AN ABSTRACT OF THE THESIS OF
advertisement

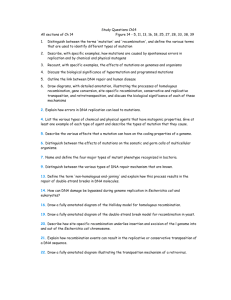
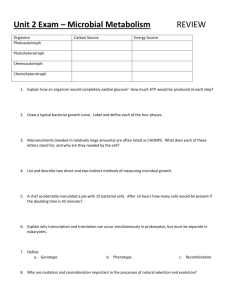
AN ABSTRACT OF THE THESIS OF Oi Wang for the degree of Master of Science in Toxicology presented on March iQ 2005. Title: Hypermutagenic Induction of Mitotic Recombination by Ionizing Radiation in Mihi Null Mouse Cells Abstract approved: Redacted for privacy Mitchell S. Turker Mitotic recombination is a common autosomal mutation in mammalian cells involving crossover events between homologous chromosomes. This process can convert a cell with a heterozygous deficiency to one with a homozygous deficiency, and thus often represents the second step in tumor suppressor gene inactivation. In this study I examined the frequency and spectrum of ionizing radiation (IR)-induced autosomal mutations affecting Aprt activity in a mouse kidney cell line null for the Mihi mismatch repair (MMR) gene. The mutant frequency results demonstrated a hypermutable response to JR and the spectral analysis revealed that most of this response was due to the induction of mitotic recombinational events. High frequency induction of mitotic recombination was not observed in a DNA repair-proficient cell line or a cell line with an MMRindependent mutator type. I also provide evidence that JR exposure did not induce significant numbers of base-substitution in the Mihi null cells. These results demonstrate that IR exposure can initiate a process leading to mitotic recombinational events and that MMR function suppresses these events. My results suggest a caveat for use of IR to treat MMR deficient tumors because the combination of high levels of induced mitotic recombinational events and preexisting intragenic mutations might increase malignant potential in surviving cells. Hypermutagenic Induction of Mitotic Recombination by Ionizing Radiation in MI/il Null Mouse Cells by Qi Wang A THESIS submitted to Oregon State University in partial fulfillment of the requirements for the degree of Master of Science Presented March 10, 2005 Commencement June 2005 Master of Science thesis of Qi Wang Presented on March 10. 2005 APPROVED: Redacted for privacy Major Professor, representing Toxicology Redacted for privacy Head of the Department of Environmen1 and olecu1ar Toxicology Redacted for privacy Dean olthe Gra)LJchoo1 I understand that my thesis will become part of the permanent collection of Oregon State University libraries. My signature below authorizes release of my thesis to any reader upon request. Redacted for privacy Qi Wang, Author ACKNOWLEDGMENTS The author expresses sincere appreciation for the enthusiastic supervision of Prof. Mitchell Turker during this work. Without him, this thesis would not have been possible. I thank him for his patience and encouragement that carried me on through difficult times, and for his insights and suggestions that helped to shape my research and life career goals. His valuable feedback contributed greatly to this thesis. I thank Prof. Andrew Buermeyer for his help and support during my initial stages of my study when I first came US. I am thankful to my committee members: Prof John Hays, Prof. Andrew Buermeyer, Prof. David Williams and Prof. Jeffrey Stone for their wise counsel and support. I would like to acknowledge the help of Dr. Phillip Yates for his support. Olga Ponomareva and Michaele Lasarev are greatly thanked for sharing ionizing radiation mutagenesis data of MMR proficient cells with me. I thank Lanelle Connolly, Amy Skinner, Renee Lewis, Sarah Godsey, Jon Oyer, Elizabeth Kasameyer and all the other former Turker lab members for their assistance with all types of technical problems at all times. I thank all the staff in Department of Environmental and Molecular Toxicology, and Center for Research on Occupational and Environmental Toxicology at Oregon Science and Health Unviersity. Without them, my study would not be that smooth and tolerable. Finally I would like to express my deep gratitude for the constant support, understanding and love that I received from my parents, my sister and my husband during the past years. I am supported by a training core from NIEHS 1P42 ES 10338. TABLE OF CONTENTS Page Introduction ................................................. Materials and Methods ..................................... Cell lines .................................................. 1 12 12 IR Cell survival assay ....................................12 Determination of mutant frequency and mutant isolation .................................... 13 Isolation of genomic DNA ........................... 14 Distinguishing between large and small Aprt mutations in mutant cells 15 LOH analysis for large mutational event ........................................... 16 DNA sequencing for small mutational event ................................... 22 Statistical analysis ....................................... 23 Results ......................................................... 24 Effect of Mihi status on cell survival to ionizing radiation ......................... 24 Mutagenic effect from IR on Mihi null cells ....................................... 25 TABLE OF CONTENTS (CONTINUED) Page The hypermutagenic response in the Mihi null cells is due to the induction of mitotic recombinational event........................ 30 Discussion ...................................................... 38 Conclusion ...................................................... 44 Bibliography ..................................................... 45 LIST OF FIGURES Figure Pg 1. Large and small mutational events can be determined by amplifying Aprt gene ........................ 16 2. Large mutational event can be characterized by LOH patterns of microsatellite markers along chromosome 8 ........................................... 18 3. Retention of heterozyogsity or loss of heterozygosity for microsatellite markers 56 and 190 shown in LOH analysis .............................. 21 4. Primers used to amplify and sequence mouse Aprt gene ................................................ 22 5. Cell survival to ionizing radiation ............................. 25 6. Mutant frequencies for JR-exposed and unexposed subclones for three kidney celllines ........................................................... 28 7. The frequencies of mutational events with or without JR-exposure .......................................... 34 LIST OF TABLES Table Page 1. Mutant frequency for IR-exposed and unexposed kidney cell line subclones ....................... 26 2. Spectrum of mutations for IR-exposed and unexposed cells .......................................... 32 3. Frequency of each mutational event ....................... 33 4. Examples of alleles with mutations ........................ 36 5. Mutation distribution at the Aprt Locus of unexposed and IR-exposed K634 .......................... 37 Hypermutagenic Induction of Mitotic Recombination by Ionizing Radiation in Mihi Null Mouse Cells Introduction Different factors contribute to mutagenesis and carcinogenesis in living organisms. These factors may come from endogenous or exogenous sources. Exogenous sources include ultraviolet radiation, ionizing radiation, or various environmental chemicals such as alkylating agents. Endogenous sources such as reactive oxygen species are produced inside the cell. Mutations can also arise as a result of DNA polymerase error. The error rate of replicative polymerases is approximately io. The 3' to 5' exonuclease activity of DNA polymerase reduces this rate to approximately 1 o. A well-studied pathway named mismatch repair (MMR) further decrease the rate to one in 1 O. Prokaryotic and eukaryotic cells have evolved this highly conserved mechanism to correct mismatches arising during replication. Although most studies of MMR functions have focused on postreplication fidelity, recent studies suggest that MMR proteins are also involved in other processes to maintain genomic integrity and to avoid mutations. These processes include DNA damage recognition and homologous recombination. These functions will be discussed below as drawn from comprehensive reviews [1] [2] [31 and original research reports. The steps in MMR are recognition and binding, nicking (in prokaryotes), excision of fragments, replication and ligation. In E. coli, MutS recognizes base- pair mismatches and 1-4 base pair insertion-deletion loops (IDL). MutS is an ATPase that funtions as a homodimer. Its N-terminus contains the DNA binding domain, and its C-terminus includes ATP binding/hydrolysis and dimerization sites. Both subunits in MutS homodimers are involved in ATP binding/hydrolysis and mismatch binding. MutS has counterparts in eukaryotic MMR systems. In yeast, the MutS homologs include MSH1, MSH2, MSH3 and MSH6, which function in MMR, and MSH4 and MSH5, which function in meiotic recombination rather than postreplication correction. MSH 1 is involved in mitotic mismatch repair in mitochondna. Instead of working as homodimers as in E. coli, MSH2, MSH3 and MSH6 recognize and bind mismatches as heterodimers. MSH2/MSH6 form MutSy and bind base-base mismatches and +1 IDL. MSH2/MSH3 form MutSy and bind +1 IDL and 2-8 nucleotide loops. MutS homologs in mammalian cells are similar to those in yeast. In the presence of ATP and a mismatch, MutS recruits MutL. MutL is also an ATPase and functions as a homodimer. The N-terminus of MutL belongs to the GHKL ATPase superfamily and its C-terminus may be used for