Orthopaedic Graduate Research Symposium
advertisement

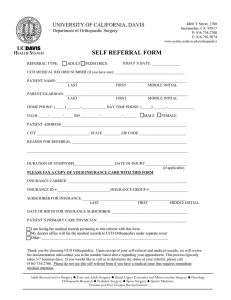
The Paul R. Lipscomb Alumni Society Presents Orthopaedic Graduate Research Symposium Friday, June 21, 2013 with special guest speaker Robert Anderson, M.D. Sponsored by University of California, Davis Health System Department of Orthopaedic Surgery Welcome to the 2013 Paul R. Lipscomb Alumni Society Graduate Research Symposium This outstanding gathering is an opportunity for our department to highlight scientific and clinical research, and to reconnect with clinical faculty and alumni who have served our department over the years. Our special guest this year is Dr. Robert Anderson, Founding Member of the Foot and Ankle Institute at OrthoCarolina. Most importantly, this is an occasion to commemorate the graduation of twelve exceptional men and women - five residents and seven fellows - into the ranks of orthopaedic surgery. While always a bittersweet occasion, this day validates the wonderful camaraderie and continuity of our field. Thank you for being part of this memorable event. Orthopaedic Surgery Chairs Paul R. Lipscomb, M.D. Professor Emeritus Chair 1969-1979 Michael W. Chapman, M.D. Professor Emeritus Chair 1979-1999 George T. Rab, M.D. Professor Chair 1999-2006 Paul E. Di Cesare, M.D., FACS Professor Michael W. Chapman Chair 2006-2011 Richard A. Marder, M.D. Professor Acting Chair 2011 - present Visiting Professors 1982 - Robert B. Winter, M.D. 1983 - Anthony Catterall, M.D. 1984 - Eugene E. Bleck, M.D. 1985 - Paul P. Griffin, M.D. 1986 - M. Mark Hoffer, M.D. 1987 - Robert B. Salter, M.D. 1988 - Colin F. Moseley, M.D. 1989 - James R. Gage, M.D. 1990 - James F. Kellam, M.D. 1991 - David S. Braddford, M.D. 1992 - Adrian E. Flatt, M.D. 1993 - Augusto Sarmiento, M.D. 1994 - M. Mark Hoffer, M.D. 1995 - James R. Andrews, M.D. 1996 - James R. Urbaniak, M.D. 1997 - Stuart L. Weinstein, M.D. 1998 - Robert A. Mann, M.D. 1999 - Joseph M. Lane, M.D. 2000 - Andrew J. Weiland, M.D. 2001 - Joel M. Matta, M.D. 2002 - Terry R. Trammell, M.D. 2003 - Kaye E. Wilkins, M.D. 2004 - Richard Gelberman, M.D. 2005 - Robert H. Hensinger, M.D. 2006 - James Heckman, M.D. 2007 - Thomas A. Einhorn, M.D. 2008 - Joseph A. Buckwalter, M.D. 2009 - Peter J. Stern, M.D. 2010 - Joseph Borrelli, Jr., M.D. 2011 - Keith Bridwell, M.D. 2012 - Gary G. Poehling, M.D. 2013 - Robert Anderson, M.D. Robert Anderson, M.D. President of the American Orthopaedic Foot and Ankle Society & Founding Member of the Foot and Ankle Institute at OrthoCarolina Dr. Anderson is a founding orthopaedic surgeon of the Foot and Ankle Institute of OrthoCarolina in Charlotte, North Carolina, practicing there since 1989. His fellowship training was in foot and ankle disorders, with a large experience in sport related injuries. He serves as a consultant to a number of NFL/NBA/ NHL/MLB teams and colleges. He is the foot and ankle consultant to MLB Umpires Division and has served as a team orthopaedist to the Carolina Panthers since 2000. He serves as the Chairman of the Foot and Ankle Subcommittee for the NFL. Additional appointments include Chief of Foot and Ankle Service at the Carolinas Medical Center, Codirector of the Fellowship Program at OrthoCarolina, and Vice-chief of the Department of Orthopaedic Surgery at OrthoCarolina. He is a Past President of the Medical Staff of Carolinas Medical Center with 1700 physician members. Dr. Anderson is also a past-president of the American Orthopaedic Foot and Ankle Society. Research appointments include Editor-in-Chief of Techniques in Foot and Ankle Surgery; associate editor/reviewer for JBJS, JAAOS, AJSM and numerous other peer-review publications. He has authored numerous other book chapters and manuscripts. He was born in Milwaukee, Wisconsin and attended the University of Mississippi. He completed his medical degree at the Medical College of Wisconsin (formerly Marquette School of Medicine), completed his residency at Carolinas Medical Center in Orthopedic Surgery and a fellowship at the Medical College of Wisconsin in foot and ankle surgery. Faculty University of California Davis Health System KYRIACOS A. ATHANASIOU, Ph.D., Ph.M. Distinguished Professor, Orthopaedic Research and Biomedical Engineering ROBERT H. ALLEN, M.D. Associate Professor, Hand and Upper Extremity BLAINE A. CHRISTIANSEN, Ph.D. Assistant Professor, Orthopaedic Research Laboratory RAKESH DONTHINENI, M.D. Associate Clinical Professor, Oncology JONATHAN G. EASTMAN, M.D. Assistant Professor, Trauma Service TANIA A. FERGUSON, M.D., MAS Associate Professor, Trauma Service DAVID P. FYHRIE, Ph.D. Professor, Orthopaedic Research Laboratory MAURO M. GIORDANI, M.D. Associate Professor, Chief of Adult Reconstructive Service ERIC GIZA, M.D. Associate Professor, Chief of Foot and Ankle Service MUNISH C. GUPTA, M.D. Professor, Chief of Adult and Pediatric Spine Service DOMINIK R. HAUDENSCHILD, Ph.D. Assistant Professor, Orthopaedic Research Laboratory ERIC O. KLINEBERG, M.D. Assistant Professor, Adult and Pediatric Spine Service J. KENT LEACH, Ph.D. Associate Professor, Orthopaedic Research Laboratory and Biomedical Engineering CASSANDRA A. LEE, M.D. Assistant Professor, Sports Medicine MARK A. LEE, M.D. Associate Professor, Trauma Service RICHARD A. MARDER, M.D. Professor and Acting Chair, Chief of Sports Medicine GAVIN C.T. PEREIRA, MBBS, FRCS Assistant Professor, Adult Reconstructive Service DEBRA J. POPEJOY, M.D. Assistant Professor, Pediatric Orthopaedics GEORGE T. RAB, M.D. Professor, Pediatric Orthopaedics A. HARI REDDI, Ph.D. Distinguished Professor, Lawrence J. Ellison Chair of Molecular Biology, Acting Director of the Orthopaedic Research Laboratories, Acting Vice Chair ROLANDO F. ROBERTO, M.D. Associate Professor, Adult and Pediatric Spine Surgery PETER B. SALAMON, M.D. Clinical Professor, Pediatric Orthopaedics ROBERT M. SZABO, M.D., MPH Professor, Chief of Hand, Upper Extremity and Microvascular Surgery JAMES M. VAN DEN BOGAERDE, M.D. Assistant Professor, Sports Medicine PHILIP R. WOLINSKY, M.D. Professor, Chief of Trauma Service BRAD J. YOO, M.D. Associate Professor, Trauma Service Faculty Shriners Hospital for Children Northern California ANDREA S. BAUER, M.D. Assistant Professor, Pediatric Orthopaedics JENNETTE L. BOAKES, M.D. Clinical Professor, Pediatric Orthopaedics JON R. DAVIDS, M.D. Associate Professor, Pediatric Orthopaedics MICHELLE A. JAMES, M.D. Clinical Professor, Chief of Orthopaedics Pediatric Service JOEL A. LERMAN, M.D. Associate Clinical Professor, Pediatric Orthopaedics Program Friday, June 21, 2013 Resident and Fellow Research Presentations Medical Education Building, Lecture Hall 1222 7:15 AM Continental Breakfast 7:45 AM Welcome - Richard A. Marder, M.D., Professor and Acting Department Chair 7:55 AM Introduction of Guest Speaker Eric Giza, M.D. 8:00 AM Visiting Professor: Robert Anderson, M.D., Founding Member of the Foot and Ankle Institute at OrthoCarolina “Sports Foot and Ankle Injuries in the NFL” 9:00 AM Alumni Lectures (Young Alumni) “What is it like out there 2-3 years after graduation?” 