Massachusetts Institute of Technolog Massachusetts Institute of Technology Harvard Medical Schoo
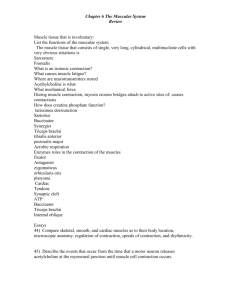
advertisement

Massachusetts Institute of Technology Technolog Harvard Medical School Schoo Brigham and Women’s Hospital VA Boston Healthcare System 2.79J/3.96J/20.441/HST522J BIOMATERIALS--TISSUE INTERACTIONS: BIOMATERIALS “T l ” ffor U “Tools Understanding d di the h M Molecular, l l C Cellular, ll l and Physiological Bases of the Tissue Response to Implants p M. Spector Spector,, Ph.D. BIOMATERIALS-TISSUE INTERACTIONS Tissue* + Biomaterial** Cell + Matrix** * Structure comprising cells of the same type ** Solid surface CELL-MATRIX INTERACTIONS In Tissue Tissu Cell + Extracellular Matrix In Tissue Engineering Scaffolds Cell + Biomaterial Scaffold CONCEPTS FOR UNDERSTANDING BIOMATERIALS-TISSUE INTERACTIONS • • • • • Control Volume Unit Cell Processes Types of Tissues Tissue Tissue Formation and Remodeling In Vitro W Wound dH Healing li In I Vi Vivo Articular Cartilage Extracellular Extracellular Matrix Cell Figures by MIT OpenCourseWare. 4 mm 10 μm Chondrocytes (P2 Canine) in a Type I Collagen-GAG Scaffold 40min Courtesy Elsevier, Inc., http://www.sciencedirect.com. Used with permission. 2 1 3 “Control Volume” 4 B. Kinner 5 Zaleskas, J. M., et al. "Contractile forces generated by articular chondrocytes in collagen-glycosaminoglycan matrices." Biomaterials 25 no. 7-8 (2004):1299-1308. 6 UNIT CELL PROCESSES Concept of a “Control Volume” around a Cell Soluble Regulator A Cell Matrix Cell + Matrix Product + Soluble (Regulator) Regulator B (Regulator) Product “Control Volume” UNIT CELL PROCESSES Concept of a “Control Volume” around a Cell Soluble Regulator Autocrine factor Cell Matrix Cell + + Matrix Product + Soluble (Regulator) (Regulator) Regulator Product “Control Volume” Another Cell; Circulation; Paracrine Endocrine UNIT CELL PROCESSES Concept of a “Control Volume” around a Cell Soluble Mechanical Regulator Loading (Strain); Subject 2.785 A Cell Cell ++ Matrix Matrix Product + Soluble (Regulator) Regulator B (Regulator) Product “Control Volume” CONCEPTS FOR UNDERSTANDING BIOMATERIALS-TISSUE INTERACTIONS • • • • • Control Volume Unit Cell Processes Types of Tissues Tissue Tissue Formation and Remodeling In Vitro W Wound dH Healing li In I Vi Vivo UNIT CELL PROCESSES • • • • • • Mitosis Migration Synthesis C Contraction i Endocytosis Exocytosis UNIT CELL PROCESSES • • • • • • • • Mitosis Migration Synthesis C Contraction i Endocytosis Exocytosis ? ? UNIT CELL PROCESSES • • • • • • • • Mitosis Migration Synthesis C Contraction i Endocytosis Exocytosis Apoptosis Differentiation COLLAGEN-GAG MATRICES: MODEL BIOMATERIALS (ANALOGS OF EXTRACELLULAR MATRIX) Investigation of cell interactions (UCPs) in vitro • Type I (bovine and porcine) • Type T II ((porcine) i ) • Chondroitin 6-sulfate 1mm • Freeze-dried • Dehydrothermally cross cross-linked linked • Additional cross-linking See IV Yannas, et al. PNAS, 1989 500μm – CELL –MATRIX INTERACTIONS WITH COLLAGEN-GAG MATRICES IN VITRO • Can provide insights into interrelationships among cell processes. – How do mitosis and synthesis interrelate? – How do mitosis and synthesis relate to contraction? – How does migration relate to contraction? • Can provide insights into cell behavior in vivo. • Can provide insights into scaffold composition and structure for improved p p performance in regenerative medicine. Chondrocytes (Passage 2 Canine) in a Type I Collagen-GAG Collagen GAG Matrix Live cell imaging for a period of 5 hours. J. Cheng CELL –MATRIX INTERACTIONS • • • • Mitosis Migration S th i Synthesis Contraction Chondrocyte (P2 Canine) in a Type I Collagen-GAG Matrix: Mitosis Photo removed due to copyright restrictions. J. Cheng Effects of Cross-Linking on Chondrocyte Proliferation DNA Content in Collagen-GAG Matrices 60 Mean ± SEM DN NA (ug g) 50 DHT UV GTA EDAC 40 30 20 Inc. cross cross-linking 10 0 00 10 10 Day 20 20 30 30 CR Lee, et al., Biomat. 