Letter to the Editor Williams Syndrome Cognitive Profile Also Characterizes Velocardiofacial/DiGeorge Syndrome
advertisement
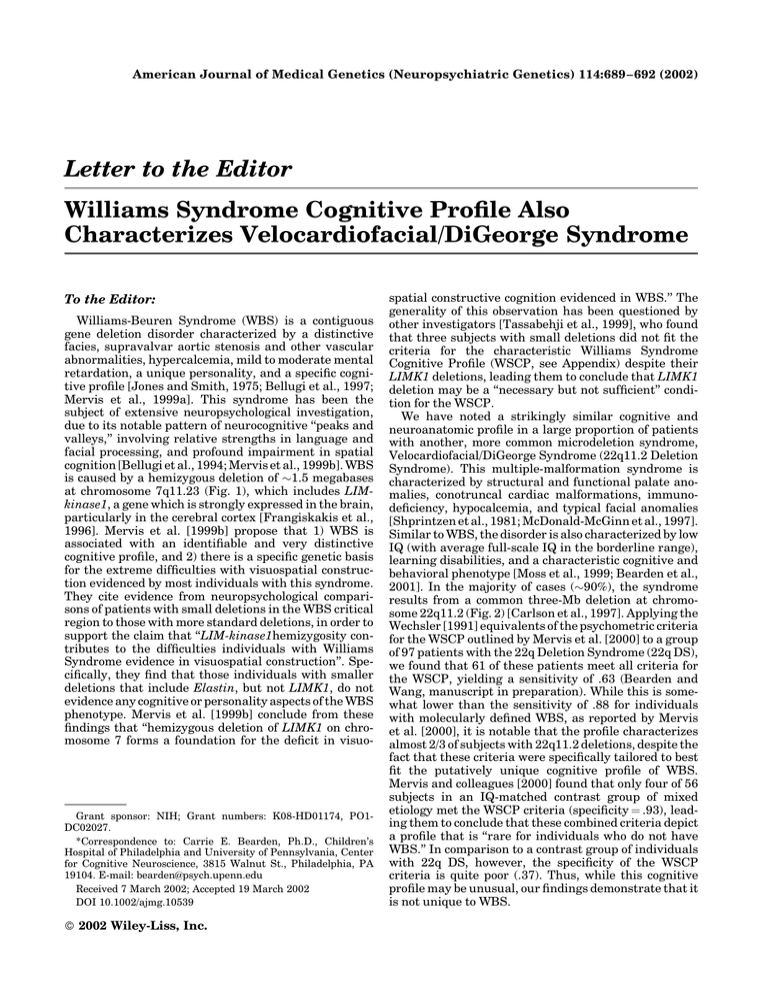
American Journal of Medical Genetics (Neuropsychiatric Genetics) 114:689– 692 (2002) Letter to the Editor Williams Syndrome Cognitive Profile Also Characterizes Velocardiofacial/DiGeorge Syndrome To the Editor: Williams-Beuren Syndrome (WBS) is a contiguous gene deletion disorder characterized by a distinctive facies, supravalvar aortic stenosis and other vascular abnormalities, hypercalcemia, mild to moderate mental retardation, a unique personality, and a specific cognitive profile [Jones and Smith, 1975; Bellugi et al., 1997; Mervis et al., 1999a]. This syndrome has been the subject of extensive neuropsychological investigation, due to its notable pattern of neurocognitive ‘‘peaks and valleys,’’ involving relative strengths in language and facial processing, and profound impairment in spatial cognition [Bellugi et al., 1994; Mervis et al., 1999b]. WBS is caused by a hemizygous deletion of !1.5 megabases at chromosome 7q11.23 (Fig. 1), which includes LIMkinase1, a gene which is strongly expressed in the brain, particularly in the cerebral cortex [Frangiskakis et al., 1996]. Mervis et al. [1999b] propose that 1) WBS is associated with an identifiable and very distinctive cognitive profile, and 2) there is a specific genetic basis for the extreme difficulties with visuospatial construction evidenced by most individuals with this syndrome. They cite evidence from neuropsychological comparisons of patients with small deletions in the WBS critical region to those with more standard deletions, in order to support the claim that ‘‘LIM-kinase1hemizygosity contributes to the difficulties individuals with Williams Syndrome evidence in visuospatial construction’’. Specifically, they find that those individuals with smaller deletions that include Elastin, but not LIMK1, do not evidence any cognitive or personality aspects of the WBS phenotype. Mervis et al. [1999b] conclude from these findings that ‘‘hemizygous deletion of LIMK1 on chromosome 7 forms a foundation for the deficit in visuo- Grant sponsor: NIH; Grant numbers: K08-HD01174, PO1DC02027. *Correspondence to: Carrie E. Bearden, Ph.D., Children’s Hospital of Philadelphia and University of Pennsylvania, Center for Cognitive Neuroscience, 3815 Walnut St., Philadelphia, PA 19104. E-mail: bearden@psych.upenn.edu Received 7 March 2002; Accepted 19 March 2002 DOI 10.1002/ajmg.10539 ! 2002 Wiley-Liss, Inc. spatial constructive cognition evidenced in WBS.’’ The generality of this observation has been questioned by other investigators [Tassabehji et al., 1999], who found that three subjects with small deletions did not fit the criteria for the characteristic Williams Syndrome Cognitive Profile (WSCP, see Appendix) despite their LIMK1 deletions, leading them to conclude that LIMK1 deletion may be a ‘‘necessary but not sufficient’’ condition for the WSCP. We have noted a strikingly similar cognitive and neuroanatomic profile in a large proportion of patients with another, more common microdeletion syndrome, Velocardiofacial/DiGeorge Syndrome (22q11.2 Deletion Syndrome). This multiple-malformation syndrome is characterized by structural and functional palate anomalies, conotruncal cardiac malformations, immunodeficiency, hypocalcemia, and typical facial anomalies [Shprintzen et al., 1981; McDonald-McGinn et al., 1997]. Similar to WBS, the disorder is also characterized by low IQ (with average full-scale IQ in the borderline range), learning disabilities, and a characteristic cognitive and behavioral phenotype [Moss et al., 1999; Bearden et al., 2001]. In the majority of cases (!90%), the syndrome results from a common three-Mb deletion at chromosome 22q11.2 (Fig. 2) [Carlson et al., 1997]. Applying the Wechsler [1991] equivalents of the psychometric criteria for the WSCP outlined by Mervis et al. [2000] to a group of 97 patients with the 22q Deletion Syndrome (22q DS), we found that 61 of these patients meet all criteria for the WSCP, yielding a sensitivity of .63 (Bearden and Wang, manuscript in preparation). While this is somewhat lower than the sensitivity of .88 for individuals with molecularly defined WBS, as reported by Mervis et al. [2000], it is notable that the profile characterizes almost 2/3 of subjects with 22q11.2 deletions, despite the fact that these criteria were specifically tailored to best fit the putatively unique cognitive profile of WBS. Mervis and colleagues [2000] found that only four of 56 subjects in an IQ-matched contrast group of mixed etiology met the WSCP criteria (specificity ¼ .93), leading them to conclude that these combined criteria depict a profile that is ‘‘rare for individuals who do not have WBS.’’ In comparison to a contrast group of individuals with 22q DS, however, the specificity of the WSCP criteria is quite poor (.37). Thus, while this cognitive profile may be unusual, our findings demonstrate that it is not unique to WBS. 690 Bearden et al. Fig. 1. Map of typical !1.5 Mb Williams syndrome deletion region (figure courtesy of M. Tassabehji). Other neurogenetic disorders (e.g., Turner syndrome, Fragile X) have a similar pattern of cognitive abilities, involving deficits in arithmetic and visuospatial abilities, with a relative strength in rote verbal memory [Reiss et al., 2000a; Kwon et al., 2001]. This pattern is commonly referred to as a ‘‘Nonverbal Learning Disorder’’ [Rourke, 1995]. In the case of Fragile X syndrome, the characteristic cognitive impairments have been attributed to the absence of the FMR1 gene product (FMRP) in neurons, resulting in abnormal morphology of dendritic spines and a reduction in the length of synapses in the cortex [Rudelli et al., 1985; Hinton et al., 1991]. Turner syndrome, a genetic disorder characterized by partial or complete absence of one of the two X chromosomes in a phenotypic female, is also characterized neuropsychologically by deficits in visualspatial/perceptual skills and attention [Pennington et al., 1985; Olney and Schaefer, 1998]. While the molecular etiology of these cognitive deficits is incompletely understood in Turner syndrome, an MRI study of females with this disorder found decreased proportional volumes primarily in the region of the parietal lobe, an area known to be linked to visuospatial function [Reiss et al., 1995]. Several studies have described a characteristic neuroanatomy of WBS, suggesting a possible underlying pathophysiology for the cognitive deficits. Gross anatomical findings in WBS consist mainly of overall volume reduction, with curtailment in the posterior-parietal and occipital regions [Galaburda and Bellugi, 2000; Reiss et al., 2000b]. Notably, similar volumetric reductions in parietal and occipital brain regions have been noted in the 22q DS population [Eliez et al., 2000; Kates et al., 2001]. Thus, it is important to examine candidate neurodevelopmental genes in the 22q11.2 region that might have similar effects. Goosecoid-like (GSCL) is one Fig. 2. Map of typical !3 Mb Velocardiofacial/DiGeorge syndrome deletion region (figure courtesy of B.S. Emanuel). potential candidate; this gene in the 22q11 region is expressed early during embryogenesis in a limited number of tissues [Gottlieb et al., 1997], and has been hypothesized to be responsible for abnormal development of posterior brain regions in 22q DS [Eliez et al., 