Food Physiology
advertisement

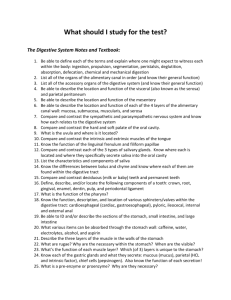
Food Physiology http://www.greathampers.co.uk Digestion Food In Digestion takes place in the gastrointestinal tact which is a long tube about 30ft in length. Digestive Challenges: 1. 2. 3. 4. Waste Out It has to deal with a huge variety of food types It has to prevent self digestion It has to avoid penetration by infectious agents It must maintain mass balance because the system secretes roughly 7 liters of fluid a day, most of which must be reabsorbed. Food Types Protein Carbohydrates Lipids Vitamins Minerals ? Four main Processes: 1. Ingestion 2. Digestion (Chemical, Mechanical) 3. Absorption 4. Egestion 30 to 120 hours to go from ingestion to egestion. Figure 21-2a Major subdivisions include: 1. Oral Cavity 2. Esophagus 3. Stomach 4. Small + Large Intestine 5. Cloaca – meaning sewer (Latin) Figure 21-2a Accessory Organs: 1. Tongue 2. Teeth 3. Oral Glands 4. Pancreas 5. Liver 6. Gall bladder 7. Host of nerve and glandular systems Figure 21-2a Oral Cavity Adults have 32 teeth, 16 in each Jaw. On one half of each Jaw: 1. Two incisors 2. One canine 3. Two premolars 4. Three molars (incl Wisdom) Oral Cavity In general the arrangement of teeth depends on feeding habits. Humans being omnivores tend not to a greatly specialized teeth. Weasel - Carnivore Sabertooth tiger Oral Cavity Children only have 20 teeth, so-called milk teeth. These are replaced at about 6 years. At 18 years or more, additional molars appear in the form of “Wisdom” teeth. Tooth Structure Three layers: 1. Pulp 2. Dentine 3. Enamel Pulp contains blood vessels and nerves. Dentine is largely inorganic (70%) but it is alive in the sense that it can be replaced. Enamel is a crystalline calcium phosphate and fluoride material. It is brittle and the hardest material in the human body. It is essentially dead. Not replaceable. Salivary Glands and Saliva We all secrete roughly 1.5 L saliva per day. At least four major glands surrounding the mouth. Functions of Salvia: Moisten food, allow easy swallowing Contains: 1. R-Protein (Binds B12) 2. Mucus 3. Enzyme Amylase 1. Digests starch to maltose + dextrin 4. Lysozyme 1. Digests bacterial cell walls 5. Lipase 1. Digests triglycerides to fatty acids and glycerol. Swallowing Reflex action once food touches the back of the mouth. Epiglottis closes the larynx diverting food (we hope) to the esophagus. Muscle Diversion Cardiac muscle tissue forms the bulk of the wall of the heart. Like skeletal muscle tissue, it is striated. High fatigue tolerance, force not as strong as skeletal. Contraction graded. Skeletal muscle, prone to fatigue, but can operate very quickly and with great force. Contraction all or none. Smooth muscle, high fatigue tolerance, slow movements. Contraction graded and tends to be involuntary. Esophagus (Oesphagus) Long muscular tube that moves food to the stomach by peristalsis. The muscle of the esophagus is a smooth muscle under involuntary control. The esophagus ends at the cardia (or cardiac) sphincter which is a one way valve. Figure 21-4a Volume roughly up to 2 L but can go to 4/6L in extreme conditions. The stomach connects the esophagus to the duodenum. It is located on the left side. Immediately beneath the stomach is the pancreas. At the lower end of the stomach is the pyloric sphincter value. Figure 21-2b The stomach is quite muscular containing at least three major layers of muscle. Each layer either runs lengthwise, circular or obliquely. The inner surface is highly folded and secretes gastric juice. The stomach is well supplied with blood vessels and the vagus nerve. Figure 21-2b Figure 21-2c Figure 21-25 Parietal Cells – HCI Secretion CA = Carbonic Anhydrase Figure 21-6 Stomach Digestion The liquid content of the stomach is called Chyme. Food stays in the stomach for about 1 to 3 hours (Rule of thumb) Some small molecules are absorbed by the stomach: Glucose Alcohol Aspirin Caffeine` Drugs in general