Department of Economics Working Paper Series
advertisement

Department of Economics
Working Paper Series
Prices and Quantities in Health Care Antitrust
Damages
by
R. Forrest McCluer
Greylock McKinnon Associates
Martha A. Starr
American University
No. 2014-3
January 2014
http://www.american.edu/cas/economics/research/papers.cfm
http://www.american.edu/cas/economics/research/papers.cfm
Copyright © 2014 by R. Forrest McCluer and Martha A. Starr. All rights reserved. Readers
may make verbatim copies of this document for non-commercial purposes by any means,
provided that this copyright notice appears on all such copies.
2
Prices and Quantities in Health Care Antitrust Damages
R. Forrest McCluer*
Greylock Mckinnon Associates
Martha A. Starr
American University
January 2014
Abstract
Antitrust analysis conventionally assumes that illegal agreements among competitors raise prices and
lower quantities, relative to lawful competition. However, markets for healthcare services have
tendencies towards overprovision, which may increase when competition declines. This paper examines
this possibility using data from a well-known antitrust case in Wisconsin. We find that, in parts of the
state where physician groups illegally divided up markets, costs of physician services rose by about
10% more than they did elsewhere, with about half of this increase due to increased services. This
suggests that higher quantities can contribute to healthcare antitrust damages, along with higher
prices.
Keywords: Antitrust, healthcare, physician services, anticompetitive conduct, damages.
JEL Codes: I11, L4, K21, C43
* Please address correspondence to: R. Forrest McCluer, Greylock McKinnon Associates, One Memorial
Drive, Suite 1410, Cambridge, MA 02142, email: fmccluer@gma-us.com, tel: (703) 237-3010. This
paper was presented at the 3rd Biennial Conference of the American Society of Health Economists, at
Cornell University, June 20-23, 2010. We are grateful to Ana Aizcorbe, Cory Capps, Michael Chernew,
Randy Ellis, Ted Frech, Thomas McGuire, Jim Neiberding, Eileen Reed, George Schink, Robert Tollison,
and seminar participants at the U.S. Bureau of Economic Analysis for valuable comments on earlier
versions of this work. McCluer worked in support of plaintiffs in the Marshfield Clinic cases. The views
expressed in this paper are those of the authors and cannot be attributed to Greylock McKinnon
Associates or any other employee or affiliate thereof. Remaining errors are the responsibility of the
authors.
I. Introduction
A core concern in antitrust analysis is whether an alleged reduction in competition in a given market has
increased prices and reduced quantities supplied, causing allocative inefficiencies and a decline in
consumer welfare. In their seminal framework linking economic reasoning and antitrust law, Landes and
Posner (1981) focused attention on loss of output as the primary cost of the exercise of monopoly power.
Easterbrook (1984) expresses a similar view that, if arrangements are anticompetitive, the output of
those engaging in them must fall. Going beyond this view, Bork (1978) argued that, because consumer
welfare is the proper focus of antitrust analysis, one needs to examine the specifics of a case to
determine whether consumers have been harmed by a given set of anti-competitive practices, without
assuming that a reduction in quantity has to be involved.1 By this reasoning, practices that do not reduce
or possibly even increase output could be the subject of antitrust scrutiny. For example, vertical price
restraints that increase output above the levels that would have been demanded in the absence of
restraints can be welfare reducing (Comanor 1985, Blair and Fesmire 1994, Rey and Tiore 2003).2
Similarly, agreements among producers to restrict or divide markets are treated as illegal per se,
regardless of how they affect quantity or price, because they inherently reduce the range of choices that
consumers face (ABA 1996:181). Nonetheless, the idea that quantity reductions will be found in cases
where firms are engaged in illegal competitive practices remains an expectation, as indicated in the
frequently-cited ruling: “Unless a contract reduces output in some market, to the detriment of
consumers, there is no antitrust problem.”3
Issues of quantity can be especially problematic in antitrust cases related to markets for healthcare
services. Consumers receive utility not from healthcare services per se, but rather from the benefits
these services provide in terms of maintaining or improving their health (Grossman 2000). As they lack
specialized medical knowledge, they need to rely on physicians and other trained professionals to
determine the levels and mixes of services that best help to advance their health goals. Yet incentives
that physicians face may often cause them to recommend more services or different mixes of services
than would be consistent with optimization of social welfare. For one, because patients with health
insurance pay only a fraction of the costs of services they receive, physicians acting as their agents may
provide more referrals or recommend more tests or treatments that would be warranted if patients
faced the full costs of the services they received (Feldstein 1973, Pauly 1986, McGuire 2000). For
another, traditional fee-for-service medicine has tended to reinforce tendencies towards overprovision,
1
As Bork (1978: 34) has stated, “[t]he goal of the law was clearly defined as the maximization of
consumer welfare, and a dynamic principle was built into the rule of reason so that the interpretation
of the law could change and adjust in its pursuit of that goal as economic understanding advanced.”