2001]. However, one notable difference between the characteristic neuroanatomy of WBS as compared to 22q DS is that subjects with Williams syndrome have been reported to have significant increases in the volume of the posterior vermis and the neocerebellar hemispheres relative to normal controls [Jernigan et al., 1993; Wang and Bellugi, 1993], while 22q DS subjects show decreased volumes in cerebellar regions concomitant with parietal—occipital reduction [Eliez et al., 2000]. While subjects with WBS tend to be unusually socially outgoing and overly friendly [Jones et al., 2000], subjects with 22q DS are often described as withdrawn [Swillen et al., 1999] or as having flat affect [Bassett et al., 1998], and have an elevated incidence of autisticspectrum diagnoses [Niklasson et al., 2001]. In addition, subjects with both Fragile X and Joubert syndrome also typically possess social and communication problems resembling autistic behavior [Cohen et al., 1991; Holroyd et al., 1991], and these disorders have both have been shown to have decreased cerebellar vermal areas [Holroyd et al., 1991; Guerreiro et al., 1998]. Thus, comparison of neurogenetic disorders with prominent affective components suggests that there may be a possible relationship between posterior vermis size and level of social drive. In summary, while the cognitive and neuroanatomic profiles of WBS do indeed make it a compelling model for elucidating complex gene-brain-behavior relationships, cross-syndrome comparisons can isolate candidate genes which may have similar distal effects on brain development, resulting in similar neurocognitive patterns. Thus, we argue that 1) the ‘‘Williams syndrome cognitive profile’’ is not unique, and 2) the putative effects of hemizygous LIM-kinase1 deletion on cognition and neuroanatomy are non-specific. Rather, LIMK1 may have similar effects on neural development as other candidate neurodevelopmental genes, and hemizygosity for any of these genes may result in a final common pathway of anomalous brain development, which is the underlying basis of this characteristic cognitive profile. While we fully agree with Mervis et al. [2000] in their conclusion that ‘‘this research demonstrates the importance of systematic phenotypic methods . . . to the efficient search for associations between behavior and genotype,’’ we would like to highlight the additional point that comparison not only across domains, but across syndromes, is Letter to the Editor critical to determine both the unique and shared effects of particular genes on brain and cognition. ACKNOWLEDGMENTS Dr. Elaine Zackai, Dr. Beverly Emanuel, and Donna McDonald-McGinn are gratefully acknowledged for their support. APPENDIX Criteria for WSCP [from Mervis et al., 2000]1 1. Pattern-Construction T score < mean T score for core subtests 2. Pattern-Construction T score < Digit-recall T score 3. Pattern-Construction T score < 20th percentile 4. T-score for either Digit Recall, Naming/Definitions, or Similarities, > 1st percentile Additional Criteria 1. Digit Recall T score > mean T score 2. Naming/Definitions T score > Pattern-Construction T score 3. Similarities T score > Pattern-Construction T score REFERENCES Bassett AS, Hodgkinson K, Chow EW, Correia S, Scutt LE, Weksberg R. 1998. 