2001;22:3145 CELL ±MATRIX INTERACTIONS Mitosis Migration Synthesis Contraction Fibroblasts Migrate Away from Soft Substrates NIH 3T3 cells are plated on polyacrylamide substrates with a transition in flexibility. The soft side is marked with fluorescent beads (to the left). Cells turn to avoid the soft substrate as they approach the boundary from the stiff side, by retracting the leading lamellipodium that crossed the boundary. Courtesy of Yu-Li Wang. Used with permission. C.-M. Lo, et al., Biophys. J. 79:144 (2000) Fibroblasts Migrate Toward Stiff Substrates NIH 3T3 cells are plated on polyacrylamide substrates with a transition in flexibility. The soft side is marked with fluorescent beads (to the left). Cells turn toward and enter the stiff side as they approach the boundary from the soft side, by expanding protrusions toward the boundary into a leading lamellipodium. Courtesy of Yu-Li Wang. Used with permission. C.-M. Lo, et al., Biophys. J. 79:144 (2000) Fibroblasts Migrate Toward Stretching Forces NIH 3T3 cells are plated on polyacrylamide substrates. Pulling forces are exerted by inserting a blunted needle in the substrate near the trailing end of the cell and dragging the needle away from the cell. Cells switch the direction of migration by expanding secondary protrusions toward the needle into a leading lamellipodium. Courtesy of Elsevier, Inc., http://www.sciencedirect.com. Used with permission. C.-M. Lo, et al., Biophys. J. 79:144 (2000) Fibroblasts Migrate Away from Compressing Forces NIH 3T3 cells are plated on polyacrylamide substrates. Pushing forces are exerted by inserting a blunted needle in the substrate near the leading edge of an approaching cell and moving the needle toward the cell. Cells switch the direction of migration by retracting the leading lamellipodium. Courtesy of Elsevier, Inc., http://www.sciencedirect.com. Used with permission. C.-M. Lo, et al., Biophys. J. 79:144 (2000) Migration of Epithelial Cells In Vitro in a Wound Healing Assay 100 μm © 2001 L. C. Santy and J. E. Casanova. License CC BY-NC-SA. Published by The Rockefeller Published Rockefeller University University Press. Press http://dx.doi.org/10.1083/jcb.200104019 Monolayers were ““wounded” by scraping. LC Santy, J. Cell Biol. 154:599 (2001) Chondrocytes (P2 Canine) in a Type I CollagenGAG Matrix: Migration and Contraction 40min J. Zaleskas, et al., Biomat. 25:1299 (2004) 2 1 3 4 5 B. Kinner 6 Courtesy Elsevier, Inc., http://www.sciencedirect.com. Used with permission. Diagram removed due to copyright restrictions. Fig. 2 in Fi i MMad dri, i Kid KidneyIInt. 41 (1992): (1992) 562. 562 Schematic of the modulation of microvascular endothelial cell phenotype during angiogenesis. Madri, Kidney Int. 41:562 (1992) CELL –MATRIX INTERACTIONS • • • • Mitosis Migration Synthesis Contraction nmol/h hour/μ hour/ μg DNA Effects of Cross-Linking on Chondrocyte Biosynthesis in Collagen-GAG- Matrices 01 0.15 Protein Synthesis; p Proline Incorporation DHT UV GTA EDC 0.1 0.03 0.02 0.05 0.01 0 0 2 7 15 Day 29 Proteoglycan Synthesis; Sulfate Incorporation 2 7 15 29 Day CR Lee, et al., Biomat. 2001;22:3145 CELL –MATRIX INTERACTIONS • • • • Mitosis Migration Synthesis Contraction α-smooth muscle actin-fusion peptide (SMA-FP) inhibits the tension exerted by lung fibroblasts on silicone substrates. After washing our of the FP, cells contract again. See video at http://jcb.rupress.org/content/suppl/2002/05/03/jcb.200201049.DC1/1.html Hinz B, et al., J Cell Biol 157:657 (2002) Chondrocytes (P2 Canine) in a Type I Collagen-GAG g Matrix: Contraction J. Zaleskas, et al., Biomat. 25:1299 (2004) 40 min Courtesy Elsevier, Inc., http://www.sciencedirect.com. Used with permission. B Kinner 40 min 40 min 300 min Courtesy Elsevier, Inc., http://www.sciencedirect.com. Used with permission. J. Zaleskas, et al., Biomat. 