dimerization and interaction between MutL and UvrD helicase. MutL coordinates functions of MutS, MutH, and UvrD. The latter two proteins will be discussed below. Eukaryotes also have MutL conterparts. In yeast, MutL homologs form heterodimers MLH1/PMS1, which is a major player in postreplication repair, and MLHI/MLH3 and MLH1/MLH2, which play minor roles. Mammalian MutL homologs form MLH1/PMS2 (MutLy), MLH1/PMS1 (MutLy) and MLH1/MLH3 heterodimers. Inactivating mutations in MutS and MutL homologs 'I can induce higher spontaneous mutation rates in cells. In humans, HNPCC (human nonpolyposis colon cancer) is caused by germline mutations in MMR genes Msh2 (50%), Mlhl( 40%) and Pms2 (10%) [4]. ATP hydrolysis releases MutS from a mismatch and triggers its movement along the DNA molecule in both directions, which can be up to 1KB in E. coli. In E. coli, MutL recruits and activates MutH, which is a monomeric endonuclease. To correct mismatches MMR must replace the incorrect base in the newly synthesized strand. Hemimethylated GATC sites help MMR to distinguish the newly synthesized strand from the template strand. MutH nicks the unmethylated strand at GATC sites and UvrD helicase then unwinds the nicked strand. SSB and helicase II also interact with MutL and are recruited to the nicked strand. RecJ, exoVil, exol, exoX excise past the mismatch and Polill is used to resynthesized the DNA strand. Ligase then seals the nick. In eukaryotes, Exol, RAD27 and DNA ploymerase y and y may provide the exonuclease functions. RPA fills the role of SSB in prokaryotes. In eukaryotes, there are no GATC hemimethylated sites that can be used to direct MMR to nick the newly synthesized strand. No counterpart of MutH has been identified and no nicking activity has been found to be associated with MMR in eukaryotes. It has been suggested that PCNA might help MMR distinguish the newly synthesized DNA strand in eukaryotes. Some studies have shown that MSH2 and MSH6 physically interact with PCNA and that PCNA help deliver MutS homologs to newly replicated strands. ru Recent studies have shown that in addition to recognizing mismatched bases, MMR may also recognize various base modifications caused by different genotoxins, such as 8-oxo-guanine lesions caused by oxidative stress and O6 methyl guanine caused by alkylating agents. By recognizing 8-oxo-guanine induced by oxidative stress, MMR might cooperate with base excision repair (BER) to repair 8-oxo-G:A mismatches. In Msh2-I- mouse embryonic fibroblasts, H202-induced 8-oxo-guanine was increased relative to MMR proficient cells [5]. MutSy is attracted by 8-oxo-G and binds preferentially to 8-oxo-G:A when compared with 8-oxo-G:C [6]. Studies have suggested that MMR helps remove 8oxo-G opposite to A and that hMSH6 may work with hMYH to remove A opposite 8-oxo-G [7]. In budding yeast, MSH2/MSH6 work with OGG1 to remove A misincorporated opposite to 8-oxo-G, thus preventing G:C to T:A transversions [8]. MMR also plays a role in suppressing mutations caused by alkylating agents. Alkylating agents, like 1-Methyl-1-nitrosourea (MNU) and 1-methyl-3-nitro-1nitrosoguanidine (MNNG), can form 06-methylguanine, 04-methylthymine and N-methyl bases. N-methyl bases are mainly repaired by BER. 0-methyl-modified bases are repaired by methylguanine methyltransferase (MGMT). When damage caused by alkylating chemicals exceeds the repair capability of MGMT, cells will undergo cell cycle arrest often followed by apoptosis. However, MMR deficient cell lines do not undergo cell cycle arrest alter exposure to alkylating agents and are resistant to cytotoxicity, suggesting a role for MMR in this process [9]. Two models have been proposed to explain these observations, the futile repair model and the signaling model. The futile repair model proposes that MMR proteins bind O6metGIT or O6metGIC during replication, remove the T or C base and then add another C or T back again. This process does not remove O6metG because O6metG is in the template strand. According to this model, multiple cycles of excision/resynthesis will eventually arrest the replication fork [9]. The signaling model proposes that it is not the arrest of the replication fork that finally leads to cell cycle arrest and apoptosis, but instead it is the activation of the ATM/ATR pathway that leads to arrest and apoptosis 1101. In this model, futile repair of O6metG leads to many double strand breaks activating the ATM/ATR pathways, which lead to cell cycle arrest and apoptosis [11]. By discussing MMR proteins involvement in avoidance of mutations caused by oxidative stress and alkylating agents, I have suggested that MMR proteins function in these two cases is recognition of modified bases that can form mismatches during replication. This leads to the suggestion that MMR proteins interact with other DNA repair pathways to eliminate modified bases or to arrest cells that will undergo apoptosis if lesions can't be repaired properly. In addition to the functions discussed above, MMR is also involved in genetic recombination. MMR may affect genetic recombination through two pathways, one is through its ability to recognize mismatched bases and the other is independent of error correction. Genetic recombination, more specifically homologous recombination, can occur in somatic cells (mitotic recombination or sister chromatid exchange), or in germ cells (meiotic recombination). MMR proteins MSH4 and MSH5 affect meiotic recombination in a way that is believed to be independent of error correction of mismatch repair. The influence of other MMR proteins such as MSH2 and MLH1 on both mitotic and meiotic recombination may stem from their function in repairing mismatches in heteroduplexes arising during recombination, and suppression of recombination between divergent sequences. MSH4 and MSH5 form a heterodimer. They don't appear to function in MMR because the mutations don't confer microsatellite instability, which is a marker for genomic instability caused by MMR deficiency. Moreover, their mRNA expression is low in tissues other than testis and ovary. Yeast Msh4 and Msh5 mutants showed wild type levels of gene conversion and postmeiotic segregation, however they exhibit reduced crossing over rates in meiosis 11121. Loss of Msh4 or Msh5 in mice leads to failure of normal meiotic pairing and synapsis. Studies indicate that MSH4/MSH5 emerge on the intermediate meiosis nodule in zygonema of prophase I, then decline in late pachynema or early diplonema. Further studies are needed to clarify their specific function in meiosis 11131. MMR proteins function in repairing mismatches in heteroduplexes during genetic recombination may be similar to its function in postreplication repair. This process also includes recognizing and binding to the mismatches. Heteroduplexes can arise in four ways: 1) when the invading strand pairs with a complimentary donor strand, 2) when the displaced strand in the donor sequence pairs with the 7 single strand on the other side of DSB (double strand break), 3) through branch migration in the Holliday junctions and 4) when the invading strand anneals back to its original DNA strand [141 . In yeast tetrad analysis studies of meiotic recombination, MMR deficiency results in an increase of postmeiotic segregation and a decrease of gene conversion, which suggests a failure to repair the mismatches that arise in the heteroduplex [15]. MMR proteins also suppress homologous recombination between divergent sequences. Mitotic recombination between similar sequences might lead to lethal chromosome translocations or the conversion of heterozygous mutations to homozygous mutations. In a recent review, the authors suggest that homologous recombination between imperfect matches sequences can be suppressed via three mechanisms: 1) by slowing strand exchange rates, 2) by blocking strand exchange, and 3) by increasing the instability of the blocked heteroduplex intermediate [14]. MMR proteins such as MutS and MutL homologs are found to promote the latter two mechanisms. In prokaryotes, transformation, transduction and conjugation all require HR to successfully transfer the introduced DNA sequence. MMR proteins were shown to inhibit these processes because the inactivation of MMR proteins increases the frequency of sequence transfer [161 [171. In yeast, MMR was also shown to block branch extension in homologous recombination in the presence of mismatches, and thus prevent HR between divergent sequences [14]. In E co/i and yeast, there is evidence implying that helicases RecQ and SGS1 and MMR repress homologous recombination between divergent sequences by unwinding 8 the invading strand [181. In mammalian cells, BLM, a RecQ family member, colocalized with MSH6 in discrete nuclear foci after ionizing radiation [191. BLM also have been reported to interact with MLH1 [20]. MMR proteins may also directly interact with signaling pathways such as the physical interaction between ATM and MSH2 after ionizing radiation exposure [21]. My thesis research is focused on how MMR affects ionizing radiation mutagenesis. Ionizing radiation is a mutagen that induces a variety of DNA lesions including DSBs, single strand breaks and base and sugar modifications. If these lesions are not repaired correctly a variety of mutations can be induced that can be characterized as large or small event mutations. Small event mutations include base substitutions, small deletions, insertions and frameshifts. In a paper