= ? Uncertainties in image‐based assessment of Radiation Therapy
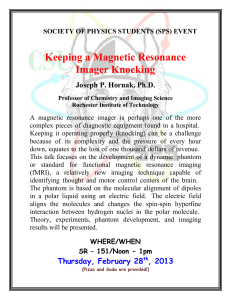
advertisement

Uncertainties in image‐based assessment of Radiation Therapy James Balter University of Michigan = ? Disclaimers • Advisor, Calypso Medical Technologies • Supported by NIH P01CA59827 Confession • I may have nothing new (or useful) to say Depression • I will still spend ~40 minutes searching for something useful to tell you! Objective • Therapy assessment is a critical element of: – Individual patient treatment outcome evaluation – Clinical trial design – Population‐based retrospective evaluation of treatment results • It is also a potential driving force in individualizing treatment mid‐course Objective • The imaging methods used, display and analysis techniques employed, standards (or lack thereof), and fundamental human variations all contribute to uncertainties in image‐based assessment • This talk will explore some image‐based assessment methods, explore a few evolving paradigms and techniques, and needs for quality control and validation of imaging for therapy assessment Longitudinal assessment Image Treat Image Tumor size • Some solid tumors visibly change size as therapy progresses • Size change is often correlated with response New Drug Kills Cancer with Few Side Effects The incredible shrinking tumor These CT scan images– showing the cross section of the patient’s abdomen–depict how her ovarian tumor (denoted by the red circle) shrunk in response to a new anticancer drug called olaparib. The patient carries a mutation in the BRCA1 gene, impairing her tumor cells’ ability to repair DNA damage. Olaparib delivers another blow to the cancer cells’ DNA repair machinery, killing them outright. Credit: The New England Journal of Medicine Response Evaluation Criteria in Solid Tumors (RECIST) • RECIST (Response Evaluation Criteria In Solid Tumors) is a set of published rules that define when cancer patients improve ("respond"), stay the same ("stable") or worsen ("progression") during treatments. • The original criteria were published in February 2000 by an international collaboration including the European Organization for Research and Treatment of Cancer (EORTC), National Cancer Institute (NCI) of the United States and the National Cancer Institute of Canada Clinical Trials Group. • RECIST 1.1, published in January 2009, is an update to the original criteria. Today, the majority of clinical trials evaluating cancer treatments for objective response in solid tumors are using RECIST. • Source: www.recist.com RECIST 1.1 attempts to enforce consistency • Cancer trials are increasingly complex, involving dozens or even hundreds of investigators from centers around the world. While the RECIST rules are highly dependent upon measurement of tumor size, different clinicians may vary greatly in their methods of performing these measurements. • Consistency in following the imaging requirements and rules is even more challenging. When investigators vary in how they follow RECIST as a trial endpoint, the study results may be placed in jeopardy by significant levels of variability. Source: recist.com Some key elements of RECIST Target lesion selection Measurement rules Consistency of repeat scans Guidelines for use of PET, and non‐axial images (e.g. MRI) • Definitions of: • • • • – PD (progressive disease) – 20% increase – CR (complete response) – disappearance of target lesion(s) – PR (partial response) – 30% decrease Cone beam CT images of a patient with oropharyngeal cancer at the first (left) and 35th (right) fraction of treatment. RECIST 1.1 specifies measurement of the largest single dimension of the tumor as an indication of response. RECIST – Need for consistent imaging modality and acquisition protocols Source: recist.com “RECIST is simple. Using RECIST is not.” Source: recist.com CT imaging – the gold standard? • Radiation Oncology places significant faith on the accuracy of CT imaging for: – Patient Geometry – Electron Density assignment • How accurate is modern CT? Current and Future Clinical Applications of Quantitative CT John M. Boone Departments of Radiology and Biomedical Engineering University of California, Davis 0.04 spr 0.03 0.02 0.01 0.00 John M. Boone position No detected scatter: p (t ) t Io ln eff t I o e With detected scatter: Io Io p (t ) t ' ln eff t I o I o e Scatter to primary ratio (SPR) = John M. Boone Water reference SPR = 5%, measurement SPR different 1% 2% 3% 4% 5% John M. Boone Water reference SPR = measurement SPR soft tissue John M. Boone 1% 2% 3% 4% 5% Different vendors have different HU values John M. Boone CT still gives accurate volume definition, right? • More on this later…. Molecular Imaging • (FDG) PET is commonly used to visualize tumor extent (metabolic surrogate) • FDG and other agents have been considered as tools to aid in “dose painting” – Metabolism surrogate: FDG – Hypoxia surrogates: FDG, FAZA, F‐Miso, Cu‐ATSM – Proliferation surrogate: FLT – Liver Metabolism (HIDA) –… I am not (yet) a dose artist… FLT (proliferation) image Courtesy of R Jeraj, UW) Balter BWH 2010 70 Gy 60 Gy 50 Gy FDG PET changes in RT of NSCLC 16 14 FDG PET 12 M e ta b o lic n o n -re s p o n d e rs SUV max 10 A v e ra g e 8 6 M e ta b o lic re s p o n d e rs 4 2 0 0 10 RT 20 30 40 50 60 70 T im e [d a y s ] Baardwijk et al 2007, Radiother Oncol, 82: 145. Courtesy of Robert Jeraj, UW Sensitivity and specificity issues for metabolic imaging • Consistency of images – Scanner calibration – Injected activity – Scan time – Reconstruction options • Patient variations – Baseline metabolism – Non‐related tissue uptake (e.g. inflammation) R Boellard, JNM 50 (5 Suppl), 2009 • Review of factors influencing quantitative PET • Included technical, biological and physical factors Peter Scully et al (Wisconsin): Optimizing PET imaging protocol parameters Reconstruction Parameters Recon Acquisition Grid Size Algorithm Iterations Post filter A 2D 128 x 128 2D OSEM 2 3 mm B 2D 128 x 128 2D OSEM 2 5 mm C 2D 128 x 128 2D OSEM 4 5 mm D 2D 256 x 256 2D OSEM 2 3 mm E 2D 256 x 256 2D OSEM 2 5 mm F 3D 128 x 128 3D OSEM 2 3 mm G 3D 128 x 128 3D OSEM 2 6 mm H 3D 128 x 128 3D OSEM 4 6 mm I 3D 256 x 256 3D OSEM 2 3 mm J 3D 256 x 256 3D OSEM 2 6 mm Scully et al – optimize parameters based on recovery of volumes of known object size and activity Scully et al Recovery Coefficient 1.2 1.0 0.8 0.6 0.4 A B C D E F G H Reconstruction I J PET signal versus tumor response for chemotherapy. A tumor that is not responding sufficiently to treatment after 2 cycles of chemotherapy (blue dashed line) may be predictable from PET changes, whereas one that would respond after 4 cycles (red) may be indistinguishable from one that may require more aggressive treatment (black) as signals below the PET detection threshold still may involve several logs of viable cells. (adapted from Kasamon YL, Jones RJ, Wahl RL. J Nucl Med. 48 Suppl 1:19S-27S, 2007) – R. Wahl, JHU Physiological imaging • Imaging as a surrogate for physiological endpoints – Ventilation: SPECT, polarized gas MRI, 4D CT – Perfusion: MAA SPECT, Dynamic contrast enhancement (MRI, CT) – Diffusion (as a surrogate for tumor cellularity, integrity of nerves): Diffusion weighted imaging –… Mayr et al IJROBP 77(2), 502‐8, 2010 Perfusion • Many different methods of acquiring and analyzing data • Multiple metrics: total perfusion, “area under curve”, initial slope, mean transit time, transfer coefficients, local blood volume,… Dynamic Contrast Enhanced (DCE) imaging for perfusion analysis • Inject contrast • Acquire a cine series of