Others have been more explicit in identifying pure consumer welfare as the basis for antitrust analysis
(e.g. Salop 2005).
2
See Gaynor and Vogt (2000) for discussion of vertical restraints in health care.
3
Chicago Professional Sports Limited Partnership v. National Basketball Association (Chicago Prof. Sports
Ltd. II), 95 F.3d 593, 597 (7th Cir.1996)).
4
as it rewards physicians for providing higher levels of services, rather than for efficiently using
resources to maintain and improve patients’ health (Robinson 2001; Emanuel and Fuchs 2008).
From the point of view of antitrust policy, the issue of interest is whether the extent of overprovision in
a given healthcare market is exacerbated or attenuated by changes in competition. Economic models
allowing for possibilities of overprovision provide ambiguous predictions in this respect. In a model in
which patients prefer to receive referrals to specialists, Iverson and Ma (2011) find that reductions in
competition in markets for physician services will tend to lower levels of service provision because, if
physicians do not have to compete as rigorously to attract and retain patients, they will not cater as
much to patients’ requests for referrals. In contrast, in Allard, Léger and Rochaix’s (2009) model in
which patients face costs of switching from one physician to another, a decline in competition tends to
increase overprovision because under less competitive conditions, physicians have to worry less about
losing patients if they provide more services than patients would like.
More generally, Ma and McGuire (2002) call attention to the role of provider networks in controlling
utilization of healthcare services. In preferred-provider arrangements, health plans build networks of
providers who agree to accept discounted payments and controls over utilization (e.g. utilization
reviews, pre-admission authorizations, prior approvals, second opinions for costly procedures), in
exchange for higher patient volumes from the plan’s enrollees. When health plans have strong
bargaining power relative to provider groups, they have good ability to insist on adherence to utilization
targets, as they can credibly threaten to exclude high-utilization providers from their networks. But
when plans have weak bargaining power relative to provider groups (as when the pools of patients they
control are small, or there are few good-quality provider groups), they may not be able to credibly
threaten to exclude higher-utilization providers from their networks.4 This model too predicts that
overprovision will tend to rise when competition among providers declines, ceteris paribus, by eroding
health plans’ bargaining power relative to that of providers. But overall, the ambiguous predictions from
theoretical models as to how changes in competition should be expected to affect levels of services
provided in given healthcare markets suggest a need for further theoretical work in this area, as well as
empirical investigations of specific cases.
In view of this gap in understanding, this paper uses data from a well-known antitrust case from central
Wisconsin in which physician groups were known to have illegally divided up markets -- and asks what
happened to prices and quantities of physician services in that part of the state as the illegal
agreements phased in. The reduction in competition would be expected to increase prices of physician
services in the affected areas, relative to comparable areas that were unaffected by them; clearly this
represents a central part of the damages experienced by healthcare consumers and third-party payers.
But additionally, the plaintiffs in the case alleged that physicians in the area responded to the decline in
4
This parallels the bargaining framework used by the Federal Trade Commission to analyze hospital
mergers; see Town and Vistnes (2001) and Capps, Dranove and Satterthwaite (2003). See also Ho
(2009) on insurer-provider networks.
5
competition in part by increasing the quantities of services they provided to their patients, so that
higher output as well as higher prices contributed to damages.