studying JR-induced mutations in the APRT (adenine phosphoribosyltransferase) gene in CHO cells, base substitutions were induced with no hot spots discovered for these mutations. Unlike most mammalian cells, loss of APRTin CHO cells can't occur readily via a large mutational event because it links to some critical genes [22]. Most ionizing radiation induced mutations are large in size [23]. In studies using human lymphoblasts and mouse embryonal carcinoma cell lines, large events account for most ionizing radiation induced mutations [241 [25]. Large events include chromosome loss, deletion and mitotic recombination. Studies in human TK6 lymphoblasts using TK (thymidine kinase) or HPRT (hypoxanthine phosphoribosyltransferase) genes as selectable markers showed that most X ray- induce mutations arise from deletions [26] [27]. However at least one study has suggested that mitotic recombination may also contribute to mutagenesis induced by ionizing radiation (IR) [28]. DNA repair proteins may interact with ionizing radiation to activate cell responses. This could affect JR-induced mutagenesis, as shown in a study in which p53 null mice showed increased deletion and mitotic recombination compared to p53 proficient mice after JR-exposure. The authors suggested that this may be due to p53 protein involvement in homologous recombination and nonhomologous end joining [29]. There are also studies about potential MMR involvement in the cellular response to IR-exposure. In research using transgenic mice with transgenic supFGl and lambda cli reporter genes, Pms2 deficiency was shown to increase the frequency of IR-induced mutations when compared with Pms2 proficient mice. This study suggested that MMR proteins' deficiency conferred hypermutability to JR-exposure and the mutations are caused by unrepaired oxidative lesions [30]. Various studies have investigated the role of MMR in IR-activated responses. An early study showed that Mi/il deficient human colon carcinoma cells (HCT 116) and murine Mi/il knockout cells had transient G2-M cell cycle arrest or inability to maintain the G2-M arrest after IR-exposure [311. They also showed that Msh2 deficient cell lines show a similarly altered G2-M checkpoint. These studies have suggested that this altered G2-M checkpoint may be due to a defective maintenance of phospho-Tyr-cdc2 level in MMR deficient cells [32]. A 10 separate study also reported that Msh2 deficient cell lines showed an inefficient G2/M checkpoint, that CHK1 activation was transient and that CHK2 was not phosphorylated [33]. A recent study suggested that S-phase checkpoint activation in response to JR also required MMR proteins, because Mlii] null cells showed RDS (radioresistant DNA synthesis) after JR-exposure. In this study the authors also showed that MSH2 binds to CHK2 and MLH1 binds to ATM, which suggested that MMR affected the S-phase checkpoint by interacting with ATM pathway [21]. A second study, however challenged these findings by showing normal S-phase checkpoints in three Mihi null cell lines. They suggested that signaling defect to JR exposure may be due to the experiment procedures and phenotypic traits of the cells the other authors used [34]. The reply to this challenge was that the different results from the studies may be due to mutations other than MMR deficiency in the MMR deficient cells used by the different groups [341. The primary damage JR causes is DSB (double strand break). DSB can be repaired through homologous recombination and nonhomologous end joining. In earlier paragraphs, I have introduced that MMR proteins can inhibit HR (homologous recombination) between divergent sequence. It is rational, therefore, to infer that in addition to the possibility that MMR exerts its influence by interacting with signaling pathways, MMR may also affect the response to JR by influencing correction of DSBs by homologous recombination repair. A study using mouse embryonic fibroblasts showed that there was defect in localization of 11 recombination-related proteins MRE1 1 and RAD5 1 and increased chromosomal damage in Msh2 deficient cells after IR-exposure [331. My graduate thesis research continues the study of the role of MMR in the response to JR-exposure. In contrast to other studies focused on cell cycle signaling pathway affected by MMR in IR-exposed cells, my work is focused on IR mutagenesis in an MMR deficient cell line. Through analyzing mutant frequencies and mutational spectra in an JR-exposed MMR deficient cell line and in MMR proficient cell lines, I investigated how IR-induced mutagenesis is changed in MMR deficient cells. 12 Materials and Methods Cell lines: The three cell lines used for my thesis are Mihi null K634, K06 and K435. K634 is a kidney epithelial cell line from mice null for Mihi. K06 and K435 are kidney epithelial cell lines derived from wild type mice. All three cell lines are heterozygous for Aprt: in these three cell lines, one copy of Aprt gene is intact and the other copy is disrupted by an insertion of a DNA sequence that confers neomycin resistance to the cells. All three cell lines are heterozygous for some microstallite markers along chromosome 8, which harbors Aprt gene. K435 shows a MMR-independent G: C to C:G transversion mutator phenotype [351. K06 exhibits a spontaneous mutational spectrum similar to diploid kidney cells in vivo [35]. All these three cell lines were maintained in the Dulbecco's Modified Eagle's Medium (DMEM, Gibco BRL) supplemented with heat-inactivated 10% (vlv) fetal bovine serum in 5% CO2, at 37 °C. JR Cell survival assay: Cells were grown in T75 flasks, then collected and put into 15 ml conical tubes at 106 cells per tube. After exposure to '37Cs-? at various doses (0 Gy, 1 Gy, 2 Gy, 4 Gy, 5 Gy, 6 Gy and 8 Gy ), the cells were plated at various densities: 200 and 400 cells per plate at 0 Gy and 1 Gy, 400 and 800 cells per plate at 2 Gy, 600 and 1200 cells per plate at 4 Gy and 5 Gy. 600 and 2000 cells per plate at 6 Gy and 13 1000 and 2500 cells per plate at 8 Gy. After 2 weeks, the plates were stained with 0.25% crystal violet and the number of surviving clones determined. Determination of mutant frequency and mutant isolation: Cells were plated at 400 cells per plate and clones allowed to form for 2 weeks. Subclones were picked and grown to confluent T75 flasks. For each subclone, 106 cells were counted, put into 15 ml conical tube and then exposed to 6 Gy of 137Cs- y radiation. Cells were then put back into T75 flasks and allowed to recover for 1 week. Untreated cells used for spontaneous mutagenesis analysis for each subclone were collected and underwent the same procedure except for irradiation. Both exposed and unexposed cells for each subclone were plated at 400 and 200 cells per plate to decide cloning efficiency for non-selected condition. Plates of 5 X iOn, 10 X iO, 15 X iO cells were set up at the same time and 2,6- diaminopurine (DAP) was added at a concentration of 80 ug/mI the next day. These plates were used to select Aprt deficient mutants and to determine the mutant frequencies. After 2 weeks, the non-selected plates were stained with 0.25% crystal violet. After an additional 7-10 days, the DAP selection plates were also stained with 0.25% crystal violet. DAP resistant clones were isolated from some selection plates and expanded for a molecular analysis. Stained plates were scored for colonies. Cloning efficiency was calculated by the ratio of number of colonies counted to the number of cells plated. Mutant 14 frequency is the ratio of the cloning efficiency in DAP selected plates to that in the non-selected plates. Isolation of genomic DNA: Aprt deficient mutant clones were expanded to confluent T25 flasks. After rinsing with PBS, lOpl of 10pM proteinase K, 4Opl of 100 pm sodium lauryl sulfate (SDS) and 500 pl of NLB solution (1 mM Tris, pH 8.0, 2.23 mM EDTA, 0.4 M NaCI) were added to each flasks. The flasks were incubated at 37°C overnight and the lysates transferred to microcentrifuge tubes. Saturated NaCl 170 p1 was added, followed by vigorous shaking for 15 seconds. After centrifugation, the supernatants were transferred to new tubes and two volumes 100% ethanol were added. DNA was precipitated and after another centrifugation the DNA pellet was washed with 70% ethanol. TE 200 pl was added to the tube and incubated overnight at 37°C to dissolve DNA. The next day, the solution was transferred to another tube, and 20 p1 7.5 M ammonium acetate and two volumes of ethanol were added to precipitate DNA. After being washed with 70% ethanol, the DNA pellet was dissolved and stored in 60 p1 TE. 15 Distinguishing between large and small Aprt mutations in mutant cells: When investigating the mutagenic effect of ionizing radiation, the mutational spectrum also needs to be analyzed. To analyze the mutational spectrum, I first distinguished between large and small event mutations for each mutant clone. In later steps, the large event mutations were further analyzed through LOH analysis and small event mutations were examined by DNA sequencing. Parental cell lines had one copy of Aprt that was made nonfunctional by an insertion of neomycin resistance sequence. Therefore for loss of Aprt function in the mutant cells, the other functional copy of Aprt must have been inactivated by a small event or large event mutation. The two types of events can be distinguished through detection of Aprt by PCR. Large events would lead to loss of the whole functional copy