9:30 AM BREAK 9:40 AM Philbert Y. Huang, M.D., Ph.D. “Injuries to the PCL Complex and Medial Structures of the Knee: Finite Element Analysis” 10:00 AM Raj S. Kullar, M.D. 10:20 AM Lance K. Mitsunaga, M.D. “Can a Universal Protocol for Prevention of Surgical Site Infections Reduce Postoperative Infection Rates to Zero in Spine Surgery Patients?” “The Properties of the Subscapularis Following Repair in Reverse Total Shoulder Arthroplasty: a Cadaveric and Biomechanical Analysis” 10:40 AM Daemeon A. Nicolaou, M.D. “Comparison in Fatigue Strength of Various Plaster Posterior Short Leg Splint Configurations” 11:00 AM Derek F. Amanatullah, M.D., Ph.D. “Calculating the Position of the Joint Line of the Knee in Relationship to Anatomic Landmarks” 11:30 AM BREAK (PHOTOS) 12:00 PM Bryon D. Hobby, M.D. “Analysis of Patient Outcomes Following Anterior Approach Total Hip Arthroplasty for Femoral Neck Fracture” 12:10 PM David L. Rothberg, M.D. “Posterior Facet Cartilage Injury in Operatively Treated Intraarticular Calcaneus Fractures” 12:20 PM John David Burrow, D.O. “Evaluation of Knee Kinematics in the Sagittal and Coronal Planes in Navigation Assisted Total Knee Arthroplasty and Correlation with Three-Month Postoperative Range of Motion” 12:30 PM Igor Immerman, M.D. “Real-time 2D and 3D MR Imaging During Active Wrist Motion” 12:40 PM Peter D. Rinaldi, D.O. “Effect of Knee Flexion Angle During Medial Patellofemoral Ligament Graft Fixation on Patellofemoral Contact Pressures” 12:50 PM Todd D. Cook, M.D. “Incidence, Risk Factors, and Outcomes of Proximal Junctional Kyphosis in Adult Spinal Deformity Surgery” 1:00 PM Adjournment Derek F. Amanatullah, M.D., Ph.D. Administrative Chief Education B.S. 1998: University of Southern California, Biomedical Engineering M.S. 2001: Albert Einstein College of Medicine, Developmental and Molecular Biology M.D. 2007: Albert Einstein College of Medicine Ph.D. 2007: Albert Einstein College of Medicine, Cellular Biology Next Step Adult Lower Extremity Reconstruction Fellowship, Mayo Clinic, Rochester, MN Career Objective I am dedicated to becoming an internationally recognized surgeonscientist. I am currently looking for an academic surgical practice that will allow me to focus on the surgical management of the arthritic hip and knee as well as pursue the development of new diagnostic and regenerative techniques for degenerative joint disease. Spouse Marirose C. Amanatullah Personal Statement I published 30 peer reviewed manuscripts and 9 non-peer reviewed manuscripts. Eleven additional manuscripts are submitted for publication in peer reviewed journals, and I am in the process of drafting 11 manuscripts based on my current work. I made 31 podium presentations and presented 21 posters at national and international orthopaedic conferences over the last three years. I received numerous awards for my orthopaedic research, including the Sanford and Darlene Anzel Award, Lloyd W. Taylor Resident Award, Vernon Thompson Award, and the J. Harold LaBriola Resident Award. Additionally, I was selected as an International Cartilage Research Society Traveling Clinical Scientist and attended the American Academy of Orthopaedic Surgeons Clinical Scientist Development Program. I served as the editor-in-chief of the Einstein Journal of Biology and Medicine for three years and have recently been invited as a guest editor of Cartilage. I am an active reviewer for numerous journals, including the Journal of the American Academy of Orthopaedic Surgeons, Tissue Engineering, Tissue Engineering and Regenerative Medicine, and Cartilage as well as a resident advisor to the American Journal of Orthopaedics. I served as a voting member of the Continuous Quality Improvement Committee and chair of the Resident Medical Staff Committee at the University of California, Davis as well as a resident liaison to the American Academy of Orthopaedic Surgeons. I am personally interested in intellectual property and am currently involved in the development of four patents. I am personally and professionally indebted to so many. My mentors gave me the tough feedback required to hone my critical thinking and decision making skills. My friends gave me the encouragement required to overcome numerous personal and intellectual hurdles. My family gave me the unconditional love required to become a better person. My parents have endured all 16 years of my training and are the only people who understand the depths of my personal and professional failures and how this forms the foundation of my current success. They have never wavered. They are the bedrock of my life. My wife shares my personal values and professional dreams. She is the love of my life. We are the perfect team poised to build a prosperous and fulfilling life together. Calculating the Position of the Joint Line of the Knee in Relationship to Anatomic Landmarks Derek F. Amanatullah, M.D., Ph.D., Michael J. Alaia, M.D., Kenneth Montini, M.D., Matthew J. Lopez, M.D., Paul E. Di Cesare, M.D., & Gavin C. Pereira, MBBS Restoration of the joint line of the knee during primary and revision total knee arthroplasty is one of many critical steps that directly influence patient outcomes. Fifty MRI scans of normal atraumatic knees were analyzed to determine a quantitative relationship between the joint line of the knee and the bony landmarks of the knee joint: femoral epicondyles, metaphyseal flare of the femur, tibial tubercle, and proximal tibiofemoral joint. The absolute distances of these anatomic landmarks to the joint line of the knee were highly variable due to patient size and gender. In order to negate the effect of size and gender, the ratios of these distances of the joint line of the knee were normalized to the respective bony diameters. The distance of the lateral epicondyle to the joint line of the knee was about one-third the interepicondylar diameter. The distance of the lateral flare of the femur to the joint line of the knee was one-half the interflare diameter. The distance of the tibial tubercle to the joint line of the knee was one-half the diameter of the tibia in the sagittal plane at the level of the tibial tubercle. The distance of the proximal tibio-femoral joint to the joint line of the knee was one-third the