A Shingle Week in the Life of a Student of...
advertisement

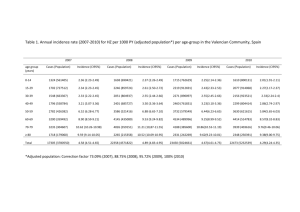
A Shingle Week in the Life of a Student of Medicine: Zoster A To Z D Bays BS, MT Khan, MD, P Kashkouli, MD, P Aronowitz, MD University of California Davis School of Medicine Introduction ■Herpes zoster is a relatively common infection with a range of clinical manifestations. During 7 days on 1 ward team, we cared for 3 different patients with herpes zoster with widely mitigating circumstances: concurrent acute generalized exanthematous pustulosis (AGEP), pyoderma gangrenosum (PG), and disseminated herpes zoster. Day 1 ■ A 24 year old man with lupus nephritis on corticosteroids and mycophenolate mofetil presented with 10 days of severe, burning pain on his back followed by a painful rash. Exam demonstrated a vesicular, erythematous rash along the left back and chest in the T4 dermatome without crossing the midline. ■ Further examination revealed a generalized rash of erythematous pustules and papules consistent with healing acute generalized exanthematous pustulosis (AGEP). On further questioning, the patient reported this was a side effect of trimethoprim/sulfamethoxazole prophylaxis started one month prior, which he had recently discontinued. ■ AGEP has been previously associated with sulfomonamides, and this case presents a reminder that detailed history and physical examination remain paramount, even with an obvious diagnosis of herpes zoster. Day 6 Day 7 ■ A 61 year old woman with a history of stage 4 laryngeal squamous cell carcinoma status post total laryngectomy and neck radiation 1 month prior to presentation and herpes zoster that began two weeks prior presented with 2 large chest ulcerations that had been increasing in size over the past week. ■ Exam demonstrated 2 large erythematous ulcerative lesions with heaped-up, violaceous borders and purulent exudate on the anterior chest consistent with PG. ■ Both of these ulcers were in the same location as crusted healing herpes zoster lesions in the T2 dermatome. ■ Mehta et al previously reported a patient with primary varicella developing PG, which they hypothesized as secondary to pathergy; however, a literature search did not demonstrate a link between PG and herpes zoster. ■ Alternatively, this could be secondary to hypersecretion of IL-8 as this has been linked with the development of PG, and varicella zoster virus infection can induce secretion of IL-8. ■ These findings could indicate that varicella zoster virus infection leads to an imbalance in the immune system predisposing to developing PG, but further research needs to be done. ■ An 89 year old man with prostate cancer who was recently started on bicalutamide presented with facial herpes zoster for one week that had now disseminated throughout his trunk and extremities. He had initially presented to an outside hospital where he was diagnosed with facial herpes zoster and then discharged without treatment. ■ He was started on IV acyclovir, but he developed altered mental status concerning for varicella zoster virus encephalitis the following day. ■ Over the next week his altered mental status resolved with IV acyclovir treatment, and the lesions eventually crusted over and he recovered. ■ While therapy is recommended for any patient over 50 who presents within 72 hours of rash onset, it is unknown if our patient’s disseminated disease could have been prevented with initial antivirals as he initially presented outside of this therapeutic window. ■ Nonetheless, this patient demonstrates the most severe, life-threatening form of herpes zoster: disseminated disease. Right Cheek Right Posterior Chest Abdomen Right Ear Axilla Case 3 Disseminated Zoster Conclusion Right Anterior Chest Case 2 Zoster + Pyoderma Gangrenosusm Case 1 Zoster + AGEP Left Breast Right Breast ■ Besides herpes zoster, the unifying feature of these patients was their relative immunocompromised state due to medical treatment and underlying disease. Beyond presenting to our care in a unique fashion, they also represent the challenge and breadth of Internal Medicine in the unique way in which one patient (or 3) can present with a common disease. References ■ Sidoroff A, Dunant A, Viboud C, Halevy S, Bavinck JN, Naldi L, Mockenhaupt M, Fagot JP, Roujeau JC. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR). Br J Dermatol. 2007;157(5):989. ■ Mehta AJ, Woodrow S, St John A. Pyoderma gangrenosum on varicella lesions. Clin Exp Dermatol. 2007 Mar;32(2):215-7. Epub 2006 Nov 27. ■ Oka M, Berking C, Nesbit M, Satyamoorthy K, Schaider H, Murphy G, Ichihashi M, Sauter E, Herlyn M. Interleukin-8 overexpression is present in pyoderma gangrenosum ulcers and leads to ulcer formation in human skin xenografts. Lab Invest. 2000 Apr;80(4):595-604. ■ Desloges N1, Schubert C, Wolff MH, Rahaus M. Varicella-zoster virus infection induces the secretion of interleukin-8. Med Microbiol Immunol. 2008 Sep;197(3):277-84. Epub 2007 Oct 2. ■ Dworkin RH, Johnson RW, Breuer J, et al. Recommendations for the management of herpes zoster. Clin Infect Dis 2007; 44 Suppl 1:S1.