brown fat??!!! Adipocyte nucleus Lipid in adipocyte (b) Figure 5.18a Figure 5.18b,i 5-20 3-19 Hyaline Cartilage Cartilage • • • Network of fibers in rubbery ground substance Resilient and can endure more stress than loose or dense connective tissue Types of cartilage: 1. hyaline cartilage (invisible fibers) 2. fibrocartilage (thick collegen bundles) 3. elastic cartilage (visible elastic fibers) • Chondrocytes!! sit in spaces called lacunae • No blood vessels or nerves so repair is very slow Articular cartilage 3-22 3-21 Elastic Cartilage Hyaline Cartilage Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Matrix (a) Cell nest Perichondrium Lacunae Chondrocytes (b) a: © Ed Reschke Figure 5.19a Figure 5.19b,i • Elastic fibers help maintain shape after deformations • Ear, nose, vocal cartilages 5-23 3-24 4 2/21/2012 Elastic Cartilage Perichondrium (a) Elastic fibers Fibrocartilage Lacunae Chondrocytes (b) • Many more collagen fibers causes rigidity & stiffness • Strongest cartilage (intervertebral discs) • No perichondrium a: © Ed Reschke Figure 5.20a Figure 5.20b,i 5-25 Fibrocartilage 3-26 Bone tissue (osseous tissue) Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Collagen fibers (a) • Chondrocytes Bones protect organs, allow for movement, store minerals, sites of blood cell formation • ‘bone’ has two meanings: – an organ of the body; femur, mandible; composed of multiple tissue types – bone tissue – osseous tissue – makes up most of the mass of bone (b) a: Dr. Alvin Telser Figure 5.21a Figure 5.21b,i 5-27 2 types of bones: Compact and Spongy 1. Compact bone – solid, dense bone – basic unit of structure is osteon (haversian system) 3-28 Compact Bone Blood • Osteon = lamellae (rings) of mineralized matrix – calcium & phosphate---give it its hardness – interwoven collagen fibers provide strength • Osteocytes surrounded by lacuna 3-29 • Connective tissue with a liquid matrix = ?? • Cell types = red blood cells (erythrocytes), white blood cells (leukocytes) and cell fragments (platelets) • Transport things • immune functions & clotting 3-30 5 2/21/2012 (1) Mucous Membranes Membranes • • • Epithelial layer sitting on a thin layer of connective tissue (lamina propria) Combo of epithelial & underlying CT layer = epithelial membrane Types of membranes: 1. mucous membrane 2. serous membrane 3. synovial membrane 4. cutaneous membrane (skin) • Lines cavity that open to the outside – e.g., mouth, vagina, anus, respiratory • Tight junctions between cells • Mucous secreted by ????? 3-32 3-31 (2) Serous Membranes • Simple squamous cells overlying CT layer • Squamous cells secrete slippery fluid • Internal cavities (not open to the outside) Examples: – pleura, peritoneum and pericardium – membrane on walls of cavity = parietal layer – membrane over organs in cavity = visceral layer 3-33 (3) Cutaneous membrane (skin) 3-34 (4) Synovial Membranes Muscle • • • Line joint cavities of freely movable joints • No epithelial cells -- just special cells that secrete slippery fluid 3-35 Cells that shorten (myocytes) Provide us with motion, posture and heat • Types of muscle: 1. skeletal muscle 2. cardiac muscle 3. smooth muscle 3-36 6 2/21/2012 Skeletal Muscle Cardiac Muscle • Cells are long cylinders with many peripheral nuclei • Visible banding (looks striated) • Voluntary • Cells are branched cylinders with one central nuclei • Involuntary • striated 3-37 Smooth Muscle 3-38 Tissue Growth • Increasing the number of cells or the existing cells grow larger • hyperplasia - tissue growth through cell multiplication • Spindle shaped cells with a single central nuclei • Walls of hollow organs (blood vessels, GI tract, bladder) • Involuntary and nonstriated 3-39 Sebaceous gland cell Fertilized egg Skin cell Stem cell Stem cell Neuron Astrocyte Progenitor cell cells Bone cells Progenitor cell • neoplasia – development of a tumor (neoplasm) – benign or malignant – composed of abnormal, nonfunctional tissue 5-40 Tissue Repair Sperm Egg • hypertrophy - enlargement of preexisting cells – muscle growth through exercise – accumulation of body fat • regeneration - replacement of dead or damaged cells by the same type of cell as before – restores normal function – skin injuries and liver regenerate • fibrosis - replacement of damaged cells with scar tissue – holds organs together – does not restore normal function • severe cuts and burns, healing of muscle injuries, scarring of lungs in tuberculosis one or more steps Fibroblasts (a connective tissue cells) produces another stem cell (self-renewal) 5-42 Blood cells and platelets 7 2/21/2012 Wound Healing Wound Healing • severed blood vessels bleed into cut • mast cells and damaged cells release histamine – inhibits spread of pathogens from injury site to healthy tissue – dilates blood vessels – increases blood flow to area – makes capillaries more permeable • forms scab that temporarily seals wound and blocks infection • blood plasma seeps into the wound carrying: • macrophages phagocytize and digest tissue debris 1 Bleeding into the wound – antibodies – clotting proteins – blood cells – transform into soft mass – granulation tissue – macrophages remove the blood clot – begins 3-4 days after injury and lasts up to 2 weeks Scab Blood clot Macrophages Fibroblasts Leukocytes 2 Scab formation and macrophage activity Figure 5.33 (2) 5-43 Wound Healing • deeper portions become infiltrated by capillaries and fibroblasts • blood clot forms in the tissue 5-44 Wound Healing • surface epithelial cells (mitosis) Scab • connective tissue undergoes fibrosis Macrophages Fibroblasts Blood capillary • remodeling (maturation) phase begins several weeks after injury and may last up to two years Granulation tissue 3 Formation of granulation tissue (fibroblastic phase of repair) Figure 5.33 (3) • scar tissue may or may not show through epithelium 5-45 Epidermal regrowth Scar tissue (fibrosis) 4 Epithelial regeneration and connective tissue fibrosis (remodeling phase of repair) Figure 5.33 (4) 5-46 Tissue Shrinkage and Death • atrophy – shrinkage of a tissue through a loss in cell size or number – senile atrophy (aging) – disuse atrophy (no use) • necrosis – premature, pathological death of tissue (trauma, toxins, or infections) • apoptosis - programmed cell death 5-47 8