diameter of the tibia in the coronal plane at the level of the proximal tibio-femoral joint. The spatial relationship of the joint line of the knee to the femur and tibia was made by calculating ratios across the joint line. The joint line of the knee was halfway between the lateral epicondyle and proximal tibio-fibular joint in the coronal plane. This description supports a simple three-step algorithm allowing orthopaedic surgeons to calculate, instead of estimate, the location of the joint line of the knee. Philbert Y. Huang, M.D., Ph.D. Administrative Chief Education B.S.: Biomedical Engineering, UC San Diego M.D./Ph.D.: Biomedical Engineering, UC Davis Next Step Sports Medicine Fellowship Sports, Orthopedic, And Rehabilitation (SOAR) Medicine Associates Bay Area, CA Career Objective To provide the best patient care through arthroscopy and general orthopaedics in an academic and athletic team setting. Spouse Fiancee Wendy Lee, M.D. Personal Statement The field of medicine and orthopedic surgery has been a long journey of training and is indeed a humbling one. I have been honored to work alongside many brilliant mentors and co-residents at UC Davis. It is truly a privilege to operate, and I have finally come to understand the sometimes difficult, yet rewarding pathway that is residency. I would like to thank my Dad Raymond, sister Mona, and brother Jeffrey for their unending support and hospitality as I would visit home in Southern California during my vacations. I would also like to thank my beautiful fiancé Wendy, who has shown me such love and selflessness for which I would have not been able to get this far and be this happy without you. I dedicate this milestone in my life to the memory of my mother Grace, whose passion, work ethic, and caring made this day possible. Injuries to the PCL Complex and Medial Structures of the Knee: Finite Element Analysis Philbert Huang, M.D., Ph.D., Jamie Dunaway, B.S., Nesrin Sarigul-Klijn, Ph.D., Cassandra Lee, M.D. Introduction: The stability of the knee with regards to posterior tibial translation is afforded by the posterior cruciate ligament (PCL) as well as several medial sided structures. A combined injury of the medial structures of the knee and PCL is less common, and it is unclear whether both or just one of the two structures injured needs to be surgically reconstructed to restore functional stability. The current study involves the construction of a finite element model of the human knee joint in order to determine the effects of posterior cruciate ligament injury on joint kinematics and contact forces. Furthermore, this model aims to provide clinicians with quantitative information when faced with PCL reconstruction decision-making. One objective for this study will be to determine the least amount of tibia and femur length to be included in the model in order to yield accurate results. Another objective will be to determine the necessity of the patella, fibula, meniscofemoral ligaments, and anterolateral and posteromedial bundles of the PCL, which are structures not included in previous knee finite element models. Background: Numerous finite element models of the knee have been accomplished with assumptions and simplifications for modeling ligaments, bone, and cartilage. Each of these biological tissues contains its own set of non-linear, viscoelastic properties, which are not only difficult to determine from experimental data, but are also patientspecific. Therefore, accurately assessing a patient’s knee joint characteristics after a PCL injury without experimental data to compare to requires both an anatomically and physiologically correct model with accurate viscoelastic material properties of included biological tissues. Loading conditions: When comparing varying degrees of flexion/extension of the knee joint, as well as subject position (standing, sitting, or lying down), loading and boundary tolerances on the superior and inferior cross-sections of the femur and tibia will likely not remain constant. Furthermore, the concept of pre-stresses in ligaments must be introduced. Nonlinear springs may be used in the modeling program, as they can hold a pre-stress. It may be assumed that the ligaments are at equilibrium such that they are only exhibiting an elastic response in a resting position. This concept must be addressed in finite element models of the knee, as patients without much femoral loading (e.g. lying down) must have pre-stresses in ligaments to keep the joint stable. Therefore, there must be a resting length for all ligaments, in which strained ligaments will develop strainrate dependent non-linear stress profiles. Normally Excluded biological tissues: Simplifying the knee joint to a model that includes the four major ligaments has been shown to yield reliable data in assessing knee joint stresses. However, when excluding certain ligaments, bone and cartilage may yield stress values and deformations to a point beyond acceptable errors from experimental data. Important tissues to consider modeling in the knee in conjunction with the aforementioned ligaments and cartilage are: the quadriceps tendon, the patella, the patellar ligament, the anterior and posterior mensicofemoral ligaments, and the fibula. Material properties: While properties are patient specific due to physiological responses and age, trabecular bone has been cited to be largely apparent density dependent. Previous studies have shown that bones may be modeled as rigid bodies in order to examine cartilage and other viscoelastic tissue behaviors. However, as this study aims to determine alterations of stresses in bone due to PCL removal, bone must be modeled as a nonrigid, density dependent transversely isotropic material. Methods: The software MIMICS will be utilized to build a model of the knee joint from CT and MRI of a sample patient. The extent of femoral and tibial length utilized in the model is to be determined. Ligaments will be reconstructed using MIMICS, at which there will be little to no gap between bone and ligament contact. A FE model will be built in Abaqus 6.10. Eight node brick elements will be used for all structures unless otherwise stated. The mesh will be developed in Mimics. A finite element model that appropriately incorporates a“novel knee system” that includes all functional structures can help elucidate the role each structure plays in the overall stability of the knee. In this model, the ligaments, menisci, and cartilage can be identified and accurately represented. By modeling and simulating an injury by removing one or more ligaments at a time, the resultant pathologic translations of the tibia with respect