CME Activity Proposal for Consideration
advertisement
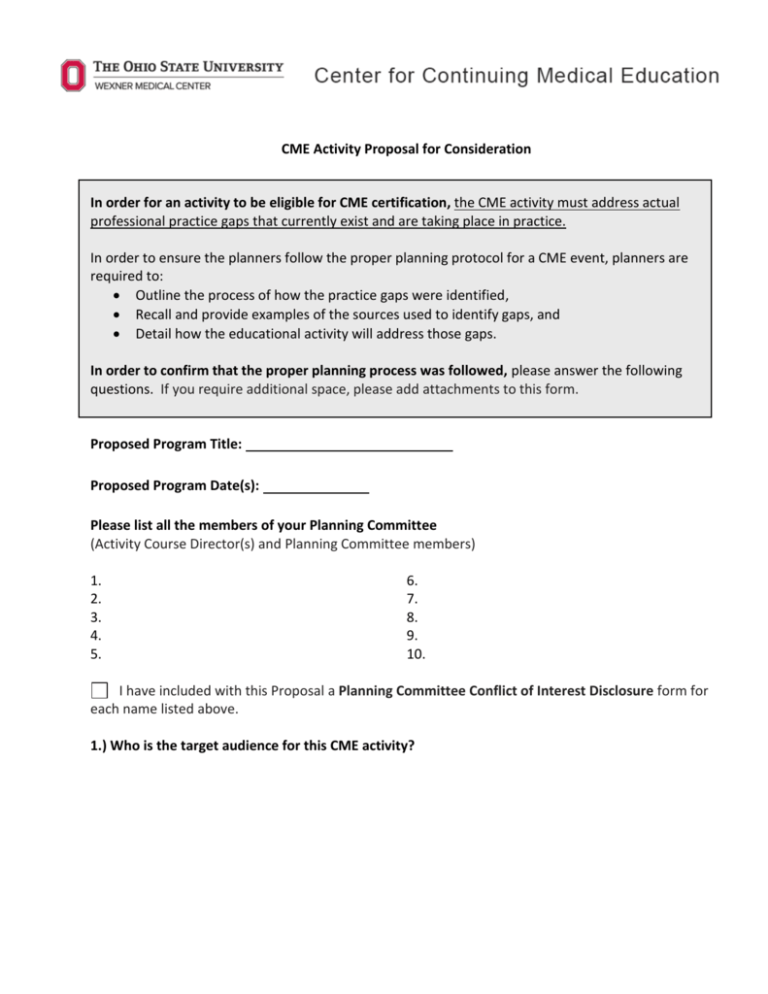
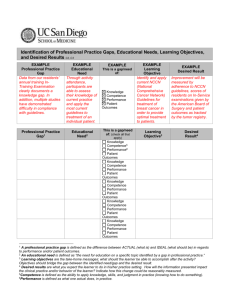
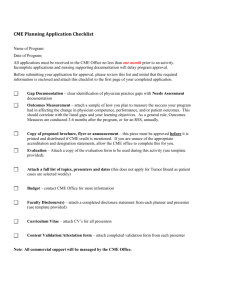
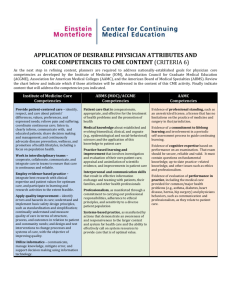
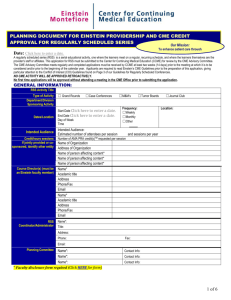
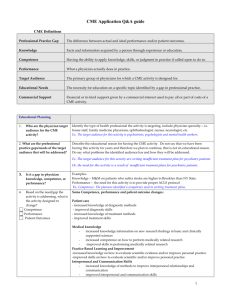
CME Activity Proposal for Consideration In order for an activity to be eligible for CME certification, the CME activity must address actual professional practice gaps that currently exist and are taking place in practice. In order to ensure the planners follow the proper planning protocol for a CME event, planners are required to: Outline the process of how the practice gaps were identified, Recall and provide examples of the sources used to identify gaps, and Detail how the educational activity will address those gaps. In order to confirm that the proper planning process was followed, please answer the following questions. If you require additional space, please add attachments to this form. Proposed Program Title: Proposed Program Date(s): Please list all the members of your Planning Committee (Activity Course Director(s) and Planning Committee members) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. I have included with this Proposal a Planning Committee Conflict of Interest Disclosure form for each name listed above. 1.) Who is the target audience for this CME activity? 2.) In order to plan this educational activity and identify the professional practice gap(s) that exist for your target audience, what evidence/data/sources were consulted? Sources must prove that the need for this activity goes beyond the sponsor’s own perception/observation of need. a.) Check all that apply: Journal articles or other peer reviewed sources Attach bibliography citing journals or other sources, include journal abstracts or relevant paragraphs that support your educational needs assessment. Clinical evidence/research Attach abstract of evidence. Discussion w/ faculty (clinical/research) Attach minutes or notes of discussions and include any references to data, journals, and other sources. Audio recordings of minutes should be digital and readily convertible to MP3. Needs assessment of audience Attach summary of needs assessment and include description of representative audience sampled. Other: Cite all studies, references, or data used to support educational needs. b.) Please provide a description of your planning process and how you used the sources listed above to identify professional practices gaps and the educational format of this activity. 3.) When identifying the professional practice gaps of your target audience, here are some questions that may have been posed by members of the planning committee: What questions does my target audience have and what does that reveal about their deficit of knowledge? What patient problems or professional challenges are they unable to address? Why are they unable to address the patient problems/challenges without some type of intervention? When considering the questions above and after analyzing the sources you identified in Question 2, please identify the professional practice gap(s) that will be addressed in this CME activity? (C2) 4.) Identify other competencies or sources that were considered when identifying the professional practice gap(s) and planning your educational activity? Refer to the List of Desirable Physician Attributes (for example, IOM competencies, ACGME Competencies, etc.) found on the last page of this Proposal. (C6) 5.) The professional practice gap(s) identified for this activity must be classified as a gap in physician knowledge, competence and/or performance. Please classify each professional practice gap identified for this activity as a gap in knowledge, competence and/or performance. (C2, C3) Gaps in Knowledge = target audience does not have the answers or knowledge. Gaps in Competence = target audience has the knowledge but does not know how to act on it. Gaps in Performance = target audience has a strategy but is unable to implement the strategy or implement the strategy properly in practice. 