Figure 21-26 Stomach Digestion Enzyme and proteins secreted by the stomach: Inactive Pepsinogen is secreted by the Chief Cells and is converted to Pepsin by the low pH of the stomach. Intrinsic factor – Used later in the small intestine to absorb vitamin B12, secreted by Parietal cells. Pepsin is an endopeptidase. Pepsin is effective against collagen (meat!) Leu, Phe, Trp Figure 21-26 Stomach Digestion Enzyme and proteins secreted by the stomach: Rennin (Chymosin) found in cow stomachs - aspartic acid protease The gene is present in humans but is inactive. Causes cleavage of phenylalanine and methionine in casein (milk protein). Also used in cheese making but is now made recombinantly in organisms such as E. coli. Some gastic lipase is also produced in the stomach. Amylase in the saliva is slowly inactivated by the low pH Figure 21-26 Stomach Hormones: all small peptides Hormones secreted by the stomach: Gastin: The hormone gastrin causes an increase in the secretion of HCl, pepsinogen and intrinsic factor from parietal cells in the stomach. Produced the G-Cells. Inhibited by low pH but stimulated by neuronal, mechanical stretching and protein fragments in the stomach. Histamine: Stimulates HCI production via Gastin Somotostatin: Inhibits Gastin, Parietal cells and Chief Cells. Figure 21-26 Post Stomach Anatomy 1. Duodenum 2. Jejunum 3. ilium 4. ileocecal value 5. Cecum 6. Colon 7. Anus Duodenum Duodenum: 25-30 cm long The word Duodenum means “12” because this part of the intestine is 12 fingers in breadth. The bile duct and pancreatic duct enter the Duodenum at a common point. The bile duct originates from the liver and the pancreatic duct from the pancreas www.gopetsamerica.com Duodenum Duodenum: Brunner’s glands (also called duodenal glands) are found in the Duodenum. These glands secrete bicarbonate ions (so does the pancreas), mucus and a growth factor that stimulates epithelial proliferation. In addition throughout the small and large we find specialized goblet cells which secrete only mucus. www.humanillnesses.com Bile Bile is a yellow/green alkaline liquid secreted by hepatocytes in the liver. Bile is stored in the gallbladder between meals and is discharged into the Duodenum after a meal. About 1 L a day is made and is what gives feces it’s characteristic color. http://www.billcasselman.com Bile - Composition Bile contains the following components: 1. Water 2. Cholesterol 3. Bile pigments: bilirubin, biliverdin These are excretion products from the breakdown of hemoglobin. 4. Lecithin (phophatidylcholine) 5. Bile salts: Essential for fat digestion http://www.billcasselman.com Bile Pigments: biliverdin and bilirubin Heme Biliverdin Bilirubin – Yellow pigment, also responsible for the color of bruises. Bile Salts Bile salts (Na) are derived from Cholesterol via conjugation with glycine or taurine. a) Glycocholate b) Taurocholate Gall stones result from precipitation of bile salts. Glycocholate Taurocholate www.nlm.nih.gov Bile Salts The production of bile salts is also a mechanism for controlling the level of Cholesterol. However about 10 to 25% of the bile salts are reabsorbed in the large intestine, presumably to recover some of the Cholesterol. About 50% of all Cholesterol made or consumed by the body is made into Bile salts. Small Intestine Hormones: all small peptides CCK = Cholecystokinin is a hormone that is produced throughout the small intestine. The release of CCK is stimulated by fatty acids, amino acids and polypeptides. Causes gallbladder to contract and inhibits emptying of stomach, stimulates pancreatic enzymes and bicarbonate. Secretin: This is a hormone mainly produced in the Duodenum in response to acidic chyme that enters the Duodenum. It inhibits acid secretion and stimulates bicarbonate production and hepatic bile flow. Small Intestine Hormones: all small peptides Motilin: This hormone regulates digestive motility and is released by neurons in the small intestine. GIP = Glucose dependent insulinotropic peptide: Inhibits acid secretion and stimulates insulin release - probably most important function (Used to be called gastric inhibitory polypeptide). The effect that GIP has on insulin release means that, paradoxically, glucose is taken up quicker by cells when given orally than when administered by injection. Gallbladder The gallbladder is an active organ where water and NaCl is actively removed to concentrate the bile. The walls of the gallbladder contain smooth muscle that contract the bladder, this action is under hormonal (CCK) and nervous control. The hormonal response is stimulated by fatty acids entering the Duodenum. Ach = acetylcholine The Pancreas The pancreas is both an endocrine and and enzyme secreting (exocrine) organ and as such its cellular morphology reflects this dual function. Acinar cells or an acinus, these secrete pancreatic enzymes + bicarbonate islets of Langerhans containing beta cells. These cells are hormonal and secrete into the blood stream hormones such as Insulin, Glucagon and somatostatin. http://www.dkimages.com/ Pancreatic Juice The pancreatic juice contains a number of components, including proenzymes, water and bicarbonate (required to neutralize the HCl from the stomach). A proenzyme is an inactive enzyme that must be modified before becoming active. 1. Trypsinogen 2. Chymotrypsinogen 3. Procarboxypeptidase 4. Pancreatic lipase 5. Pancreatic amylase - Inactive - Inactive - Inactive - secreted in active form but requires colipase for activity - secreted in active form There are also some RNAses and DNAse, etc. A disease called pancreatic necrosis occurs when the pancreas produces active forms of the proteases, this results in the pancreas digesting itself. Activation of Proenzymes The small intestine secretes an enzyme called enteropeptidase. This enzyme is responsible for activating trypsinogen into its active form Trypsin. Trypsin in turn not only activates the other proenzymes but also activates more trypsinogen. This creates a positive feedback. Activation of Proenzymes CCK = Cholecystokinin is a hormone that is produced throughout the small intestine. The release of CCK is stimulated by fatty acids, amino acids and polypepides. Hormonal Control of the Pancreas Pancreatic Juice - Amylase Starch or Glycogen (Glycogen is more highly branched) http://www.vivo.colostate.edu Small Intestine The small intestine in general includes goblet cells, enzyme and hormone releasing cells, Payer’s patches, large nervous network, rich blood and lymph system and transport proteins. Final digestion occurs on the intestinal borders. 1. Jejunum: Less goblet cells (mucus) and generally lack’s payers patches (lymph nodes), 2.5 m long. The work Jejunum means “empty” because at death the Jejunum is found to be often empty of contents. 2. ileum: Payer’s patches, absorbs B12, large surface area. 2-4 m long. The word ileum means “twisted”. Figure 21-2d Figure 21-2e Figure 21-13 Protein Structure: Terminology Figure 21-16a Endopeptidases Examples: Stomach Pepsin, Pancreatic Trypsin Figure 21-16b Exopeptidases Figure 21-16c Figure 21-17 Protein Digestion: Summary Carbohydrate Digestion: Summary Starch Glycogen Maltotriose (breakdown product of starch, glycogen) Sucrose: Lactose: Maltose: Trehalose Glucose, Fructose Sucrase Glucose, Galactose Lactase Glucose, Glucose Maltase Glucose, Glucose (insect sugar): Trehalase We DO NOT digest cellulose (or lignin – wood - for that matter) Carbohydrate Digestion: Summary Saccharose = Sucrose! Carbohydrate and Proteins All free amino acids and sugars go directly into the blood stream and on to the liver. Diversion: Basic Circulatory System Carotid Jugular Pulmonary vein Pulmonary artery Aorta Vena Cava Hepatic vein Hepatic artery Hepatic portal vein Renal Coronary iliac Mesenteric Artery Basic Circulatory Systems Figure 21-30 Fat Digestion Figure 21-30 Hormone Action Summary Sheet Figure 21-31 – Overview (1 of 4)