of Aprt gene, whereas small events would retain this copy. Three PCR primers were used: APRT-GA (GTAAACCTGACCCAATGTCTC), APRT-GS (AGCAAAGACCTAGTGTTCCTAGCAAG) and NEO-GS (GATCAGGATGATCTGGAGGAA). APRT-GA and APRT-GS were used to amplify exon 3 of the wild type copy of Aprt. APRT-GA and NEO-GS were used to amplify part of the neomycin resistant sequence and part of exon 3 of the knockout copy of Aprt. 16 PCR conditions were as followed: first denature at 94°C for 3 minutes, followed by 30 cycles denature at 94°C for 30 seconds, annealing at 58°C for 30 seconds, DNA extentesion by Taq polymerase (Invitrogen) at 72°C for 30 seconds, and alter the final cycle, reaction left at 72°C for 3 minutes. The PCR products were then separated in 1% agarose (Gibco BRL) For the small event mutation, two bands (344 bps for wild type copy and 600 bps for the knockout copy) would be expected. For large event mutation, the 344 bp band was lost, with 600 bp band left, as Figure 1 shows. LA)U LOU LOU MlOhp Knockout Aprt allele Wild type .1prI allele 44Obp ZOObp Small event mutation Large event mutation Figure 1: Large and sinai! mutational events can be determined by amplifying Aprt gene. Details were given in Materials and Methods. Knockout band of Aprt gene is aproximately 600 bps, and wild type band is 344 bps. Small event mutations would retain both bands, and large event retains the 600 bps knockout band only. LOH analysis for large mutational event: After distinguishing between large and small event mutants, we further characterized large event mutations by loss of heterozygosity (LOH) analysis. 17 Genetic polymorphism occurs when there are more than two variant alleles for a single locus in the genome. Loss of heterozygosity at a polymorphic locus in the genome is important in carcinogenesis. There are three types of large event mutations that can lead to LOH: deletion, chromosome loss and mitotic recombination. Distribution of L011 among polymorphic loci along one chromosome can be used to characterize these three types of large event mutations, as Figure 2 shows. A useful polymorphism for mouse genetics is the dCA repeat microsatellite, which is scattered throughout the mouse genome, and for which there are many strain specific polymorphisms. These polymorphic microsatellite loci were used as markers to determine the distribution of LOH in the Aprt mutant cells. 18 P . I intragenic recombination event I deletion Chromosome loss ikterozgous mkrosateilite Joel Figure 2: Large mutational event can be characterized by LOH patterns of inicrosatellite markers along chromosome 8. LOH patterns for polymorphic chromosome loci representing intragenic events, chromosome loss, mitotic recombination, and deletions. The mouse Aprt gene is located on chromosome 8. For the K634 cell line (Mihi null) I used 11 polymorphic microsatellite markers along chromosome 8 (from centromere to the telomere, marker 124, 3, 125, 190, 100, 312, 166, aprt, 13, 93, 56) In this study, through investigation of LOH for these 11 polymorphic microsatellite markers, I could detect distribution of LOH along chromosome 8, and then distinguish deletion, chromosome loss and mitotic recombination, as Figure 2 shows. First I amplified the polymorphic microsatellite dCA repeat regions for each locus along chromosome 8. All primers used were obtained from Research Genetics (Huntsville, AL) except for primers for CA-APRT microsatellite marker. 19 This primer pair are T[TCATAACGGAGCITCCCTTFAGT (CA3) and GGACCTTCCTGTGAGCCCGTG (CA4). PCR conditions for these markers are the following. First denature at 94°C for 5 minutes, followed by 30 cycles denature 94°C for 40 seconds and annealing and extension (Taq polymerase) both at the same step at 55°C for 30 seconds. After the final cycle the reactions left were left at 72°C for another 10 minutes. After denaturing the PCR products at 95°C for 5 minutes, we separated PCR products on 8% polyacrylamide gel at 80 watts. After overnight transfer of DNA product from gel to Hybond N+ membrane (Amersham), I did a southern hybridization, using DIG (digoxigenin) labeled probe. The oligonucleotide(CA)15 probe was labeled by DIG through the following protocol: Mix 8 /41 5X reaction buffer (made up by the manufacturer in the kit), 8 /41 25uM CoC12, 2 jil terminal transferase (all these three reagents are from ROCHE), 2 jil DIG (digoxigenin)-1 1-dUTP (ROCHE), 4 jil 50 jiM Oligonucleotide (CA)15, 2 jil 100 pM dATP and H20 14 p1. Then the reaction was incubated at 37°C for 15 minutes and terminated by adding 2 p1 0.5 M EDTA (pH=8.0). After washing the membrane in 0.4 M NaOH for 20 minutes and 2XSSC for 20 minutes, I incubated the membrane in hybridization buffer for 2 hours at 42°C. (100 ml hybridization buffer was made by mixing 25 ml 20X SSC, 10 ml 10% nonfat milk dissolved in buffer 1 (see below), 200 p110% SDS, 1 ml 10% N- 20 Lauryl Sarcosine, 40 p1 DIG-labeled probe and 65 ml H20). I rinsed off unbound probe by three washes in 6XSSC and 0.1% SDS solution for each for 5 minutes. And after one minute wash in Buffer 1 (solution of 200 mmol maleic acid, 300 mmol NaCL, 400 mmol NaOH in 2 L H20 at pH 7.5) and 0.3% Tween 20, I blocked the membrane in 10% nonfat milk dissolved in Buffer 1 for 30 minutes. Then I incubated the membrane in 1:10000 Anti-DIG-AP (ROCHE) in 10% nonfat milk Buffer 1 solution for 2 hours. After 2 washes in Buffer 1 for 15 minutes each and 1 wash in Buffer 3 (6 mmol TrisHCl, '14 mmol Trizma base, 50 mmol NaC1 in 400 ml H20) for 2 minutes, the membrane was developed overnight in the dark in a solution of 400 p1 50 mg/ml NBT, 500 p1 50 mg/ml BCIP in 60 ml Buffer3. The next day, the membrane was fixed in TE for 15 minutes. A representative analysis is shown in Figure 3. 21 Marker 56 aiLI Bl. a!Lk Retention of heterozygocity N 1.011 Loll i ol Iwterozygosity ele Marker 190 tide LOH Figure 3: Retention of heterozyogsity or loss of heterozygosity for microsatellite markers 56 and 190 shown in LOH analysis. LOH analysis was carried out for each mutant with large event mutation as described in detail in Materials and Methods section 'LOH analysis'. After separation on polyacrylamide gel and bloting, the membrane was developed. Each lane represented a result from a mutant DNA preparation. Retention of heterozygosity for a given microsatellite marker is shown by two bands, and each of them represented one allele for the locus. Loss of heterozygosity is demonstrated by loss of one band. 22 DNA sequencing for small mutational event: 1 Cuss 2 3 4 5 JIAI'RT5 APRT5A ............................................................ APRT4;s QIAPRT5 QJ%PRT3' ............................................................. .4 APItT-4 Figure 4: Primers used to amplify and sequence mouse Aprt gene. The mouse Aprt gene is 2.3 kb long and contains five exons which are shown in box regions. CH5S, QIAPRT3, APRT-GS, QIAPRT5 and QIAPRT3' were used for amplification. The fragments amplified by each pair of primers are showed with dashed lines. CH5S, APRT-4 and QIAPRT3' were used for sequencing. See Materials and methods section' DNA sequence analysis' for detail. The basic scheme for the amplification of Aprt regions for a sequence analysis is shown in Figure 4. Exon 1 and 2 are amplified by primer pair: CH5S (GCTTGTGTTTAGGCAGCTCAAG) and QIAprt3 (GAGCAGAGTTCGTCTCTAGGAAC). Exon 3 and exon 4 are amplified by Aprt-GS (AGCAAAGACCTAGTGTTCCTAGCAAG) and Aprt-5A (CGGTAGCTCACAAAGGTCACTTAG) . Exon 4 and exon 5 are amplified by QiAPRT5 (GTAAATGTGGGTGCTCAGAGAG) and QiAPRT3' (CTTGTCCCTGTAGTGTCACTCTG). PCR was conducted under the following conditions. First denature at 94°C for 3 minutes, followed by 35 cycles of denature at 94°C for 30 seconds, annealing at 58°C for 30 seconds, extension at 72 °C for 1 minute by Taq, finally extension at 72 by additional 10 minutes. 23 The PCR products were separated on a 1.2% agarose gel, and purified with a purification kit (Qiagen). DNA fragments were then sequenced by an automated sequencer. The sequences for exon 1 and 2 were obtained with primer CH5S. The sequences for exon 3 and 4 were obtained with primer Aprt-4 (CTTAGTCAGCACCCAGGACAG). The sequences of exon 5 were obtained with QiAPRT3'. Statistical analysis: The difference between spontaneous and IR-exposed mutant frequencies (Table 1 & 2, Figure 6 & 7) was tested using the Wilcoxian signed-rank pair test for paired data. A 90% confidence interval was found by first log-transforming the data and then inverting the signed-rank test. All tests were performed at a significance level of 0.05. One sided p-values were used due to the expected ranking between spontaneous and IR-induced mutant frequencies. To determine IR effects for specific mutational events, the number of spontaneous mutations and those from the IR-exposed cells was tabulated for each of the four separate classes of mutation (mitotic recombination, chromosome loss, deletion, and intragenic). Fisher's exact test was then used to determine whether the type of mutation was independent of how it came about (spontaneous vs. IR-induced). When this overall test was significant, a separate Fisher's exact test was performed for each mutational type (vs. all others combined) to isolate the mutation(s) responsible for significance. 