Document 13180144
advertisement
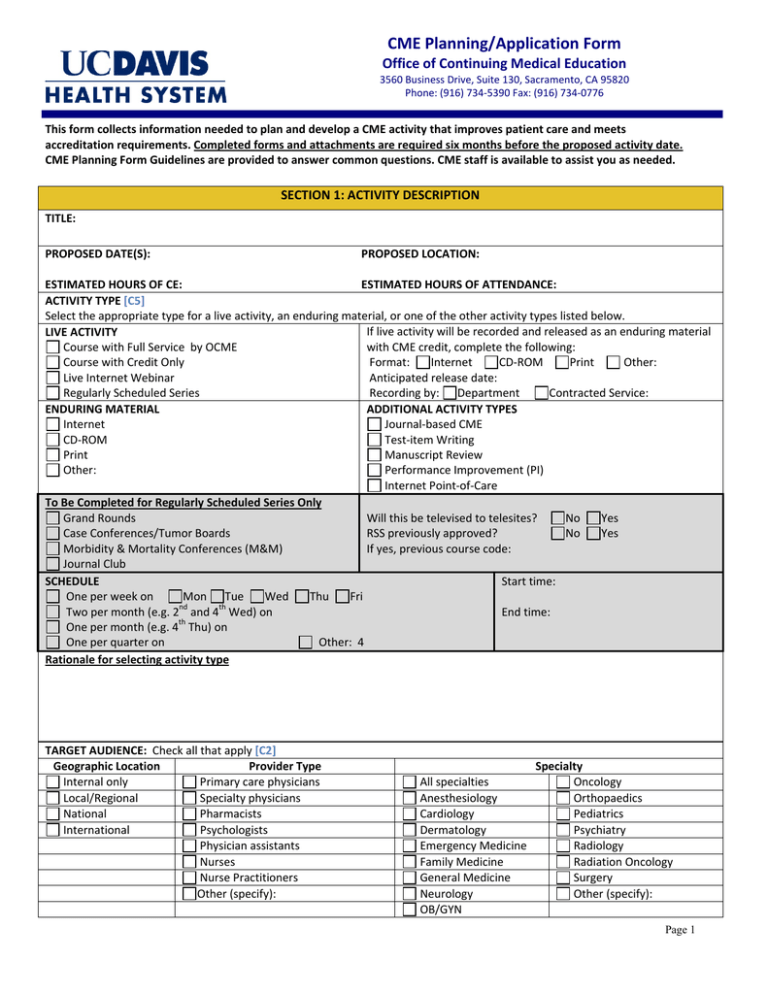
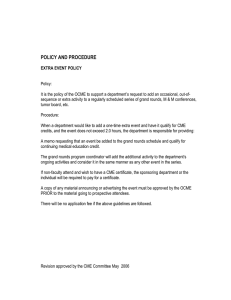
CME Planning/Application Form Office of Continuing Medical Education 3560 Business Drive, Suite 130, Sacramento, CA 95820 Phone: (916) 734-5390 Fax: (916) 734-0776 This form collects information needed to plan and develop a CME activity that improves patient care and meets accreditation requirements. Completed forms and attachments are required six months before the proposed activity date. CME Planning Form Guidelines are provided to answer common questions. CME staff is available to assist you as needed. SECTION 1: ACTIVITY DESCRIPTION TITLE: PROPOSED DATE(S): PROPOSED LOCATION: ESTIMATED HOURS OF CE: ESTIMATED HOURS OF ATTENDANCE: ACTIVITY TYPE [C5] Select the appropriate type for a live activity, an enduring material, or one of the other activity types listed below. If live activity will be recorded and released as an enduring material LIVE ACTIVITY with CME credit, complete the following: Course with Full Service by OCME Course with Credit Only Internet CD-ROM Print Other: Format: Live Internet Webinar Anticipated release date: Regularly Scheduled Series Contracted Service: Recording by: Department ADDITIONAL ACTIVITY TYPES ENDURING MATERIAL Internet Journal-based CME CD-ROM Test-item Writing Print Manuscript Review Other: Performance Improvement (PI) Internet Point-of-Care To Be Completed for Regularly Scheduled Series Only Grand Rounds Will this be televised to telesites? No Yes Case Conferences/Tumor Boards RSS previously approved? No Yes Morbidity & Mortality Conferences (M&M) If yes, previous course code: Journal Club SCHEDULE Start time: One per week on Mon Tue Wed Thu Fri Two per month (e.g. 2nd and 4th Wed) on End time: One per month (e.g. 4th Thu) on One per quarter on Other: 4 Rationale for selecting activity type TARGET AUDIENCE: Check all that apply [C2] Geographic Location Provider Type Internal only Primary care physicians Local/Regional Specialty physicians National Pharmacists International Psychologists Physician assistants Nurses Nurse Practitioners Other (specify): All specialties Anesthesiology Cardiology Dermatology Emergency Medicine Family Medicine General Medicine Neurology OB/GYN Specialty Oncology Orthopaedics Pediatrics Psychiatry Radiology Radiation Oncology Surgery Other (specify): Page 1 ACTIVITY DESCRIPTION Please provide a 4-5 sentence paragraph that describes the overall educational purpose and goal of this activity. SPONSORSHIP Direct: OCME and UCD department/division and, if applicable, an outside accredited entity involved in planning Joint: OCME and UCD department/division and non-UCD, non-accredited provider involved in planning Identify joint provider(s): TYPE OF CREDIT REQUESTED Note: Only AMA/PRA Category 1 available for RSS American Medical Association AMA/PRA Category 1 CreditsTM American Academy of Family Physicians (AAFP): AAFP member must be involved in planning the activity Accreditation Council for Pharmacy Education (ACPE): Pharmacist must be involved in planning the activity California Board of Behavioral Science (BBS): LCSW/MFT Other (specify): COMMERCIAL SUPPORT (EDUCATIONAL GRANTS) AND EXHIBIT FEES [C 7, 8, 9, 10] Activity directors agree to develop this activity independent of commercial interests and according to accreditation requirements. All commercial support is managed by the OCME. Letters of Agreement for educational grants must be signed by the OCME representative. The OCME maintains separation of promotion from education; therefore exhibit fees are also managed by OCME. Yes No Do you plan to solicit educational grants? If yes, please identify