to the femur by simulating clinical exams can be determined. In addition, contact forces in the joint and the increase in stresses in the remaining intact ligaments can be determined. The information obtained from this study can then be used towards clinical decisionmaking and patient care for those who have sustained such an injury. Raj S. Kullar, M.D. Administrative Chief Education B.S.: University of California, Davis Biological Sciences M.D.: University of California, Davis Next Step Fellowship – Sports Medicine, University of Utah Sports Medicine Career Objective My career objectives are to provide quality medical care to patients with a smile on my face, and to always leave work knowing that I am doing exactly what I always wanted to do in life. Spouse Jasneet Kullar Personal Statement It brings me great pride and gratitude to be able to say I have completed what I feel is the best residency program in California. What an amazing ride it has really been. I feel so lucky to have learned from such great mentors. Thank you for your patience and willingness to put up with me, even if it was painful at times! Thank you to Margaret, the clinic, operating room staff, and administrative staff for making the last five years an absolute blast. On a more personal note, thanks to my family for always being there for me. I would be nowhere without the constant support of my sisters, brother-in-laws, and parents through undergrad, medical school, and residency. I love you guys, and I hope I am making you proud today. I am also fortunate in that I am clearing two of life’s hurdles in the same year – getting married and completing residency. I truly am excited to see what life has in store. What I do know is that whatever path my professional career takes, I will do it with an amazing woman by my side. I can’t wait to experience that ride with you, Jasneet. Good luck to all the juniors. See you when I see you! The Properties of the Subscapularis Following Repair in Reverse Total Shoulder Arthroplasty: a Cadaveric and Biomechanical Analysis Kullar R, M.D., Anderson M, M.S., Van den Bogaerde JM, M.D. A deltopectoral approach for reverse total shoulder arthroplasty necessitates release of the subscapularis for exposure and implant placement. Recently, some surgeons have begun repairing the subscapularis with thoughts that it may improve internal rotation or it may act as a sling against anterior escape. We sought to evaluate the functional integrity of the subscapularis after reverse shoulder replacement to cyclic and physiologic loads, as well as the anatomic orientation of the muscle after repair. Twelve paired fresh frozen human cadaveric shoulder girdle specimens were dissected of all tissue except the subscapularis. The scapula and humerus were potted in polymethylmethacrylate (PMMA, GC America) with the scapula in neutral abduction and the humerus in neutral rotation, and then mounted to the Instrom. Initial control measurements were obtained to measure the intrinsic tension of the native subscapularis, including a passive test and active tension force with a hooked force. A reverse shoulder was then placed, the subscapularis repaired through drill holes with #2 Fiberwire sutures around the stem. Similar measurements were taken with the reverse shoulder in place. Photographs were taken before and after shoulder replacement to document the location of the subscapularis in relation to the acromion and coracoid. Data analysis showed a statistically significant difference in pull ratio as well as pull stiffness between control and repair groups. There was also a statistically significant difference in passive slope between control and repair groups, indicating a greater tension within the subscapularis muscle. There was no statistically significant difference in passive maximal pull. There was failure of the repair in 3 of 12 specimens. In conclusion, the subscapularis is significantly less functional after reverse TSA, generating significantly less torque and demonstrating higher tension than control levels. Three of twelve repairs failed during testing. Thirdly, the function of the subscapularis as an internal rotator after reverse TSA in physiologic conditions is certainly limited. Lance K. Mitsunaga, M.D. Administrative Chief Education Undergraduate: Stanford University M.D.: UC San Diego School of Medicine Next Step Orthopaedic Spine Surgery Fellowship at Kaiser Permanente Northern California Regional Spine Center in Oakland, CA. Career Objective I hope to do whatever I can as a spine surgeon to affect the lives of my patients and my community for the better. Spouse Mary Tran Personal Statement It is with the utmost pride with which I call myself a graduate of the UC Davis Department of Orthopaedic Surgery Residency Program. When I think about all those who came before me and made this residency program into what it is today, I realize how fortunate I am to be a small part of this tradition. Five years have abruptly come and gone, but the lessons I have garnered here over the years on what it truly means to be a physician, a surgeon, and—perhaps, most importantly—a good man, are immeasurable. To the faculty, staff, and all my teachers, thank you for your patience and the knowledge you have passed on. To my family, I hope I have made you proud and made the most of all your sacrifices. And, to Mary and Cookie, I know the past few years have not always been easy, but you have both stayed faithfully by my side through it all. I have no idea how I’ll ever earn everything you have given to me, but I’ll spend the rest of this life trying. As we say in Hawaii: “A hui hou!” Until we meet again… Can a Universal Protocol for Prevention of Surgical Site Infections Reduce Postoperative Infection Rates to Zero in Spine Surgery Patients? Lance Mitsunaga, M.D., Marko Tomov, MSI, Deepak Nallur, B.S., Blythe Durbin-Johnson, Ph.D., Rolando Roberto, M.D. Background: Surgical site infection (SSI) rates are an important measure of quality in spine surgery. SSIs in spine surgery occur at a predictable rate, varying from less than 1% to more than 10%, depending on various factors. Postoperative SSIs in spine surgery can lead to serious consequences from a patient and socioeconomic standpoint. Recently, wound irrigation with dilute betadine solution and the local application of intra-wound antibiotic powder prior to wound closure have both been described to reduce rates of postoperative spine SSIs. Purpose: The aim of this study was to evaluate the efficacy of a universal protocol combining the use of dilute betadine irrigation solution and intrawound vancomycin powder in the prevention of SSIs