22q11 deletion syndrome in adults with schizophrenia. Am J Med Genet 81:328–337. Bearden CE, Woodin M, Wang PP, Moss E, McDonald-McGinn D, Zackai E, Cannon TD. 2001. Neuropsychological function in the chromosome 22 deletion syndrome: selective deficit in visual-spatial memory. J Clin Exp Neuropsychol 23:447–464. Bellugi U, Wang PP, Jernigan TL. 1994. Williams syndrome: an unusual neuropsychological profile. In: Broman SH, Grafman J, editors. Atypical cognitive deficits in developmental disorders: implications for brain function. Hillsdale, NJ: Lawrence Erlbaum Associates. p 23– 56. Bellugi U, Klima ES, Wang PP. 1997. Cognitive and neural development: clues from genetically based syndromes. In: Magnusson D, editor. The lifespan development of individuals: behavioral, neurobiological, and psychosocial perspectives: a synthesis. New York, NY: Cambridge University Press. p 223–243. Carlson C, Sirotkin H, Pandita R, Goldberg R, McKie J, Wadey R, Patanjali SR, Weissman SM, Anyane-Yeboa K, Warburton D, Scambler P, Shprintzen R, Kucherlapati R, Morrow BE. 1997. Molecular definition of 22q11 deletions in 151 velo-cardio-facial syndrome patients. Am J Hum Genet 61:620–629. Cohen IL, Sudhalter V, Pfadt A, Jenkins EC, Brown WT, Vietze PM. 1991. Why are autism and the fragile-X syndrome associated? Conceptual and methodological issues. Am J Hum Genet 48:195–202. Eliez S, Schmitt JE, White CD, Reiss AL. 2000. Children and adolescents with velocardiofacial syndrome: a volumetric MRI study. Am J Psychiatry 157:409–415. Eliez S, Schmitt JE, White CD, Wellis VG, Reiss AL. 2001. A quantitative MRI study of posterior fossa development in velocardiofacial syndrome. Biol Psychiatry 49:540–546. 691 Frangiskakis JM, Ewart AK, Morris CA, Mervis CB, Bertrand J, Robinson BF, Klein BP, Ensing GJ, Everett LA, Green ED, Proschel C, Gutowski NJ, Noble M, Atkinson DL, Odelberg SJ, Keating MT. 1996. LIMkinase1 hemizygosity implicated in impaired visuospatial constructive cognition. Cell 86:59–69. Galaburda AM, Bellugi U. 2000. V. Multi-level analysis of cortical neuroanatomy in Williams syndrome. J Cogn Neurosci 12:74–88. Gottlieb S, Emanuel BS, Driscoll DA, Sellinger B, Wang Z, Roe B, Budarf ML. 1997. The DiGeorge syndrome minimal critical region contains a goosecoid-like (GSCL) homeobox gene that is expressed early in human development. Am J Hum Genet 60:1194–1201. Guerreiro MM, Camargo EE, Kato M, Marques-de-Faria AP, Ciasca SM, Guerreiro CA, Netto JR, Moura-Ribeiro MV. 1998. Fragile X syndrome. Clinical, electroencephalographic and neuroimaging characteristics. Arq Neuropsiquiatr 56:18–23. Hinton VJ, Brown WT, Wisniewski K, Rudelli RD. 1991. Analysis of neocortex in three males with the fragile X syndrome. Am J Med Genet 41:289–294. Holroyd S, Reiss AL, Bryan RN. 1991. Autistic features in Joubert syndrome: a genetic disorder with agenesis of the cerebellar vermis. Biol Psychiatry 29:287–294. Jernigan TL, Bellugi U, Sowell E, Doherty S, Hesselink JR. 1993. Cerebral morphologic distinctions between Williams and Down syndromes. Arch Neurol 50:186–191. Jones KL, Smith DW. 1975. The Williams elfin facies syndrome. A new perspective. J Pediatr 86:718–723. Jones W, Bellugi U, Lai Z, Chiles M, Reilly J, Lincoln A, Adolphs R. 2000. II. Hypersociability in Williams syndrome. J Cogn Neurosci 12:30–46. Kates WR, Burnette CP, Jabs EW, Rutberg J, Murphy AM, Grados M, Geraghty M, Kaufmann WE, Pearlson GD. 2001. Regional cortical white matter reductions in velocardiofacial syndrome: a volumetric MRI analysis. Biol Psychiatry 49:677–684. Kwon H, Menon V, Eliez S, Warsofsky IS, White CD, Dyer-Friedman J, Taylor AK, Glover GH, Reiss AL. 2001. Functional neuroanatomy of visuospatial working memory in fragile X syndrome: relation to behavioral and molecular measures. Am J Psychiatry 158:1040–1051. McDonald-McGinn DM, LaRossa D, Goldmuntz E, Sullivan K, Eicher P, Gerdes M, Moss E, Wang P, Solot C, Schultz P, Lynch D, Bingham P, Keenan G, Weinzimer S, Ming JE, Driscoll D, Clark BJ 3rd, Markowitz R, Cohen A, Moshang T, Pasquariello P, Randall P, Emanuel BS, Zackai EH. 1997. The 22q11.2 deletion: screening, diagnostic workup, and outcome of results; report on 181 patients. Genet