companies: Yes No Do you plan to solicit exhibit fees? If yes, please identify companies: SECTION 2: LEADERSHIP AND ADMINISTRATIVE SUPPORT ACTIVITY DIRECTOR OR COURSE CHAIR Physician or base scientist who has overall responsibility to plan, develop and implement the activity Name/Degrees: Title: Department: Division: Address: Phone: Email: Administrative Contact: Phone: Email: ACTIVITY CO-DIRECTOR OR COURSE CO-CHAIR (if applicable) Individual who shares responsibility to plan the activity. Name/Degrees: Department: Address: Phone: Title: Division: Email: ADMINISTRATIVE COORDINATOR/CME ASSOCIATE Individual responsible for operational and administrative support of the activity (i.e. staff assistant in director’s department) Name/Degrees: Title: Department: Division: Address: Phone: Fax: Email: Page 2 PLANNING COMMITTEE (if applicable) Others responsible for designing and implementing the activity Name/Degrees: Title: Institution/Department/Division: Name/Degrees: Email: Title: Institution/Department/Division: Email: UCD Employee Yes No UCD Employee Yes No ALIGNMENT WITH UCDHS CME MISSION STATEMENT [C3] Our CME activities are designed to change competence and/or performance and/or patient outcomes as described in our mission statement. This activity is designed to: (check all that apply) Assist physicians and healthcare professionals gain competence and improve performance to become better able in providing quality care in order to change patient outcomes and improve lives Address professional practice gaps of identified specialties and/or the interprofessional health care team Assist in the dissemination of new medical knowledge Promote the practice of evidence-based medicine Address Faculty Development issues Promote Inter-professional education Other (specify): SECTION 3: GAPS, NEEDS ASSESSMENT AND OBJECTIVES [C2, 3] Practice gaps refer to the variance between what the target audience is currently doing in practice and what they should be doing. Said another way, a gap is a problem, issue, challenge, etc. Gaps can be in terms of knowledge (lack of awareness of something), competence (not knowing how to do something) or performance (not actually doing something). The educational need is the cause or reason for the gaps. Objectives state the results of the activity, what the activity is designed to change in terms of what learners should be able to do to close the gaps and meet their needs. Please state gaps, needs, objectives, etc. for topic and/or major topic areas. GAP This NEED Learning Objective The difference between current Identifies Cause or reason for the gap. What learners should be able to do (in practice and desired or optimal a Gap in: Knowledge causes, competence causes terms of changes in competence, practice. Problem, issue, or performance causes. performance or patient outcomes) as a challenge to be addressed. result of attending this CME activity. What is the problem or issue (gap)? Knowledge Competence Performance Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: Page 3 What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). What is the problem or issue (gap)? Knowledge Competence Performance Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). What is the problem or issue (gap)? Knowledge Competence Performance Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). • If more fields for reporting gaps is needed, please find an additional page at the end of this form Page 4 SECTION 4: CONTENT DEVELOPMENT IDENTIFIED BARRIERS AND STRATEGIES TO BE ADDRESSED [C18, 19] What are the real or potential barriers that may prevent learners from achieving changes in competence, performance or patient outcomes? Select