after spinal surgery. We hypothesized that implementing this infection prevention protocol would reduce SSI rates in spine surgery patients. We also attempted to determine if there are any patient or surgical characteristics associated with SSIs. Materials and Methods: Effective 1/1/12, all spine surgery patients received the study intervention: Dilute Betadine irrigation (0.3% weight/volume) and one gram of vancomycin powder spread throughout the wound. All spinal surgery cases performed by orthopaedic surgery staff physicians at UCDMC from 2010-2012 were captured by reviewing Health System databases and data from NSQIP (National Surgical Quality Improvement Program). Cases requiring reoperation to treat SSIs were identified using Current Procedural Terminology (CPT) code data. Cases requiring irrigation and debridement with either subsequent positive intraoperative cultures or clinical suspicion were considered SSI cases. A chi-square analysis was performed to compare SSI rates from 2010 and 2011 (prior to implementation of the universal protocol) to those from 2012 (after the protocol was initiated). We also partnered with hospital NSQIP personnel to obtain details of all spine surgery infection cases (as well as noninfected control cases) from UCDMC from the years 2010-2012, including patient demographics/co-morbidities and procedural details. The effect of patient and surgical characteristics on the risk of SSI was first analyzed in a univariate fashion for one patient/ surgical characteristic at a time. Patient/ surgical characteristics with p-values less than 0.05 in this univariate analyses were then included together in a multivariable mixed effects logistic regression model. Results: In 2010-2012, the total number of spinal surgeries performed by UCDMC orthopaedic surgeons was 599, 653, and 693, respectively. The SSI rate for 2010-2011 (prior to implementing our universal protocol) was 2.4%. This was reduced to 1.7% in 2012, after the protocol was initiated (p=.334). In our univariate mixed effects logistic regression analyses, smoking, alcohol use, anemia, dyspnea, coronary artery disease, congestive heart failure, malignancy, coagulopathy, and revision surgery were among the factors individually associated with significantly higher odds of SSI. Posthoc testing showed a significantly higher odds of SSI among patients who had an operation lasting more than 5 hours and those who required a blood transfusion. In our multivariable mixed effects logistic regression analysis, alcohol use, anemia, CAD, and revision surgery were associated with significantly higher odds of SSI. Conclusions: Our study clarified SSI rates in spinal surgery at UCDMC and identified several patient and procedural characteristics associated with SSIs. This is the first step in performing a more accurate preoperative risk assessment for SSIs and to focus measures designed to reduce SSIs. We found that two specific SSI prevention measures in spine surgery—topical irrigation with dilute betadine solution and the simple application of vancomycin powder— have the potential to decrease SSI rates, though we were not able to achieve statistical significance. Daemeon A. Nicolaou, M.D. Administrative Chief Education B. S.: Neuroscience, UCLA 1994 M.D.: University of Michigan Medical School, 2008 Next Step Trauma Fellowship at Univeristy in St. Louis, MO St. Louis Career Objective I would like to operate in a high energy trauma facility specializing in pelvic and acetabular trauma, as well as periarticular fractures, malunions and nonunions. I hope to serve at an institution where the challenges lead to patient care advances as I aspire to teach and continue to learn from my colleagues, teammates, friends as well as, the next generation of Orthopaedic residents. Spouse I haven’t been lucky enough yet Personal Statement I would like to thank first and foremost my family for all of their love and support over these many years. They have always been there supporting me through my many adventures on this long journey. I know that I would have never reached this point in my life without them and I’m sure I don’t say it enough, but I love you all and am so thankful to have you. Dr. Roberto, thank you for always having our backs no matter the cost to yourself. It has not gone unnoticed and is certainly appreciated by all of us. Miss MacNitt, you have been a life saver on so many occasions. You really keep this program and us residents on task from behind the scenes. Thank you!! Dr. Salamon, thank you for giving me the bug to travel to other parts of the world to share our knowledge of Orthopaedics and learn from others. Go Blue!! Dr. Manske, thank you for your zen-like attitude and helping me develop from a resident to a surgeon. Dr. Marder, thank you for showing me how to be a first class physician both in and out of the operating room and making sure I can do an ACL.:) Dr. Hallare, thank you for allowing me the chance to feel like a trauma surgeon. I learned so much in that time and owe you a debt of gratitude. Finally, to my trauma mentors: Drs. Wolinsky, Lee, Ferguson, Yoo and Eastman. I would like to thank you for all of your time and interest in my education and training. I hope to build on the fundamentals you have taught me. You have inspired me with your dedication to excellence, breadth of knowledge and generous disposition to share with all of us. You have set a high bar! I look forward to seeing you all at future events and conferences. You should certainly expect to hear from me as I turn to you for advice about complex cases. :) Comparison in Fatigue Strength of Various Plaster Posterior Short Leg Splint Configurations Daemeon Nicolaou, M.D., Matthew Anderson, B.S., Brad Yoo, M.D. This study looks at the strength of various posterior short leg splint configurations using 15 sheets of plaster of paris splinting material: posterior slab, U-type splint and rebar configuration. Testing was done using the 5800R Instron materials testing machine and cycled to 130N at 0.5 hertz for 10,000 cycles or until failure. The data found no statistical difference between the posterior slab and rebar configurations of splint for cycles to failure, 90.2 and 59.4 respectively, whereas the U-type splint did not fail within 10,000 cycles. From our data, the standard U-type splint is the strongest splint configuration and should be utilized whenever a short leg plaster splint is warranted in fracture care or post-operatively. John David Burrow, D.O. Adult Reconstruction Fellow Education Undergraduate: University of Tennessee at Martin, Martin, TN M.D.: Virgina College of Osteopathic Medicine, Blacksburg, VA