24 Results Effect of Mlhl status on cell survival to ionizing radiation. The influence of MMR status on cell viability after exposure to JR has been examined by several groups. A group using Msh2 null primary mouse epithelial cell lines showed hypersensitivity of these cells to X rays compared with Msh2 proficient cells, with relative reduction of cell survival compared to wild type cells of approximately 1.5 fold [33]. Two other groups reported slight resistance to IR for MMR deficient cells: one group used mouse fibroblast cells deficient for Pms2, Mihi, or Msh2 [36], and the other group used mouse embryonic stem cells exposed to low-level JR [37]. In contrast two other groups, one using HeLa and Raji Cells and the other using human ovarian cancer, endometrial carcinoma and colorectal carcinoma cell lines, found that MMR status does not affect cell survival after exposure to IR. Jt has been suggested that the different results obtained by these groups may be due to other factors other than MMR, since clones from the same parental cells could acquire slightly different traits during clonal selection in different labs. In a recent study, investigators switched MMR status by regulation with doxycycline, and found that Mihi status had no effect on cell survival to JR [38]. To determine JR resistance I irradiated the Mihi null cell line K634 and the DNA repair proficient cell line K06 at '37Cs-y doses from iGy to 8 Gy. I found cell survival for the Mihi null K634 similar to that for Mihi proficient K06 (Figure 5). K435 is a cell line with a G:C to C:G mutator phenotype. It displayed 25 normal sensitivity to JR killing when compared with wild type cells in a previous study 11391. From the initial experiment, I can conclude that Mihi status did not affect sensitivity to JR killing. 120% 100% I Survival 60% 40% 20% 0% 2 4 6 8 20% 137Cs-y radiation (Gy) Figure 5 Cell survival to ionizing radiation. Mihi null K634 cells and the DNA repair proficient K06 cells were exposed to various doses of '37Cs-y radiation indicated in the figure. The relative cloning efficiencies were determined and plotted. Mutagenic effect from JR on Mihi null cells Environmental mutagenesis can be studied by determining mutant frequencies and mutational spectra induced by a given genotoxin. Any alteration in either of these two endpoints demonstrates the mutagenic effects of the genotoxin on the cell genome. J first studied the effect of JR on mutant frequencies by exposing the Mihi null K634, K06 and K435 cells to 6 Gy radiation and scoring mutant frequencies (Table 1, Figure 6). Table 1. Mutant frequency X1Ofor JR-exposed and unexposed kidney cell line subclone? Mihi null K634 Spontaneous mutant Subclonesb 3c 5b 3d JR-exposed mutant freq.d freq.c 3.0 4.2 3.5 28 30 23 lb 16 14 68 60 4c Average (Stand. Dev.) 29 16 (11) 31 K435 subclones (G:C to C:G mutator phenotype) Spontaneous mutant freq. JR-exposed mutant freq. 2.7 4.4 0.8 0.6 2.3 10 ic 6b la 1 2 3 4 5 6 7 8 9 10 14 15 Average (Stand. Dev.) 1.0 2.2 9.6 2.2 0.8 9.8 0.5 3.1 (3.8) 16 19 62 13 37 (23) 3.0 6.0 0.8 1.6 2.3 5.8 9.0 13 1.5 1.5 1.6 4.5 (5.6) 27 K06 subclones (DNA repair proficient) Spontaneous Mutant Freg. 204 3.1 10 205 206 207 221 0.3 0.2 0.1 0.3 0.03 0.5 0.03 0.08 0.46 (1.0) 5.3 0.6 0.6 224 225 226 230 Average (Stand. Dev.) JR-exposed mutant freq. 1.5 0.03 0.7 0.7 0.2 2.1 (3.6) a The data from the table are plotted in Fgure 6. b Each subclone was expanded and split for determination of spontaneous and IRinduced mutant frequencies. c Mutant frequencies for cells not exposed to JR d Mutant frequencies for cells exposed to 6 Gy '37Cs-y radiation. 28 LOO4U LQi-O3 I 1.ODE-DS i .00E-C16 pIL K6S4 IR SJOIL Xc 1k So K43 1k Figure 6. Mutant frequencies for JR-exposed and unexposed subclones for three kidney cell lines. The three cell lines tested were Mihi null K634, DNA repair proficient K06 and K435 with a G:C to C:G mutator phenotype. Each subclone of these cell lines was grown and split to two cultures. One was exposed to 6 Gy 137Cs-? radiation, and the other was unexposed. Then the mutant frequencies were determined and plotted, and each pair are connected by lines. The average IR-induced mutant frequency for DNA repair proficient K06 is 2.1 X iO (Tablel), which is approximately 4.6 fold higher than the spontaneous mutant frequency. This change was statistically significant ( p <0.015). The calculated number of JR-induced mutations was approximately 1 in every 6000 cells. The result demonstrates a mutagenic response to JR for K06, which is consistent with general knowledge that JR is a mutagen. In a previous study in our lab 35], the G:C to C:G transversion phenotype in the K435 cells was shown not to be due to a deficiency in MMR system. K634 is an Mihi null cell line. Because these cell lines have a high spontaneous mutant 29 frequency, the next question I wanted to address was whether they would exhibit a mutagenic response to JR. Addressing this question would allow me to determine if the defects present in the K435 and/or K634 cells (Mihi null ) would cause an unusual mutagenic response to JR. These defects could lead to an altered cellular response to JR or a failure to repair the damage. If JR-induced repair and cell defects were independent of each other, the mutagenic effect could be cumulative. If they interacted with each other, the effects could be synergistic. Alternatively, if there was no unusual response to JR-exposure, the high spontaneous mutant frequency would mask the JR mutagenic effect. The spontaneous mutant frequency of K435 was high (3.1 X 1O) (Table 1) which is 6.7 fold higher than K06 cells. This is due to the high mutation rate for G:C to C:G mutation in this cell line. After JR-exposure, the increase in mutant frequency was not statistically significant (p <0.133). This didn't exclude the possibility that there was a mutagenic effect of JR to K435, but instead suggests that at best there was only an additive effect. If JR-induced mutations in 1 of every 6000 K435 cells (the JR effect in DNA repair proficient cells K06 cells), this would only add 1.7 X iO to the high spontaneous mutant frequency, which would be masked by the high spontaneous background. Consistent with the mutator phenotype conferred by Mihi deficiency, Mihi null K634 had a high spontaneous mutant frequency (16 X 1 0) (Table 1). This high spontaneous background could mask the mutagenic effects of genotoxins, as it was difficult to consistently detect increased mutant frequencies after these cells 30 were exposed to ultraviolet radiation (UV) or hydrogen peroxide [40]. Yet this was not the case for JR-exposure. The average mutant frequency for Mihi null K634 exposure to JR was 37 X 10 (Table 1), which was about a 2.3 fold increase over that for nonexposed cells (p < 0.024). This modest relative increase translated to a very large absolute induction of 20 X iO above the spontaneous background, or approximately one JR-induced mutation for every 500 MIhi null K634 cells. This level of induction was approximately 12 fold higher than that in the K06 cells (one induced mutant in every of 6000 cells). This difference suggested a hypermutagenic effect of JR in the MI/il deficient K634 cells, and that Mihi deficiency and JR-exposure have a synergistic effect, not an additive effect. This interaction may play a significant role in prevention of JR caused DNA damage leading to mutations. The hypermutagenic response in the Mihi null cells is due to the induction of mitotic recombinational events. To determine the types of mutations induced by IR, I first distinguished between large and small event mutations in the mutant Mihi null cells by detection of loss or retention of the wild type Aprt alleles. In unexposed Mihi null K634 cells, 81% of the spontaneous mutations were small events and 19% were due to large events. After exposure to IR, large events accounted for 65% of all the mutations, and small events decreased to 35%. This shift in mutational spectra suggested IR-induced large event mutations in Mihi null cells. 31 To determine the types of large mutational events that were induced by JR in the Mihi null cells, I analyzed the distribution of LOH for microsatellite markers along chromosome 8 (Table 2). By multiplying the percentage of each type of large and small mutations with the mutant frequency of the cells, I obtained frequencies for each type of mutational events (Table 3). Overall, the combined mutational spectra for the JR-exposed DNA repair proficient K06 cells were statistically different than the spectra of non-irradiated K06, although for any of the three types of large event mutations a statistical difference between the non-irradiated and irradiated K06 can not be reached. Nonetheless a 5-10 fold increase in the frequency for each of these three types of large events was observed. (Table 3) This suggested that the increase in mutant frequency for JR-exposed K06 was a result of a combined effect of the increase for all three types of large event mutations (Figure 7). 32 Table 2. Spectrum of mutations for JR-exposed and unexposed cells. K634 cell line (Mihi null). Mutationa Unexposed' 12 (17%) JR-exposed" Mitotic Recombination Deletion Chromosome Loss Intragenic (1.3%) (1.3%) 27 (52%) 3 (5.3%) 5 (8.8%) 58 (81%) 22 (39%) Total Samples 72 57 1 1 K435 cell line (G:C to C:G mutator phenotype) Mutation IR-exposed Spontaneous Mitotic Recombination Deletion Chromosome Loss Intragenic 1 (3.7%) 1 (3.7%) 2 (7.4%) 2 (7.1%) 3 (11%) 7 (25%) 23 (85%) 16 (57%) Total Samples 27 28 K06 cell line (DNA repair proficient) Mutation Spontaneous Mitotic Recombination Deletion Chromosome Loss Intragenic 5 (18%) Total Samples 1 (3.6%) IR-exposed 10 (40%) 2 (8.0%) 11(39%) 13 (52%) 8 (29%) 0 28 25 a The different classes of mutations identified with the molecular analysis b The number of mutations identified for each mutational class from the total number of samples examined. 