25:1299 (2004) Non-Seeded: 8 days Non-Seeded: 8 days Cell-Seeded: - 88 days Cell-Seeded: days 10mm 10 10mm Non-Seeded and Cell-Seeded Collagen-GAG Scaffolds S. Vickers Courtesy of Scott Vickers. Used with permission. 21 days Adult canine articular chondrocytes (passage 3)3) contract a type I I Adult canine articular chondrocytes (passage contract a type collagen-GAG matrix, reflected inContraction thethe decrease inin diameter collagen-GAG g Cell matrix, , reflected in decrease diameter Cell-Mediated Mediated %O Origina al Diam meter 100 Mean ± SEM Highly x-link., high modulus 90 80 DHT UV GTA EDAC 70 60 50 40 Little x-link., low modulus 30 0 10 Day 20 30 CR Lee, et al., Biomat. 2001;22:3145 Human Articular Chondrocytes in Monolayer Culture IH - Green: α-smooth muscle actin; Orange: type II collagen Chondrocytes express the gene for α-smooth muscle actin and this enables them to contract Courtesy of John Wiley and Sons, Inc. Used with permission. Source: Kinner, B., and M. Spector. J Orthop Res 19 (2001): 233-241. B. Kinner, et al. JOR 2001;19:233 α-Smooth Muscle Actin Immunohistochemistry of Human Articular Cartilage Neg. control Courtesy of John Wiley and Sons, Inc. Used with permission. Fig 1a and b in Kim, A. C., and M. Spector. "Distribution of Chondrocytes Containing Alpha-smooth Muscle Actin in Human Articular Cartilage." J Orthop Res 18 (2000): 749. Kim and Spector, JOR 2000;18:749 MUSCULOSKELETAL CELLS THAT CAN EXPRESS a a-SMOOTH MUSCLE ACTIN AND CAN CONTRACT Articular chondrocyte Osteoblast Meniscus fibroblast and fibrochondrocyte Intervertebral disc fibroblast and fibrochondrocyte • Ligament fibroblast • Tendon fibroblast • Synovial cell M. Spector, Mesenchymal • esenchymal stem cellcell Mesenchymal stem Wound Repair Regen. • • • • 9:119:11-18 (2001) POSSIBLE ROLES FOR a-SMOOTH MUSCLE ACTIN-ENABLED CONTRACTION Musculoskeletal Connective Tissue Cells • Tissue engineering Contracture of scaffolds • Healing Closure of wounds ((skin wounds and bone fractures)) • Disease processes Contracture (Dupuytren’s) • Tissue formation Modeling of ECM architecture and remodeling (e.g., crimp in ligament/tendon?) CONCEPTS FOR UNDERSTANDING BIOMATERIALS-TISSUE INTERACTIONS • • • • • Control Volume Unit Cell Processes Types of Tissues Tissue Tissue Formation and Remodeling In Vitro W Wound dH Healing li In I Vi Vivo TYPES OF TISSUES Which Tissues Can Regenerate Spontaneously? Yes No Connective Tissues • Bone • Articular Cartilage, Ligament, Intervertebral Disc, Others Epithelia (e.g., epidermis) √ √ √ Muscle √ • Cardiac, Skeletal • Smooth Nerve √ √ BIOMATERIALS-TISSUE INTERACTIONS C ll + Matrix Cell M t i Connective Tissue Epithelia M l Muscle Nerve UNIT CELL PROCESSES Concept of a “Control Volume” around a Cell Soluble Mechanical Regulator Loading (Strain) A Cell Cell + + Matrix Matrix (Regulator) (Regulator) Product + Soluble Product Regulator B “Control Volume” BIOMATERIALS-TISSUE INTERACTIONS Cell + Matrix Connective Tissue Epithelia Muscle N Nerve Adhesion Protein Collagen Biomaterial BIOMATERIALS-TISSUE INTERACTIONS Cell + Matrix Connective Tissue Epithelia Muscle Nerve Adhesion Protein Collagen Biomaterial Integrin Chinese hamster ovary cell migration in a wound-healing assay CHO cells express the α5β1 but not α4β1 integrin C. Watters,, Cell Biol. Ed. 2:210 (2003) K.A. Pinco, Mol. Biol. Cell 13:3203 (2002) Photos removed due to copyright restrictions. Figure 3 in Watters, C. Cell Biol. Ed. 2:210 (2003) Image and links to associated videos at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC256980/figure/F3/ Cells transfected with plasmid DNAs for α4 and α4/GFP Migration of fibroblast-like fibrosarcoma cells in a 3-D collagen lattice K. Wolf, et al., J. Cell Biol. 160:267 (2003) Reduction