Residency: Orthopaedic Surgery, UMDNJ, Stratford, NJ Next Step Associate in Adult Reconstruction, Orthopedic Sports and Spine Newport News, VA Career Objective To fullfill the increasing need for primary arthroplasty and revision arthroplasty in the upcomming years with a skilled knowledge base and continue to seek innovative and progressive ideas in Adult Reconstruction. Spouse Darany Toy, D.O. Personal Statement I would like to thank the department of Orthopaedics at UC Davis as a whole. The knowledge obtained in review of patients and lectureship over the last year will serve as reinforcement for the obstacles to come. Additionally for the department of Adult Reconstruction, I would like to express my gratitude for the knowledge base and variety of treatment options that I was exposed to through the course of the year. I feel that I have encountered a wide range of complex patients and pathology and I am confident that I will make sound decisions for my patient’s based on the knowledge acquired this year. I look forward to a career that will be in high demand even in uncertain medical climate. I will carry the knowledge base acquired this year to better serve my patients and hopefully expand upon this as I evolve through my career. Evaluation of Knee Kinematics in the Sagittal and Coronal Planes in Navigation Assisted Total Knee Arthroplasty and Correlation with Three-Month Postoperative Range of Motion John David Burrow, D.O., Gavin Pereira, M.D., MBBS, FRCS(Eng), FRCS(Orth) Review: Total knee arthroplasty is one of the most preformed Orthopaedic surgeries in the United States with projections to increase four fold over the next 20 years. In general, postoperative range of motion is dependent on a number of factors including preoperative range of motion. Still it is reported that 10-20 % of patients do not achieve complete satisfaction with total knee arthroplasty. Recent studies suggest that the postoperative stiffness may be a result of altered kinematics affecting the postoperative range of motion. Methods: In this retrospective review of 103 patients, 62 patients met the requirements for inclusion utilizing Stryker R navigation by a single surgeon at a single institution, a comparison of pre operative range of motion in flexion and extension, as well as variation of coronal plane from flexion to extension with post operative and a correlation between functional outcome at 3 months in range of motion. The data collected and saved at the beginning of surgery after navigational pins are set and the knee is registered, is the basis of original kinematics of the knee. At the time of finishing the surgery and before removing the trackers, the knee is taken through a final range of motion and this data is collected as well. The pre and post operative data was then compared to the patient postoperative range of motion at the three-month evaluation. Conclusions: The initial kinematics compared to the balance of post implantation kinematics can vary as noted by data collection. It is thought that a significant change in the kinematics may result in less than optimal out comes for patient satisfaction as noted by post operative range of motion. Utilizing Chi square analysis in a population of 62 patients preformed at a single institution by a single surgeon, a p value of 0.00027493 concludes that a statistical difference exists within the data set and is further evaluated by odds ratio to predict expected outcomes. Todd D. Cook, M.D. Spine Fellow Education Undergraduate: University of Georgia, Athens, GA M.D.: George Washington University School of Medicine, Washington, DC Orthopedic Residency: JPS/Tarrant County Hospital System, Fort Worth, TX Next Step Private Practice Spartanburg, SC Spouse Alexis Children Kyle and Aiden Personal Statement I would like to thank everyone at the UC Davis Department of Orthopaedics for their commitment to the education and guidance of the graduating fellows. This year has been challenging but has been, without question, the most fulfilling of my Orthopedic training. I will always be grateful for the Spine Faculty who have shared their wealth of experience and imparted the values necessary to provide extraordinary spine care. Incidence, Risk Factors, and Outcomes of Proximal Junctional Kyphosis in Adult Spinal Deformity Surgery Todd Cook, M.D., Munish Gupta, M.D. Spinal fusion for adult spinal deformity (ASD) is performed to correct sagittal and coronal imbalance , achieve an optimal correction and solid arthrodesis. Proximal junctional kyphosis (PJK) is a postoperative complication caused by postoperative increased junctional stress concentration. The reported incidence of PJK after long fusion constructs for ASD ranges from 25-39%. Previous studies have cited older age, combined anteroposterior fusion, low bone mineral density, fusion to the sacrum, inappropriate global spine alignment, and greater sagittal vertical axis change as risk factors for PJK. Few studies have analyzed long term follow up or clinical outcome data in patients with PJK. The clinical outcome, natural course of PJK, and the risk factors of developing postoperative PJK have not been fully defined. The purpose of this study was to assess the prevalence, natural course, and risk factors of PJK after long instrumented spinal fusion for ASD. A retrospective review of a prospectively collected surgical database was performed. All patients were treated with long instrumented (> 5 levels) fusions and had a minimum of 1-year follow-up. All surgeries were performed at a single institution by the senior author between 2003 and 2012. Inclusion criteria consisted of age older than 21 years at the time of surgery, ASD treated with instrumented spinal fusion at a minimum 5 motion segments, and complete radiographic follow-up. Complete radiographic review required adequate preoperative, postoperative (6–12 wk), and most recent follow-up anteroposterior and lateral 36in. long scoliosis radiographs. The effect of age, sex, BMI, comorbidities, upper instrumented vertebra (UIV) level, UIV instrumentation type, surgery type, global spine alignment (GSA), change in sagittal vertical axis (SVA), incidence of PJK, and clinical relevance of PJK was investigated. Bryon D. Hobby, M.D. Trauma Fellow Education Undergraduate: Concordia College, Moorhead, MN M.D.: University of Washington School of Medicine, Seattle, WA Residency: Orthopaedic Surgery, University of New Mexico, Albuquerque, NM Next Step Assitant Professor, Department of Orthopaedics and Rehabilitation, University of New Mexico, Albuquerque, NM Career Objective I look forward to providing comprehensive orthopaedic care to