33 Table 3 Frequency X1O of each mutational eventz K634 cell line (Mihi null) Mutation Spontaneous IR-exposed Mitotic Recombination Deletion 3.42 0.33 2.04 Chromosome Loss Intragenic 0.33 12.0 18.5 3.45 12.5 K435 cell line (G:C to C:C mutator phenotyj) Mutation Spontaneous IR-exposed Mitotic Recombination Deletion Chromosome Loss Intragenic 0.11 0.11 0.23 2.62 K06 cell line (DNA repair proficient) Mutation Spontaneous Mitotic Recombination Deletion Chromosome Loss Intragenic 0.10 0.01 0.21 0.13 a Data from this table are plotted in Figure 7. 0.39 0.57 1.34 3.05 JR-exposed 0.86 0.17 1.11 34 2x103 Mutant Frequency 1xIO 1nragenc vfltS hromome ks )tk recombinabon .cp o'. Figure 7. The frequencies of mutational events with or without JR-exposure. The relative frequencies for each of the four mutational categories (intragenic events, chromosome loss, deletion, mitotic recombination) are shown in Table 3 and plotted here. Spon, spontaneous mutant frequencies; IR, mutant frequencies in IR-exposed cells. Although most large spontaneous events examined (12 of 14) in the Mihi null K634 cells were due to mitotic recombination (Table 2), these events represented only 17% of all spontaneous mutations. Most large mutational events in the IRexposed K634 cells were also due to mitotic recombination (27 of 35), representing nearly half of all mutational events (47%) in the IR-exposed cells. (p <0.001). This led to a determination that one in every 670 JR-exposed Mliii null cells had an induced mitotic recombination between chromosome 8 homologues. This induced frequency is nearly 20 fold higher than that observed in DNA proficient K06 cells, in which one in approximately 13000 JR-exposed K06 cells had a mitotic recombinational event suggesting that JR-exposure had a synergistic 35 effect on the induction of mitotic recombination in Mihi null K634 cells. An additive effect of JR exposure would have added just 0.76 X iO to the spontaneous mitotic recombination frequency in Mihi null K634 cells, which would have been masked by the high spontaneous background. This synergistic induction of mitotic recombination by JR-exposure contributed to most of the IR- induced mutations (75%) in the Mi/il null K634 cells. After JR-exposure, the frequency of mitotic recombinational events (18.5 X 1 O) exceeded that of intragenic events (12.5 X 10k) (Table 3, Figure 7). Jncreased numbers of deletional events and chromosome loss were also observed in the JR-exposed Mihi null K634 cells, but these changes were not statistically significant (p < 0.32 1 and 0.087 respectively), or as dramatic as that of mitotic recombination. No increase in intragenic mutational events was observed after Mihl null K634 was exposed to JR. Spontaneous frequency of small event mutations was 12.0 X iO, and it was essentially the same in JR-exposed cells (12.5 X 10) (Table 3, Figure 7). To determine if IR-exposure altered the types of base pair substitution, J sequenced some Aprt mutants from unexposed and JR-exposed Mihi null K634 cells. My group has previously shown that treatment of the K634 cells with hydrogen peroxide or UV induced alleles with multiple base-pair substitutions [401 Only one such allele (6.7%) in the JR-exposed Mihl null K634 cells was observed, which is at the background level in this cell line. There was also no significant difference detected between unexposed and JR-induced Mihi null K634 cells for other types of mutations (Table 4, 5). J found one complex mutation in a 4 C repeat, which became a 6 C repeat, in one spontaneous mutant and one JR induced mutant from the same subclone. Therefore this was considered a single spontaneous mutation. Overall I found no effect of IRexposure on small event mutations. As Figure 7 shows, the increased mutant frequency of IR-exposed Mihi null K634 mainly stemmed from an increase in mitotic recombination. Table 4 Examples of alleles with mutations Mutation events Sefluence context exon A:T to C:G CCGGCCCCACT EXON 3 Gly to Ala Thr to Pro G:CtoA:T G:CtoA:T CGGAAAAGGGG CCGACUCCCAA CAGGTIAGACT GTT'CAGTGCGG CTAGETAGGAG CGGAAAAGGGG EXON 3 Stop EXON 1 Phe to Ser EXON 3 Leu to Arg EXON 1 Arg EXON3 Stop EXON3 Stop A:T to C:G CCGGCCCCACT (A) spontaneous mutants K634-13 G:CtoC:G K634-1 1 G:CtoA:T K634-14 K634-15 K634-16 K634-33 K634-35 A:T to G:C A:TtoC:G G:C to A:T (B) Ionizing radiated K634-5 G:CtoC:G G:CtoT:A G:CtoA:T K634-1 K634-6 K634-2 K634-3 K634-22 K634-23 K634-24 K634-25 1(634-27 G:C to A:T G:C DELETION G:C DELETION G:CtoA:T G:C to A:T GCtoC:G A:TtoT:A A:T to G:C G:CtoA:T EXON 3 Gly to Ala Thr to Pro AGGCCCCACACACA BEFORE FIRST SP1 EXON I ACGTGATVFAG before translation EXON 1 Arg to Trp GTGGCGçGGCGC EXON 3 CCGGGCCCACT EXON 1 CCGGGCTGCI'G EXON 1 Pro to Leu ACVFCCAATCC EXON I LeutoVal TGGTGGçGCGGC EXON 5 Ala to Pro CFCCGGCTGAA EXON 3 Cys to Ser GTGGGc[GTGTG EXON 4 Arg GCAGAGAGTGGT EXON 4 Glu to Lys GAGCTGiAAATC a These two mutants were derived from the same subclone which was split for being unexposed and exposed to IR. So they accounted for one spontaneous mutation. 37 Table 5 Mutation distribution at the Aprt Locus of unexposed and JR-exposed Mliii null K634 Mutation Transition A:TtoG:C G:CtoA:T Spontaneous K634 JR-exposed K634 1 1 4 6 Tansversion A:TtoT:A A:TtoC:G G:CtoC:G G:CtoT:A 0 2 0 2 2 Deletion 0 2 Cluster Multiple mutations la 1 0 1 1 1 a: These two mutants were derived from the same subclone which was split for being unexposed and exposed to JR. So they accounted for one spontaneous mutation. The overall effect of JR on the mutational spectrum in the K435 cells was not statistically significant (p < 0.121). This demonstrates that the defect underlying the G:C to C:G mutator phenotype of K435 didn't lead to a hypermutagenic increase in mitotic recombination or other mutational events after JR-exposure. 38 Discussion In this study, I showed that Mliii null cells exhibit a hypermutagenic response when exposed to IR and the hypermutagenic response in the Mliii null cells is due to the induction of mitotic recombinational events. The results can further interpreted as demonstrating that Mlhi suppresses JR-induced mutations. Therefore in this discussion, I will explore how Mihi may fit into the JR-induced cellular response to inhibit mitotic recombination. Homologous recombination (HR) can occur in meiosis and in mitosis. In mitosis, HR can use a sister chromatid as template, which is sister chromatid exchange, or a homologous chromosome as template, which is mitotic recombination. Sister chromatid exchange is accurate and can restore the original sequence, whereas mitotic recombination can change a sequence because it uses a heterologous substrate. In normal cells, sister chromatid exchange occurs at high frequency because sister chromatids are in close proximity to each other for a long period of time in S-phase and can readily be used as a template. Mitotic recombination occurs at low frequency and requires three factors. The first is physical proximity between homologs [411. The second is sufficient homology between homologs [42]. The third is an intact recombinational repair machinery. The physical proximity of homologs can occur during the cell cycle [43]. In one system [41], LOH from mitotic recombination at the Apc locus in B6 APC/mice leads to intestinal adenomas. In this mouse model, homologous recombination was the principal pathway leading to LOH. Investigators have used 39 a Robertsonian translocation fusing chromosomes 18 (containing Apc) and 7 to suppress homologous recombination by eliminating the close proximity of chromosome 18 homologs in the nucleus. This resulted in a reduction in LOH at Apc locus on chromosome 18 and a reduced incidence of intestinal adenoma. Although it is possible that MLH1 can increase mitotic recombination by moving chromosome homologs closer together, there is no evidence that loss of MMR protein affects chromosomal nuclear location. Divergent sequence between homologs has also been shown to suppress mitotic recombination. In one study, the progeny from crosses between two distantly related strains was shown to have suppressed mitotic recombination. Reintroducing sequence identity to regions of the homologous chromosome restored mitotic recombination [44j. In a recent study from the same group, they showed that sequence dependent suppression on mitotic recombination between divergent sequences was modulated by Mi/il. In this study, mitotic recombination in inter-strain mouse hybrids was suppressed in fibroblasts, and Mihi deficiency could alleviate this suppression. Msh2 was reported to suppress homologous recombination between divergent sequence 42I. This suggests that not only MLH1 but other MMR proteins might play a role into this suppression. The following may be a mechanism for the suppressive effect of MMR proteins on mitotic recombination between divergent sequences. Mismatches arising during the strand exchange could reduce the strand exchange in homologous recombination. In an in vitro reaction with a 3% divergence in sequence, the strand exchange rate was reduced 3 fold and it was suggested that this slowing down provided time for MMR proteins to detect mismatches in this process 1451. On recognition of mismatches, MMR may block ongoing strand migration