image volumes • Analyze within regions or voxels: – Reference input (arterial, venous) signals – Test tissue signals • Derive parameters from model fit to these signals Mayr et al IJROBP 77(2), 502‐8, 2010 Examples of perfusion related models • Brain perfusion model (Ostergaard MRM 1999) – Brain perfusion • Kety model (Toft JMRI 1999) – Transfer constant to tissue and blood volume • Dual‐input and single compartment liver perfusion model – Arterial and portal venous perfusion Cao AAPM2009 t R2*tiss (t ) R2* AIF ( ) R (t ) d 0 Ct (t ) K trans t 0 e k ep ( t ) C p ( )d v p C p (t ) t 1 Cl (t ) [k a Ca ( a ) 0 (1 Hct ) k p C p ( p )]e k 2 ( t ) d Choose acquisition sequence, parameters and models • What is targeted in the • choose right acquisition, clinical trial parameters and model – Anti‐VEGF therapy in recurrent GBM – Ktrans and blood volume • Toft (Kety) and CBV models Sorensen et al, Cancer Research 2009 Cao AAPM2009 Choose acquisition sequence, parameters and models • What is targeted in the • choose right acquisition, clinical trial parameters and model – Chemo + RT In HN Cancer Local control – Blood volume and flow • Toft and blood flow models Local failure 17mL/100g Pre RT Cao AAPM2009 BV after 2 weeks RT Cao, et al Red Journal 2008 Choose acquisition sequence, parameters and models • What is targeted in the • choose right acquisition, clinical trial parameters and model – Radiation effect on liver – Portal venous perfusion function • Dual‐input, single compartment liver perfusion model Cao AAPM2009 Motion needs to be considered Before registration Cao AAPM2009 After registration Perfusion CT involves potentially significant dose (even by RT standards) 30 – 50 CT scans at the same location perfusion A. perfusion imaging John M. Boone time to peak enhancement blood volume B. computed parametric images Safety of new imaging protocols Some organized efforts for standardizing quantitative imaging • Quantitative Imaging Network • Quantitative Imaging Biomarker Alliance (QIBA) The Quantitative Imaging Network (QIN) • PAR‐11‐150; a U01 mechanism issued originally in August 2008, and reissued in March 2011. – No set‐aside funds and no limit to the number of awards • Submission dates: – February 5, June 5, and October 5 – Electronic submissions through grants.gov • Reviewed by Special Emphasis Panel (SEP) from NCI The QIN Program • Our hypothesis: Optimized and validated quantitative imaging techniques are needed on commercial platforms for large scale multi‐center clinical trials focused on therapy response. • Therefore: Necessary to promote innovative research in this area. • Goal: Bring quantitative imaging as a validated method or tool to oncologists to support clinical decision making. R Nordstrom, NIH Current QIN Status • Currently, 9 network members – Two more teams in position to be funded – Several face‐to‐face meetings • Broad range of imaging modalities – CT and PET/CT – SPECT – MRI, DCE‐MRI, DW‐MRI • Phantom studies, quality assurance • Longitudinal studies • Database development and sharing R Nordstrom, NIH The Present Members of QIN Univ. of Washington Brigham & Women’s Hospital Columbia Univ. Mass. General Hospital Stanford Univ. Univ. of Iowa Univ. of Pittsburgh Vanderbilt Univ. H. Lee Moffitt R Nordstrom, NIH QIN working groups • Data Collection (Barbara Croft) • Image Analysis and Performance Metrics (Huiming Zhang and Keyvan Farahani) • Bioinformatics/IT and Data Sharing (Larry Clarke) • Outreach: External/Industrial Relations (Pushpa Tandon) • Clinical Trial Design and Development (Barbara Galen) QIBA • Mission: Improve the value and practicality of quantitative biomarkers by reducing variability across devices, patients, and time • Current committees: – DCE MRI – fMRI – FDG‐PET – Volumetric CT – COPD‐Asthma How do we