trauma patients as well as educating residents. Spouse Stephanie Hobby Children Maryn Hobby Personal Statement I would like to thank everyone at University of California Davis Medical Center’s Orthopaedic Department for an excellent fellowship year. I would especially like to thank the Trauma Faculty for sharing their expertise and guidance throughout the year. I look forward to continuing relationships with the faculty here and am excited to use my experiences from my fellowship year in my practice in New Mexico. Igor Immerman, M.D. Hand Fellow Education Undergraduate: Johns Hopkins University, Baltimore, M.D. M.D.: Case Western Reserve University, Cleveland, OH Residency: NYU Hospital for Joint Diseases, New York, NY Next Step A year of traveling together with my wife in Israel and Russia. I plan on spending time at academic Hand Surgery departments in Jerusalem, Moscow, and Saint Petersburg. Career Objective Academic practice focused on the Upper Extremity and Hand Surgery Spouse Olesya Shayduk-Immerman Personal Statement I wish to thank the entire faculty of the Department of Orthopaedic surgery for the wonderfully educational experience of the past year. I also want to thank all the hardworking residents of the department – it has been a pleasure learning with you, and from you. Above all, I wish to thank my mentor Dr Szabo, and the members of the Hand Surgery faculty – Drs Allen, James, and Bauer, for your teaching, guidance, and mentorship. Your lessons will remain with me throughout my career, and I hope that you can continue to be my mentors and advisors for years to come. Real-time 2D and 3D MR Imaging During Active Wrist Motion Igor Immerman, M.D., Robert D. Boutin, M.D., Michael H. Buonocore, M.D., Ph.D., Zachary Ashwell, Robert M. Szabo, M.D., M.P.H., and Abhijit J. Chaudhari, Ph.D. Hypothesis: Rapid magnetic resonance imaging (Active-MRI) protocol can be utilized to evaluate the wrist during realtime active motion, and the resulting images enable measurement of metrics typically evaluated in the setting of wrist instability. Methods: A 3T MR protocol utilizing a balanced steady-state free precession (bSSFP) pulse sequence (TrueFISP, Siemens Healthcare, Inc.) was developed for imaging the wrist at a single plane during active movement, with 0.94mm x 0.94mm in-plane spatial resolution, 6mm slice thickness, and temporal resolution of 475ms per image (2D Active-MRI). To measure motion parameters that occurred out of the single plane, novel real-time 3T MRI protocols were developed, utilizing another bSSFP sequence (FIESTA, GE Healthcare, Inc.) in 3D acquisition mode. Volumetric data was obtained during active motion, in different scans providing the following isotropic spatial and temporal resolutions: 1.2mm and 5.03s; 1.6mm and 2.95s, 2.0mm and 2.12s (3D Active-MRI). Fifteen wrists of asymptomatic volunteers were scanned with 2D Active-MRI, and four wrists of asymptomatic volunteers were scanned with 3D Active-MRI protocols. Specifics of evaluated motions and measurements are shown in Figure 1. All measurements were performed by consensus of two experienced observers (fellowship-trained musculoskeletal radiologist and an orthopedic hand surgeon) in neutral and at the maximal endpoints of the range of motion. Results: The real-time 2D Active-MRI imaging protocol allowed measurements of parameters in the single plane of the examined wrist motion (see Table 1). 3D volume rendering was able to show out-of-plane movement and allowed more precise measurements. Ulnar variance was only measured in one wrist. In pronation, neutral, and supination UV was -1mm, -2mm, and -4mm, respectively. The SL and CL angles were measured in radial/ulnar deviation in 4 wrists. The mean SL angles in ulnar deviation, neutral, and radial deviation were 600, 720, and 680, respectively. The mean CL angles in ulnar deviation, neutral, and radial deviation were 00, 130(volar), and 20(dorsal), respectively. Summary Points: • High resolution real-time 2D single plane and 3D volumetric MR images of the wrist can be successfully acquired during active wrist motion with negligible artifacts. • Active-MRI can be successfully used to obtain objective information relevant to wrist mechanics and instability with no radiation exposure. • Active-MRI of the wrist is much faster than routine “static” 2D and 3D MR imaging, and may assist in a physiologic and functional imaging evaluation. Figure 1 – Images obtained and parameters measured during active wrist motion ECU – extensor carpi ulnaris; DRUJ – distal radioulnar joint; SL – scapholunate; CL – capitolunate; RL - radiolunate Table I: Quantitative metrics derived from 2D motion-MRI images of the wrist during the different maneuvers. * One volunteer unable to complete the pronation/supination motion protocol ** DRUJ Subluxation ratio, as described by Park et al, JBJS(Am) 2008 *** The wrist harness limited the ability for achieving the full range of volarflexion in a subset of volunteers therefore measurements for volarflexion are not reported. Thu-Ba LeBa, M.D. Pediatric Fellow Education Undergraduate: Cornell University, Ithaca, NY Graduate: Columbia University, New York, NY M.D.: Tulane University, New Orleans, LA Residency: Orthopedic Surgery, UTMB, Galveston, TX Next Step Pediatric Orthopaedic Surgeon Department of Orthopaedic Surgery Children’s Hospital of Central California Madera, California Spouse Brandon Vo Personal Statement This past year has been a fantastic year of learning and growth for me. I would like to thank all my mentors at the Shrine and at UC Davis for their continued teaching, guidance, and encouragement. As I start the next stage of my career, I aim to put forth all that you have taught me about being a compassionate doctor and a skilled surgeon. I know our relationship will continue to grow in the coming years, as I will only be “down the road,” and I look forward to it. Scar Recurrence After Excision in the Pediatric Population Thu-Ba LeBa, M.D., Kevin Diaz, B.S., Samuel Adams, M.D., Jon Davids, M.D. The purpose of this study is to determine the recurrence of scars after excision at the time of revision surgery in the pediatric orthopaedic population. Children often undergo hardware removal. Reasons for removal may be for resumption of normal growth or for lessening the difficulty of removal later on due to bone overgrowth. However, it is unclear how the previous scars should be addressed. Assessment of scar healing has been addressed in the burn and plastics literature, but not in orthopaedic surgery. This was a prospective study of 37 patients undergoing 58 hardware removals from the tibia or femur. Patients were