6.) Based on the need/gap the activity is addressing, what are the desired results of the activity? Said differently, what is the activity designed to change? You must be able to detail how you plan to measure these changes in question 7. (C3) 7.) What type(s) of evaluation method(s) will you use to know if the activity was effective at meeting the need and creating change in competence, performance, or patient outcomes? (C11) To measure a change in COMPETENCE, you must measure if the learner has developed new strategies based on the information provided in the activity. To measure a change in PERFORMANCE, you must measure if the learner made a change in their practice or implemented new strategies as a result of the activity. (As a result of this activity, how do you intend to change your practice? Evaluate learners intent to change, 6 month follow up) To measure a change in PATIENT OUTCOMES, you must measure if the changes implemented by the learner in practice have affected patient outcomes. (chart reviews, changes in quality improvement numbers, etc.) 8.) Are there other initiatives within your institution working on this issue? Are there other organizations we could partner with that are working on this issue? Yes No If yes, what are those initiatives/ organizations and do you have any plans to partner with them? (C18,C20) 9.) Given the information provided above, identify potential topics that may be covered in your activity and how will they relate to the professional practice gap(s). 10.) Please answer the following questions about the educational format of your activity. a.) What will be the format of this activity (Live, Enduring Material, Internet, Other?) b.) What is the educational design of the activity (e.g. presentation, case studies, round table, and simulation)? c.) What is the benefit of this educational format? Why was this educational format chosen/preferred? Please remember to consider adult learning principles and the physician learning and change process. (C3, C5) Revised 2.13.13 Desirable Physician Attributes Please “X” all competencies that apply to your conference/meeting. Institute of Medicine Core 1. Provide patient-centered care identify, respect, and care about patients' differences, values, preferences, and expressed needs; relieve pain and suffering; coordinate continuous care; listen to, clearly inform, communicate with, and educate patients; share decision making and management; and continuously advocate disease prevention, wellness, and promotion of healthy lifestyles, including a focus on population health 2. Work in interdisciplinary teams cooperate, collaborate, communicate, and integrate care in teams to ensure that care is continuous and reliable 3. Employ evidence-based practice integrate best research with clinical expertise and patient values for optimum care, and participate in learning and research activities to the extent feasible 4. Apply quality improvement identify errors and hazards in care; understand and implement basic safety design principles, such as standardization and simplification; continually understand and measure quality of care in terms of structure, process, and outcomes in relation to patient and community needs; and design and test interventions to change processes and systems of care, with the objective of improving quality 5. Utilize informatics communicate, manage, knowledge, mitigate error, and support decision making using information technology ABMS(MOC)/ACGME 6. Patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. 7. Medical knowledge about established and evolving biomedical, clinical, and cognate(e.g., epidemiological and social behavioral) sciences and the application of this knowledge to patient care 8. Practice-based learning and improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements inpatient care. 9. Interpersonal and Communication skills that result in effective information exchange and teaming with patients, their families, and other health professionals 10. Professionalism as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population 11. Systems-based practice as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system for healthcare and the ability to effectively call on system resources to provide care that is of optimal value AAMC 12. Evidence of professional standing such as an unrestricted license, a license that has no limitations on the practice of medicine and surgery in that jurisdiction. 13. Evidence of a commitment to lifelong learning and involvement in a periodic self-assessment process to guide continuing learning 14. Evidence of cognitive expertise based on performance on an examination. That exam should be secure, reliable and valid. It must contain questions on fundamental knowledge, up-to date practice-related knowledge, and other issues such as ethics and professionalism 15. Evidence of evaluation of performance in practice including the medical care provided for common/major health problems (e.g., asthma, diabetes, heart disease, hernia, hip surgery) and physicians behaviors, such as communication and professionalism, as they relate to patient care