know that everything works? • Accuracy – How close you are to the truth • Precision – How reproducible your measurement is In vivo evaluation – test retest • Perform imaging through analysis on the same subject without therapeutic intervention • Reasonably incorporates multiple sources of uncertainty Frings et al JNM 51(12), 2010 Phantom development • The need for quantitative imaging phantoms is well established • The design and propagation of useful phantoms is not Volume characterization phantom (CT‐QIBA) (b) (a) • The FDA has a research lab (N Petrick) developing image volume assessment phantoms N Petrick, FDA Spherical Ellipsoid Lobulated Spiculated (c) FDA ‐ Phantom images Current: 2 fixed densities (‐630, +100 HU) N Petrick, FDA Future: mixed density N Petrick, FDA One example analysis – slice thickness effect on ellipse volume measurement N Petrick, FDA Perfusion phantom 1 – QIBA (Jackson et al) • Designed for support of DCE MRI studies • Inserts of known T1 in a static phantom Perfusion phantom 2 – PMH (Driscoll et al) A) Perfusion Pump (A) B) Injection Pump (B) C) Flow Phantom (D) D) Flow control valves (E) (C) Driscoll, Coolens, Keller et al. E) Combined Flow PMH phantom Tested the range of the phantom with two different input flow rates and different contrast injection boluses Driscoll, Coolens, Keller et al. Perfusion Phantom 3 –UM (Thomas et al) Vascular branching network Compartments to yield differential sub‐voxel perdusion Synthetic data • Good for algorithm and software testing/validation • Removes imaging experiment bias • QIBA has synthetic DCE data as a project under the DCE‐MRI group (Barboriak – Duke) ‐ https://dblab.duhs.duke.edu/wysiwyg/downl oads/README_dcemri_testdata.txt Synthetic Data – Cao (UM) • Simulated DCE phantom for testing the standard DCE model (general Toft model) Parameters considered: CNR, temporal resolution, dynamic acquisition time, Ktrans, • • Vp, kep, input function temporal jitter, … >1 million simulations to cover a large range of variations of parameters 2500 simulations for each combination of the parameters • 12 Relative SD% of Vp K=0.01, vp=0.01,kep=0.07 K=0.05, vp=0.2, kep=0.3 K=0.1 , vp=0.05, kep=0.7 K=0.5, vp=0.1, kep=3.3 K=0.001,vp=0.01,kep=0.007 15 Relative SD% of K trans 20 10 5 K=0.01, vp=0.01,kep=0.07 K=0.05, vp=0.2, kep=0.3 K=0.1 , vp=0.05, kep=0.7 K=0.5, vp=0.1, kep=3.3 K=0.001, vp=0.01, kep=0.007 8 4 0 0 0 0 20 40 60 CNR Cao AAPM2009 80 20 40 60 80 100 CNR e.g. Ktrans and Vp do not have same sensitivity to noise! 100 What do we need? • Data acquisition standards – Imaging systems and acquisition/reconstruction methods that are designed to be reproducible • Design of systems • Standard use protocols • Incorporation of acquisition (and analysis) parameters within the framework of the image data What do we need? • Methods and procedures for maintaining and evaluating quantitative imaging systems – Phantoms – standard data for testing analysis methods – common algorithms/language of analysis What do we need? • Education – Most current quantitative imaging issues do not yet impact actual treatment planning in typical clinics yet – their emergence (as well as our growing dependence on PET, automated image segmentation, and deformable registration) hints at educational and infrastructure needs to support practice changes in our near future Summary • Image‐based therapy assessment is heavily used in clinical trials, and is emerging in routine radiotherapy • Imaging systems and their use need careful characterization, validation, and QA to support quantitative use • As Radiation Oncology departments are routinely using advanced imaging, image‐based quantitative evaluation is emerging as a growing educational and support need for medical physicists RECIST 1.1 – consistent contrast use