and inhibit strand transfer. In vitro experiments showed that addition of MutS increased accumulation of strand transfer intermediates and addition of MutL helped to destablize the intermediate in homologous recombination between divergent sequences 1461 [451. In E coli, yeast, and mammalian cells, several studies showed that MMR proteins suppressed or prevented homologous recombination between divergent sequences 1171147114811491 [501. In my study, a moderate increase of mitotie recombination in untreated Mihi null cell lines was observed. This increase is not as large as the increase in base-pair substitution, which may be due to the low occurrence of DSBs in untreated cells. Yet this is not the case for the cells exposed to JR. A predominant DNA lesion in JR-exposed cells is the double strand break (DSB) 1511. DSBs can be repaired by non homologous end joining (NHEJ) and by homologous recombination. In mammalian cells, NHEJ is used more frequently than homologous recombination. However, recent experiments have shown that homologous recombination is also a prominent pathway [52]. NHEJ could occur in G1IGO phase and homologous recombination in S and G2 phase. There is competition between NHEJ and homologous recombination. DNA-Pkcs suppresses spontaneous and double strand break induced homologous recombination [53]. The involvement of MMR proteins in NHEJ has not been 41 studied as much as in homologous recombination. One report suggested that MLH1 may modulate NHEJ by inhibiting end annealing of DSB between noncomplementary bases or promoting annealing between microhomologies [5411. As mentioned above, homologous recombination could proceed through sister chromatide exchange or mitotic recombination. The sister chromatid is used 1001000 times more frequently than a homologous or heterologous chromosome [52]. Sister chromatid exchange is preferred to reduce the potential for genetic alteration that can occur when homologous and heterologous chromosomes are used as template. I propose that MMR proteins help to suppress mitotic recombination between homologous chromsomes and shunt DSB repair to homologous recombination between sister chromatids. If so, JR exposure and Mihi deficiency have an effect on mitotic recombination induction because mitotic recombinational events are not suppressed. Some studies investigating MMR proteins have suggested an involvement in JR activated cell cycle checkpoint pathways. One study showed that MMR deficient cells have a defective S-phase checkpoint and the cells had radiation resistant DNA synthesis [21]. However, another study using three different cell lines showed that Mihi deficient cell lines exhibited a similar S-phase response to JR as MMR proficient cell lines [34]. If a defect in the JR-induced S-phase checkpoint exists in MMR deficient cells, it should lead to an increase in base substitution after JR-exposure because replication would have occurred in the presence of oxjdative base lesion and the absence of MMR correction of the mutations. Yet in 42 my study, I could not detect increased base substitution or multiple mutations, which were observed when the Mihi null cells were exposed to hydrogen peroxide. The high background of spontaneous base substitutions may have masked a relatively low JR-induction of base substitutions. but regardless my data are inconsistent with an S-phase checkpoint defect. Studies showed IR-exposed MMR deficient human tumor cells arrested normally in G2, but were released earlier than MMR proficient cells [31] [55]. Theoretically, since most mitotic recombination occurs in G2 phase, the shortened G2 phase checkpoint caused by an earlier release in JR-exposed Mihi null cells would have led to decreased mitotic recombination because there would be less time for the recombination pathways to be initiated and resolved. However I observed a dramatic increase in mitotic recombination. The results from my study suggest that, rather than interacting with IR- activated cell checkpoint pathway, MMR proteins might be involved in DNA repair pathways after JR-exposure. My research further suggests that MMR proteins suppress a mitotic recombination pathway used to repair IR-caused DSBs and thus shunt DSBs to be repaired through sister chromatic exchange and nonhomologous end joining. The above discussion shows that JR-exposure can change Mihi null cells with microsatellite instability to cells with both microstallite and chromosomal instability because of the greatly increased mitotic recombination caused by IR. Both types of genomic instabilities could play a role in tumor suppressor gene 43 inactivation. Some suppressor genes may be more readily affected by one type of genomic instability than the other because of the different gene sequence and contexts. For example, in colorectal carcinogenesis chromosome instability was shown to be involved in inactivation of tumor suppressor genes, such as APC, p53, DCC, SMAD2, and SMAD4 1561. In contrast, microsatellite instability in colorectal cancer is involved in inactivation of TGFJJRJI, hMSH6, and BAX because they have mononucleotide runs IGFIIR, hMSH3, 11571111581. The range of suppressor genes that could be inactivated by JR-exposure would be significantly increased in cells with both types of instabilities, and this would increase malignant potential in tumor cells. Moreover, microstatellite instability would induce point mutations in the genome and lead to increased heterozyogous mutations in cells, while chromosome instability resulting LOH would convert heterozygous mutations to homozygous mutations. My observation of this cellular change from microsatellite instability to both microsatellite and chromosome instabilities without a decrease in cellular survival raises concern about the use of IR in cancer treatment because a significant percentage of some tumors commonly treated with JR are MMR deficient 1141. My research may also suggest cautions about the additional adverse effects of other mutagens in MMR deficient mammals, such as the radiomimetic agent bleomycin, which may induced double strand breaks, and thus may increase mitotic recombination in Mi/il null cells and transform the cells to a more malignant state. Conclusion Mismatch repair (MMR) proteins are involved in maintaining post replication fidelity, recognition of DNA damage by ultraviolet radiation and DNA methylating agents, and homologous recombination repair. Several articles have also suggested that MMR proteins are also involved in JR-induced cellular response by affecting cell cycle checkpoints. My graduate thesis work continues the study of the role of MMR in the response to DNA damage by focusing on how MMR proteins affect JR mutagenesis. J examined the frequency and spectra of IR-induced autosomal mutations leading to loss of Aprt expression in a mouse kidney cell line null for the Mihi gene. The increase of mutant frequency in Mihi null cells after JR-exposure demonstrated a hypermutagenic response to JR beyond the high spontaneous mutagenic trait of these cells. Mutational spectrum analysis demonstrated that most of the response was due to the induction of mitotic recombination. The high frequency induction of mitotic recombination was not observed in a DNA repair proficient cell line or a cell line with an MMRindependent mutator phenotype. These results show that JR can induce mitotic recombination in Mihi null cells and that the MLHJ protein plays an important role in suppressing these induced events. 45 Bibliography [1] A.B. Buermeyer, S.M. Deschenes, S.M. Baker and R.M. Liskay Mammalian DNA mismatch repair, Annu Rev Genet 33 (1999) 53 3-564. [2] B .D. Harfe and S. Jinks-Robertson DNA mismatch repair and genetic instability, Annu Rev Genet 34(2000) 359-399. [31 M.J. Schofield and P. Hsieh DNA mismatch repair: molecular mechanisms and biological function, Annu Rev Microbiol 57 (2003) 579608. [4] J. Jiricny and M. Nystrom-Lahti Mismatch repair defects in cancer, Curr Opin Genet Dev 10 (2000) 157-161. [5] C. Colussi, E. Parlanti, P. Degan, G. Aquilina, D. Barnes, P. Macpherson, P. Karran, M. Crescenzi, E. Dogliotti and M. Bignami The mammalian mismatch repair pathway removes DNA 8-oxodOMP incorporated from the oxidized dNTP pool, Curr Biol 12 (2002) 9 12-918. [6] A. Mazurek, M. Berardini and R. Fishel Activation of human MutS homologs by 8-oxo-guanine DNA damage, J Biol Chem 277 (2002) 82608266. [7] Y. Gu, A. Parker, T.M. Wilson, H. Bai, D.Y. Chang and A.L. Lu Human MutY homolog, a DNA glycosylase involved in base excision repair, physically and functionally interacts with mismatch repair proteins human MutS homolog 2/human MutS homolog 6, J Biol Chem 277 (2002) 11135-11142. [8] T.T. Ni, G.T. Marsischky and R.D. Kolodner MSH2 and MSH6 are required for removal of adenine misincorporated opposite 8-oxo-guanine in S. cerevisiae, Mol Cell 4 (1999) 439-444. [9] P. Karran Mechanisms of tolerance to DNA damaging therapeutic drugs, Carcinogenesis 22 (2001) 1931-1937. [101 R. Fishel Signaling mismatch repair in cancer, Nat Med 5 (1999) 12391241. [11] L. Stojic, R. Brun and J. Jiricny Mismatch repair and DNA damage signalling, DNA Repair (Amst) 3 (2004) 1091-1101. [121 J.L. Argueso, J. Wanat, Z. Gemici and E. Alani Competing crossover pathways act during meiosis in Saccharomyces cerevisiae, Genetics 168 (2004) 1805-1816. [13] N.K. Kolas and P.E. Cohen Novel and diverse functions of the DNA mismatch repair family in mammalian meiosis and recombination, Cytogenet