examined preoperative, at 6 months and at 12 months post surgery. Photographs of the scars were taken at each visit. The decision to revise the scar was made by the surgeon at the time of the surgery. At each clinical visit, a questionnaire with a visual analog scale was completed to assess the patient’s satisfactory of the scar. Objective assessment of the scar was performed by 2 orthopaedic surgeons and a medical student using the Stony Brook Scar Evaluation Scale. The hypotheses of the study include: 1) the Stony Brook Scar Evaluation Scale can be used as a preoperative modality to determine the necessity of scar revision; 2) Revised scars have a better appearance at one year after surgery compared to the preoperative appearance; and 3) Scars that are deemed not necessary to revise (having a midline incision) are no worse at one year after surgery than before surgery. Peter D. Rinaldi, D.O. Sports Fellow Education Undergraduate: Eastern Washington University, Cheney, WA M.D.: Touro University College of Osteopathic Medicine, Mare Island, CA Residency: Orthopaedic Surgery, Riverside County Regional Medical Center, Moreno Valley, CA Next Step Currently interviewing for a private practice position in Sacramento Career Objective I would like to build on my experience through residency and fellowship for a few years before seeking a teaching position at an orthopaedic residency program. Spouse Caroline Rinaldi Personal Statement I feel very blessed to have had the opportunity to complete my Fellowship here as part of the UC Davis Department of Orthopaedic Surgery. It is impossible to measure the influence of a mentor on one’s development as a surgeon, especially considering the thousands of patients over the course of a career who subsequently benefit from that influence. I would like to thank the Sports Medicine Faculty for your dedication, wisdom and technical instruction as you served as mentors to me this year. I believe that the excellence of this department is derived from its Faculty leadership and that is manifested in the quality of Residents selected to train at UCD. The residents here are a great group and I am grateful to them for enriching my learning experience. I hope I was able to contribute equally to your development as you did to mine. Thank you also to the Orthopaedic Department, Same Day Surgery Center & J-Street clinic staff who made my days here so enjoyable. If I can deliver the same quality of care with the personal touch that is the standard here, my career will undoubtedly be successful as measured by many healthy and satisfied patients. Effect of Knee Flexion Angle During Medial Patellofemoral Ligament Graft Fixation on Patellofemoral Contact Pressures Richard A. Marder, M.D.; Peter Rinaldi, D.O.; Matthew Anderson, M.S. Medial patellofemoral ligament reconstruction has been a popular topic in the orthopaedic literature of late. There are numerous techniques with several graft options, fixation methods and points of fixation described. A PubMed search for “medial patellofemoral ligament reconstruction” returned 230 articles reflecting an increase of 10 articles in one month’s time. Recently, there have been a number of articles highlighting the complications encountered after MPFL reconstruction. Published complication rates range from 15 to 20 percent overall, with complications requiring reoperation including patellofemoral arthrosis, pain and decreased range of motion in addition to recurrent patellar instability. The purpose of this study is to determine the optimal degree of knee flexion at which to position the knee during MPFL graft tightening and fixation to minimize joint contact pressures during a flexionextension arc. In this biomechanical study, we placed force transducers in the subchondral bone of each cadaveric specimen’s medial and lateral patellar facets. The knees were cycled through a range of motion, analyzing the resultant patellar contact pressures after fixation of the MPFL graft with the knee at zero, 15, 30 and 60 degrees of flexion, respectively. By minimizing contact pressure felt at the articular surface, postoperative pain, arthrosis, motion deficits and resultant need for additional surgery could be reduced. David L. Rothberg, M.D. Trauma Fellow Education Undergraduate: Oregon State University, Corvallis, OR M.D.: University of North Dakota, Grand Forks, ND Residency: University of Utah, Salt Lake City, UT Next Step Assistant Professor, Department of Orthopaedics, University of Utah, Salt Lake City, UT Career Objective University Orthopaedic Trauma Spouse Suzanne O’Rourke Rothberg Children Evelyn Birdie Rothberg Personal Statement I would like to thank the UC Davis Department of Orthopaedics for the opportunity to train in the Trauma Division. This has been an invaluable year of learning that I will use for the rest of my career and I am very grateful and honored to have been here. Posterior Facet Cartilage Injury in Operatively Treated Intraarticular Calcaneus Fractures David L. Rothberg, M.D., Bryon D. Hobby, M.D., Brad J. Yoo, M.D. Objective: To investigate the incidence of posterior facet articular injury in joint depression calcaneus fractures treated with open reduction internal fixation. The location, size, and depth of the articular injury will also be examined. Design: Prospective, Cohort Study Observational Setting: Regional Trauma Center (Level 1) Participants: A single surgeon series of 28 patients with 29 joint depression intraarticular calcaneus fractures. Intervention: Intra-operative, observational data collection. Main Outcome Measures: Patient demographic and injury data, radiographic fracture characterization, and intraoperative observation of articular injury size, depth, and location will be recorded. Observations will be correlated with the OTA and Sanders classification systems. Results: Age, sex, mechanism of injury, and depth and location of cartilage injury are not significantly different between the 14 OTA/Sanders type 2 and 15 type 3 DIACF’s evaluated in this study (p > 0.05). Posterior facet articular cartilage delamination is found in 79% of type 2 and 100% of type 3 fractures (p = 0.10). Location of cartilage injury is commonly (48%) along the distal, lateral aspect of the posterior facet (p = 0.002). The percentage area of cartilage injury is significantly larger in type 3 fractures (3.1%) then type 2 (1.3%) (p = 0.02). Conclusions: DIACF’s have a consistent location of posterior facet articular cartilage delamination along the distal lateral aspect of the osteo-articular fragment. This lesion is larger in OTA/ Sanders classification type 3 fractures compared to type 2 fractures.