Test 1:99–108. Mervis CB, Morris CA, Bertrand J, Robinson BF. 1999a. Williams syndrome: findings from an integrated program of research. In: Tager-Flusberg H, editor. Vol. Neurodevelopmental disorders. Developmental cognitive neuroscience. Cambridge, MA: MIT Press. p 65–110. Mervis CB, Robinson BF, Pani JR. 1999b. Visuospatial construction. Am J Hum Genet 65:1222–1229. Mervis CB, Robinson BF, Bertrand J, Morris CA, Klein-Tasman BP, Armstrong SC. 2000. The Williams syndrome cognitive profile. Brain Cogn 44:604–628. Moss EM, Batshaw ML, Solot CB, Gerdes M, McDonald-McGinn DM, Driscoll DA, Emanuel BS, Zackai EH, Wang PP. 1999. Psychoeducational profile of the 22q11.2 microdeletion: a complex pattern [see comments]. J Pediatr 134:193–198. Niklasson L, Rasmussen P, Oskarsdottir S, Gillberg C. 2001. Neuropsychiatric disorders in the 22q11 deletion syndrome. Genet Med 3:79–84. Olney AH, Schaefer GB. 1998. Turner syndrome. Ear Nose Throat J 77:812. Pennington BF, Heaton RK, Karzmark P, Pendleton MG, Lehman R, Shucard DW. 1985. The neuropsychological phenotype in Turner syndrome. Cortex 21:391–404. Reiss AL, Freund LS, Baumgardner TL, Abrams MT, Denckla MB. 1995. Contribution of the FMR1 gene mutation to human intellectual dysfunction. Nat Genet 11:331–334. 1 Mervis et al. [2000] employed the Differential Abilities Scale (DAS) as their primary cognitive assessment measure, whereas we administered the Wechsler Intelligence Scale for Children (WISC-III, 3rd edition). The DAS subtests (Pattern-Construction, Digit Recall, Naming/Definitions, and Similarities) were designed to be analogous to the Wechsler tests, and are highly correlated with the respective WISC-III measures (Block Design, Digit Span, Vocabulary, and Similarities, respectively). Reiss AL, Eliez S, Schmitt JE, Patwardhan A, Haberecht M. 2000a. Brain imaging in neurogenetic conditions: realizing the potential of behavioral neurogenetics research. Ment Retard Dev Disabil Res Rev 6:186–197. Reiss AL, Eliez S, Schmitt JE, Straus E, Lai Z, Jones W, Bellugi U. 2000b. IV. Neuroanatomy of Williams syndrome: a high-resolution MRI study. J Cogn Neurosci 12:65–73. Rourke BP. 1995. Syndrome of nonverbal learning disabilities: neurodevelopmental manifestations. New York, NY: Guilford Press. p 1–50. 692 Bearden et al. Rudelli RD, Brown WT, Wisniewski K, Jenkins EC, Laure-Kamionowska M, Connell F, Wisniewski HM. 1985. Adult fragile X syndrome. Cliniconeuropathologic findings. Acta Neuropathol (Berl) 67:289–295. Shaikh TM, Kurahashi H, Saitta SC, Hu P, Roe BA, Driscoll DA, McDonaldMcGinn DM, Zackai EH, Budarf ML, Emanuel BS. 2000. Chromosome 22specific low copy repeats and the 22q11.2 deletion syndrome: genomic organization and deletion endpoint analysis. Hum Mol Genet 9:489–501. Wang PP, Bellugi U. 1993. Williams syndrome, Down syndrome, and cognitive neuroscience. Am J Dis Child 147:1246–1251. Wechsler D. 1991. Wechsler intelligence scale for children. 3rd ed. San Antonio, TX: The Psychological Corporation. Shprintzen RJ, Goldberg RB, Young D, Wolford L. 1981. The velo-cardiofacial syndrome: a clinical and genetic analysis. Pediatrics 67:167–172. Swillen A, Devriendt K, Legius E, Prinzie P, Vogels A, Ghesquiere P, Fryns JP. 1999. The behavioural phenotype in velo-cardio-facial syndrome (VCFS): from infancy to adolescence. Genet Couns 10:79–88. Tassabehji M, Metcalfe K, Karmiloff-Smith A, Carette MJ, Grant J, Dennis N, Reardon W, Splitt M, Read AP, Donnai D. 1999. Williams syndrome: use of chromosomal microdeletions as a tool to dissect cognitive and physical phenotypes. Am J Hum Genet 64:118–125. Carrie E. Bearden* Paul P. Wang Tony J. Simon Department of Child Development The Children’s Hospital of Philadelphia Philadelphia, Pennsylvania