Genome Res 107 (2004) 216-23 1. [14] J.A. Surtees, J.L. Argueso and E. Alani Mismatch repair proteins: key regulators of genetic recombination, Cytogenet Genome Res 107 (2004) 146- 159. [15] J.L. Argueso, A.W. Kijas, S. Sarin, J. Heck, M. Waase and E. Alani Systematic mutagenesis of the Saccharomyces cerevisiae MLH1 gene reveals distinct roles for Mihip in meiotic crossing over and in vegetative and meiotic mismatch repair, Mol Cell Biol 23 (2003) 873-886. [161 I. Matic, M. Radman and C. Rayssiguier Structure of recombinants from conjugational crosses between Escherichia coli donor and mismatch-repair deficient Salmonella typhimurium recipients, Genetics 136 (1994) 17-26. [17] C. Rayssiguier, D.S. Thaler and M. Radman The barrier to recombination between Escherichia coli and Salmonella typhimurium is disrupted in mismatch-repair mutants, Nature 342 (1989) 396-401. [18] K. Myung, A. Datta, C. Chen and R.D. Kolodner SGS1, the Saccharomyces cerevisiae homologue of BLM and WRN, suppresses genome instability and homeologous recombination, Nat Genet 27 (2001) 113-116. [191 G. Pedrazzi, C.Z. Bachrati, N. Selak, I. Studer, M. Petkovic, I.D. Hickson, J. Jiricny and 1. Stagljar The Bloom's syndrome helicase interacts directly with the human DNA mismatch repair protein hMSH6, Biol Chem 384 (2003) 1155-1164. [201 G. Pedrazzi, C. Perrera, H. Blaser, P. Kuster, G. Marra, S.L. Davies, G.H. Ryu, R. Freire, I.D. Hickson, J. Jiricny and I. Stagijar Direct association of Bloom's syndrome gene product with the human mismatch repair protein MLH1, Nucleic Acids Res 29 (2001) 4378-4386. [211 K.D. Brown, A. Rathi, R. Kamath, D.I. Beardsley, Q. Zhan, J.L. Mannino and R. Baskaran The mismatch repair system is required for S-phase checkpoint activation, Nat Genet 33 (2003) 80-84. 47 [22] A.J. Grosovsky, J.G. de Boer, PJ. de Jong, E.A. Drobetsky and B.W. Glickman Base substitutions, frameshifts, and small deletions constitute ionizing radiation-induced point mutations in mammalian cells, Proc Nat! Acad Sci U S A 85 (1988) 185-188. [23] K. Sankaranarayanan Ionizing radiation, genetic risk estimation and molecular biology: impact and inferences, Trends Genet 9 (1993) 79-84. [241 A. Fujimori, A. Tachibana and K. Tatsumi Allelic losses in mutations at the aprt locus of human lymphoblastoid cells, Mutat Res 269 (1992) 5562. 11251 M.S. Turker, M. Pieretti and S. Kumar Molecular evidence for the induction of large interstitial deletions on mouse chromosome 8 by ionizing radiation, Mutat Res 374 (1997) 201-208. [261 C.Y. Li, D.W. Yandell and J.B. Little Molecular mechanisms of spontaneous and induced loss of heterozygosity in human cells in vitro, Somat Cell Mol Genet 18 (1992) 77-87. [27] C.Y. Bao, A.H. Ma, H.H. Evans, M.F. Horng, J. Mend, T.E. Hui and W.D. Sedwick Molecular analysis of hypoxanthine phosphoribosyltransferase gene deletions induced by alpha- and Xradiation in human lymphoblastoid cells, Mutat Res 326 (1995) 1-15. [28] M.B. Benjamin and J.B. Little X rays induce interallelic homologous recombination at the human thymidine kinase gene, Mol Cell Biol 12 (1992) 2730-2738. [29] L. Liang, C. Shao, L. Deng, M.S. Mendonca, P.J. Stambrook and J.A. Tischfield Radiation-induced genetic instability in vivo depends on p53 status, Mutat Res 502 (2002) 69-80. [30] X.S. Xu, L. Narayanan, B. Dunklee, R.M. Liskay and P.M. Glazer Hypermutability to ionizing radiation in mismatch repair-deficient, Pms2 knockout mice, Cancer Res 61(2001) 3775-3780. [311 T.W. Davis, C. Wilson-Van Patten, M. Meyers, K.A. Kunugi, S. Cuthill, C. Reznikoff, C. Garces, C.R. Boland, T.J. Kinsella, R. Fishel and D.A. Boothman Defective expression of the DNA mismatch repair protein, MLH1, alters G2-M cell cycle checkpoint arrest following ionizing radiation, Cancer Res 58 (1998) 767-778. [32] T. Yan, J.E. Schupp, H.S. Hwang, M.W. Wagner, S.E. Berry, S. Strickfaden, M.L. Veigi, W.D. Sedwick, D.A. Boothman and T.J. Kinsella Loss of DNA mismatch repair imparts defective cdc2 signaling and G(2) arrest responses without altering survival after ionizing radiation, Cancer Res 61(2001) 8290-8297. [33] A. Franchitto, P. Pichierri, R. Piergentili, M. Crescenzi, M. Bignami and F. Palitti The mammalian mismatch repair protein MSH2 is required for correct MRE1 1 and RAD5 1 relocalization and for efficient cell cycle arrest induced by ionizing radiation in G2 phase, Oncogene 22 (2003) 2110-2120. [34] P. Cejka, L. Stojic, G. Marra and J. Jiricny Is mismatch repair really required for ionizing radiation-induced DNA damage signaling?, Nat Genet 36 (2004) 432-433; author reply 434. [35] C.Y. Shin, O.N. Ponomareva, L. Connolly and M.S. Turker A mouse kidney cell line with a G:C --> C:G transversion mutator phenotype, Mutat Res 503 (2002) 69-76. [36] J.A. Fritzell, L. Narayanan, S.M. Baker, C.E. Bronner, S.E. Andrew, T.A. Prolla, A. Bradley, F.R. Jirik, R.M. Liskay and P.M. Glazer Role of DNA mismatch repair in the cytotoxicity of ionizing radiation, Cancer Res 57 (1997) 5143-5147. [37] T.L. DeWeese, J.M. Shipman, N.A. Larrier, N.M. Buckley, L.R. Kidd, J.D. Groopman, R.G. Cutler, H. te Riele and W.G. Nelson Mouse embryonic stem cells carrying one or two defective Msh2 alleles respond abnormally to oxidative stress inflicted by low-level radiation, Proc Nati Acad Sci US A 95(1998)11915-11920. [38] E. Papouli, P. Cejka and J. Jiricny Dependence of the cytotoxicity of DNA-damaging agents on the mismatch repair status of human cells, Cancer Res 64 (2004) 3391-3394. [39] B.M. Gage, D. Alroy, C.Y. Shin, O.N. Ponomareva, S. Dhar, G.G. Sharma, T.K. Pandita, M.J. Thayer and M.S. Turker Spontaneously immortalized cell lines obtained from adult Atm null mice retain sensitivity to ionizing radiation and exhibit a mutational pattern suggestive of oxidative stress, Oncogene 20 (2001) 4291-4297. [40] C.Y. Shin, I. Mellon and M.S. Turker Multiple mutations are common at mouse Aprt in genotoxin-exposed mismatch repair deficient cells, Oncogene 21(2002)1768-1776. [41] K.M. Haigis and W.F. Dove A Robertsonian translocation suppresses a somatic recombination pathway to loss of heterozygosity, Nat Genet 33 (2003) 33-39. [42] C. Shao, L. Deng, Y. Chen, R. Kucherlapati, P.J. Stambrook and J.A. Tischfield Mihi mediates tissue-specific regulation of mitotic recombination, Oncogene 23 (2004) 9017-9024. [43] A. Garcia-Bellido and F. Wandosell The effect of inversions on mitotic recombination in Drosophila melanogaster, Mo! Gen Genet 161 (1978) 317-321. [44] C. Shao, P.J. Stambrook and J.A. Tischfield Mitotic recombination is suppressed by chromosomal divergence in hybrids of distantly related mouse strains, Nat Genet 28 (2001) 169-172. [45] L. Worth, Jr., T. Bader, J. Yang and S. Clark Role of MutS ATPase activity in MutS,L-dependent block of in vitro strand transfer, J Biol Chem 273 (1998) 23 176-23182. [46] L. Worth, Jr., S. Clark, M. Radman and P. Modrich Mismatch repair proteins MutS and MutL inhibit RecA-catalyzed strand transfer between diverged DNAs, Proc Nat! Acad Sci U S A 91(1994) 3238-3241. [47] A. Nicholson, M. Hendrix, S. Jinks-Robertson and G.F. Crouse Regulation of mitotic homeologous recombination in yeast. Functions of mismatch repair and nucleotide excision repair genes, Genetics 154 (2000) 133-146. [48] N. de Wind, M. Dekker, A. Berns, M. Radman and H. te Riele Inactivation of the mouse Msh2 gene results in mismatch repair deficiency, methylation tolerance, hyperrecombination, and predisposition to cancer, Cell 82 (1995) 321-330. 149] A. Abuin, H. Zhang and A. Bradley Genetic analysis of mouse embryonic stem cells bearing Msh3 and Msh2 single and compound mutations, Mol Cell Biol 20 (2000) 149-157. [501 B. Elliott and M. Jasin Repair of double-strand breaks by homologous recombination in mismatch repair-defective mammalian cells, Mo! Cell Biol 21(2001) 2671-2682. [511 F. Hutchinson Chemical changes induced in DNA by ionizing radiation, Prog Nucleic Acid Res Mol Biol 32 (1985) 115-154. L 50 [321 11531 11541 R.D. Johnson and M. Jasin Double-strand-break-induced homologous recombination in mammalian cells, Biochem Soc Trans 29 (2001) 196201. C. Allen, A. Kurimasa, M.A. Brenneman, D.J. Chen and J.A. Nickoloff DNA-dependent protein kinase suppresses double-strand break-induced and spontaneous homologous recombination, Proc Nati Acad Sci U S A 99 (2002) 3758-3763. L.A. Bannister, B.C. Waidman and A.S. Waidman Modulation of errorprone double-strand break repair in mammalian chromosomes by DNA mismatch repair protein Mihi, DNA Repair (Amst) 3 (2004) 465-474. [55] G. Aquilina, M. Crescenzi and M. Bignami Mismatch repair, G(2)IM cell cycle arrest and lethality after DNA damage, Carcinogenesis 20 (1999) 2317-2326. [56] A. Goel, C.N. Arnold, D. Niedzwiecki, D.K. Chang, L. Ricciardiello, J.M. Carethers, J.M. Dowell, L. Wasserman, C. Compton, R.J. Mayer, M.M. Bertagnolli and C.R. Boland Characterization of sporadic colon cancer by patterns of genomic instability, Cancer Res 63 (2003) 1608-1614. 11571 [58] R. Parsons, L.L. Myeroff, B. Liu, J.K. Wilison, S.D. Markowitz, K.W. Kinzler and B. Vogelstein Microsatellite instability and mutations of the transforming growth factor beta type II receptor gene in colorectal cancer, Cancer Res 55 (1995) 5548-5550. J.R. Eshleman, G. Casey, M.E. Kochera, W.D. Sedwick, S.E. Swinler, M.L. Veigi, J.K. Willson, S. Schwartz and S.D. Markowitz Chromosome number and structure both are markedly stable in RER colorectal cancers and are not destabilized by mutation of p53, Oncogene 17 (1998) 719-725.