all that apply by checking below. Lack of time to assess or counsel patients Lack of consensus on professional guidelines Lack of administrative support/resources Cost Insurance/reimbursement issues No perceived barriers Patient compliance issues Other (specify): Describe how you will attempt to address these identified barriers in the activity: COLLABORATION AND COOPERATION [C20] Interprofessional teamwork and team based patient care can improve health care quality and patient safety. Who else should be included in the planning and delivery of this activity to promote team learning and how will you include them? Are there internal Yes No. If yes, please explain. and/or external stakeholders that could be included in the planning process? QI/Patient Safety Patients Nurses How will collaboration enhance the activity’s intended outcomes: Pharmacists Dentists Social Workers Physician specialists Primary care physicians Outside organizations QUALITY IMPROVEMENT [C21] We encourage you to think about ways to incorporate quality improvement measures into the planning of this CME activity. Yes No. Will the content of this activity include or address one or more of the measures below? If yes, please check the appropriate box(s) and describe. Institutional Quality Goals Patient Safety Sentinel Events Performance/Quality Improvement Measures Other quality improvement metrics Specialty Society Quality Goals CULTURAL AND LINGUISTIC COMPETENCY Select one or more areas of emphasis you will implement to address this competency as required by California Business and Professions Code, Section 2190.1. Apply linguistic skills to communicate effectively with target Incorporate translation resources and/or integrate relevant population strategies into course materials Use cultural information to establish therapeutic relationships Incorporate review and explanation of relevant regulations regarding linguistic access Elicit and incorporate pertinent cultural data in diagnosis and Other (specify): treatment Understand and apply cultural and ethnic data to the process Not applicable to activity content (if checked, please explain): of clinical care PAIN MANAGEMENT Select one or more areas of emphasis you will implement to address this competency as required by California Business and Professions Code, Section 2190.5. Pain management Care of terminally ill and dying patients N/A to activity content GERIATRIC CARE Select one or more areas of emphasis you will implement to address this competency as required by California Business and Professions Code, Section 2190.3. Geriatric medicine Care of elderly patients N/A to activity content Page 5 SECTION 4: CONTENT DEVELOPMENT DESIRABLE PHYSICIAN ATTRIBUTES/CORE COMPETENCIES [C6] CME activities are developed in the context of desirable physician attributes. Check below to identify American Board of Medical Specialties (ABMS)/Accreditation Council for Graduate Medical Education (ACGME) or Institute of Medicine (IOM) core competencies to be addressed in this activity. Briefly describe activity content related to competencies identified. COMPETENCY CONTENT (e.g. lecture title; workshop, discussion, panel, etc) Provide patient care or patient-centered care Medical knowledge Practice-based learning and improvement Interpersonal and communication skills Professionalism System-based practice Work in interdisciplinary teams Apply quality improvement Utilize informatics Employ evidence-based practice SECTION 5: EDUCATIONAL FORMAT EDUCATIONAL FORMAT [C5] Select the educational format(s) that will be used to facilitate change in competence, performance or patient outcomes. Check all that apply and provide