of migration speed and induction of detached, nonmobile spherical morphology by adhesion perturbing t bi anti–α1 ti 1 iintegrin t i antibody, as a consequence of impaired collagen fibril binding. “UNIT CELL PROCESSES” Cell + Matrix Connective Tissue Epithelia Muscle Nerve UCP Mitosis S nthesis Synthesis Migration Contraction Endocytosis Exocytosis “UNIT CELL PROCESSES” Cell + Matrix Connective Tissue Epithelia Muscle N Nerve UCP Mitosis Synthesis y Product Cell proliferation Matrix molecules,, enzymes, cytokines Migration Translocation Contraction Strain Endocytosis Solubilized fragments Exocytosis Regulators “UNIT CELL PROCESSES” “ C OC SS S” Regulator UCP Cell + Matrix Connective Tissue Epithelia Muscle N Nerve Product + Regulator Mitosis Synthesis Migration Contraction Endocytosis Exocytosis Cytokines (Growth Factors) REGULATORS • Cytokines/Growth Factors – http://themedicalbiochemistrypage.org/growth http://themedicalbiochemistrypage.org/growth-factors.html – (previously: http://web.indstate.edu/thcme/mwking/growth-http://web.indstate.edu/thcme/mwking/growth factors.html • http://www.copewithcytokines.de/ “UNIT CELL PROCESSES” “ C OC SS S” Regulator Mechanical Force (Strain) UCP Ce + Matrix Cell at Product oduct + R eegulator gu ato Connective Adhesion Mitosis Tissue ssue Protein Synthesis Epithelia Collagen Migration Muscle Biomaterial Contraction Endocytosis Nerve Integrin Exocytosis Cytokines (Growth Factors) “UNIT CELL PROCESSES” “ C OC SS S” Regulator Mechanical Force (Strain) UCP Ce + Matrix Cell at Product oduct + R eegulator gu ato Connective Adhesion Mitosis Tissue ssue Protein Synthesis Epithelia Collagen Migration Muscle Biomaterial Contraction Endocytosis Nerve Integrin Exocytosis Cytokines (Growth Factors) “UNIT CELL PROCESSES” “ C OC SS S” Regulator (TGF (TGF--β1) UCP Cell + Matrix Product + Regulator Matrix strain Cytokines Mitosis Connective Adhesion (contracture/ (Growth Factors) Synthesis Tissue Protein shrinkage) g ) Migration E ith li Epithelia Collagen Muscle Biomaterial Contraction Endocytosis Nerve Exocytosis Integrin “UNIT CELL PROCESSES” “ C OC SS S” TGFTGF G -β1 Contraction Fibroblast + Collagen Contracture + Reg. CONCEPTS FOR UNDERSTANDING BIOMATERIALS - TISSUE INTERACTIONS • • • • • Control Volume Unit Cell Processes Types of Tissues Tissue Tissue Formation and Remodeling In Vitro W Wound dH Healing li In I Vi Vivo +FGF-2 TISSUE FORMATION AND REMODELING IN VITRO +FGF-2 Canine chondrocytes grown in a type II collagen-GAG scaffold for 2 weeks. (Safranin O stain for GAGs) N. Veilleux, et al., Osteoart. & Cart. 2005;13:278 Courtesy of Elsevier, Inc., http://www.sciencedirect.com. Used with permission. CONCEPTS FOR UNDERSTANDING BIOMATERIALS-TISSUE INTERACTIONS • • • • • Control Volume Unit Cell Processes Types of Tissues Tissue Tissue Formation and Remodeling In Vitro W Wound dH Healing li In I Vi Vivo WOUND HEALING Roots of Tissue Engineering Injury Inflammation (Vascularized tissue) 4 Tissue Categories Connective Tissue Epithelium Nerve Muscle R Reparative ti Process Regeneration* CT: bone Ep: eepidermis pidermis Muscle: smooth *spontaneous Repair (Scar) CT: cartilage Nerve Muscle: cardiac, skel. RESPONSE TO IMPLANTS: WOUND HEALING Surgical Implantation Acute Inflammation Vascular Response Clotting Phagocytosis Neovascularization New Collagen Synthesis Tissue of Labile and Stable Cells Tissue of Permanent Cells Implant Movement Framework F k Framework F k Intact Destroyed Regen. Scarring (incorp. (fibrous encapsulation; of implant) synovium) Chronic Inflammation Granulation Tissue Scarring S i (fibrous encapsulation; synovium) Chronic Inflammation MIT OpenCourseWare http://ocw.mit.edu 20.441J / 2.79J / 3.96J / HST.522J Biomaterials-Tissue Interactions Fall 2009 For information about citing these materials or our Terms of Use, visit: http://ocw.mit.edu/terms.