rationale. METHODS TO ENGAGE LEARNERS RATIONALE FOR FORMAT Case studies Audience response system Panel discussion with Q&A Debate Hands-on lab sessions Simulation Small work groups Other: Lecture with Q &A Page 6 ADDITIONAL RESOURCES TO REINFORCE LEARNING [C17] Attendees place great value on additional resources or tools that they can use. Are there additional resources such as the ones listed here that could be provided to learners to enhance change as an adjunct to this activity? Yes No If yes, please describe how they will be provided to learners. Reminder systems, checklists Newsletters, booklets, DVDs Posters, safety flip charts Patient assessment tools Post activity follow up Algorithms, clinical protocols Pocket card guidelines Patient educational material Other: SECTION 6: EVALUATION AND OUTCOMES ASSESSMENT EVALUATION AND OUTCOMES MEASUREMENT [C3, C11] How will you measure if changes occur in competence, performance, and/or patient outcomes? Check all that apply. COMPETENCE Evaluation form for participants (required) Physician and/or patient surveys Audience response system (ARS) Case Based Test Customized pre/post-test Other (specify): PERFORMANCE Demonstration of adherence to guidelines Chart audits Direct observations Other (specify): Customized follow-up survey/interview/focus group about actual change in practice at specified intervals PATIENT OUTCOMES Observed changes in health status measures Observed changes in quality/cost of care Measure mortality and morbidity rates Patient feedback and surveys Other (specify): OUTCOMES ASSESSMENT A. Do you have plans to follow up with the participants for a post-activity outcomes assessment? B. Would you be willing to partner with OCME to develop a post-activity outcomes assessment? Yes Yes No No Please provide signature and date below: Activity Director or Course Chair Signature_______________________________________ Date___________________ If available at this time, attach the activity agenda and other materials for review. The CME Advisory Committee approves all requests. Course chairs will be notified after committee review. OCME USE ONLY: Date Application Received: ____________ Date Reviewed: _____________ Approved By: _________ Page 7 CME Specialist Assigned: ______________ Date Approved by OCME: ___________ Type of Activity: Annual _____ New _____ Other _____ Full Service _____ Credit Only _____ RSS______ Type of Sponsorship: Direct ___ Joint ___ Type of Credit: CME ___ Pharmacy ___ Nursing ___ BBS ___ AAFP ___ Other _____ Grants? Yes No Exhibit Fees? Yes No Responsible department ___________________________ Notes: _____________________________________________________________________________________ • What is the problem or issue (gap)? Additional space for Section 3 gaps if necessary: Knowledge Competence Performance Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). What is the problem or issue (gap)? Knowledge Competence Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: Page 8 Performance What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). • What is the problem or issue (gap)? Additional space for Section 3 gaps if necessary: Knowledge Competence Performance Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). Page 9 What is the problem or issue (gap)? Knowledge Competence Performance Why does the gap exist? What educational needs (knowledge, competence, performance) should be addressed to close the gaps? The solution to address or fix the problem or issue. After attending this activity, participants should be able to: What sources did you use to identify the needs? Please list and attach examples (journal article, CDC guidelines, etc). Page 10