This paper reexamines the question of whether output for physician services increased in central
Wisconsin when these illegal market-allocation agreements phased in, using data from 40 million health
insurance claims in the state in 1988-1995. A problem that arises in trying to quantify output of
physicians’ services concerns its heterogeneity, as services range from annual well-child visits to openheart surgery. The paper develops a method for disaggregating charges for physician services into
quantity and price components, using a measure of quantity that values services at their average prices
during the years covered by the analysis. This method bears some similarities to other work on indexes
for prices and quantities in health care (e.g. Berndt et al., 2001; Aizcorbe and Nestoriak 2011), but
whereas they are open-ended measures intended to monitor price changes on an ongoing basis, the
method here focuses on quantifying effects of illegal conduct on prices and quantities in a given time
and place.
The next section of the paper describes the case analyzed in the paper, in which Marshfield Clinic, a
large multi-specialty group practice known for being a high-quality provider in Wisconsin, played a
central role. The third section presents the data to be used and explains the method for disaggregating
charge data into price and quantity components. It also describes the difference-in-difference regression
models used to compare changes in output and prices in the areas affected by the illegal marketallocation agreements, to those in otherwise similar areas that were not. The fourth section presents
empirical results, and a final section concludes. In brief, we find that an important share of the extra
increases in costs faced by patients in the part of the state where illegal arrangements were in effect,
relative to increases faced by patients elsewhere, were associated with increased provision of services.
Estimates from our preferred specification suggest that average annual patient costs rose by about 10%
more in the part of the state in which anticompetitive agreements were in effect than they did
elsewhere in the state, ceteris paribus, with an increase in the quantity of services provided accounting
for about one-half of the extra increase. This underlines the need to consider whether higher quantities,
as well as higher prices, may contribute to healthcare antitrust damages.
II. The Marshfield Clinic class action suit
In the 1990s, a series of lawsuits were brought against the Marshfield Clinic of central Wisconsin, one
of the largest private, multi-specialty group practices in the United States. At that time, the clinic
employed 300-400 physicians who practiced at the main clinic in Marshfield and 24-27 satellite clinics
in the surrounding areas. Most of Marshfield Clinics’ physicians served on the medical staff at St.
Joseph's Hospital, a 524-bed tertiary-care teaching institution adjacent to the main clinic. In addition,
the Clinic owned and operated its own managed-care organization, Security Health Plan. It also had a
6
varied array of business arrangements with other physicians and healthcare providers in the area,
aiming to create a regionally integrated healthcare system known for its quality of care. 5
Table 1 provides a brief chronology of the cases against Marshfield Clinic, as background to the issues
discussed in the current paper. The initial suit was brought by Blue Cross-Blue Shield of Wisconsin and
its HMO, Compcare, charging that Marshfield Clinic and its HMO, Security Health Plan of Wisconsin,
were monopolizing physician services, fixing prices, and illegally dividing markets with competitors. At
that time, the case raised thorny new legal and conceptual issues related to correct definitions of
healthcare markets and valid methods of distinguishing between legal vs. illegal factors contributing to
higher healthcare costs.6 While the jury was persuaded by the charges against Marshfield, the
appeals-court judge, distinguished legal thinker Richard Posner, took issue with much of the analysis
presented in the first case, overturning most of the initial findings and remanding the case to district
court, with instructions to plaintiffs to limit estimates of damages to those associated with illegal
division of markets only. Damage estimates presented in the remand phase were in turn rejected by
the district-court judge, among other things for failing to distinguish between legal and illegal factors
contributing to Marshfield Clinic’s higher patient costs. Summary judgment was issued in Marshfield’s
favor; BCBS appealed unsuccessfully.
Subsequent class-action litigation (referred to as ‘Rozema’ after the named plaintiffs) charged
Marshfield Clinic and other healthcare providers with entering into business arrangements that illegally
restricted trade and increased costs of physician services for people who lived in an eight-county “area
of influence” (AOI).7 Defendants in the case in addition to Marshfield Clinic were Security Health Plan,
the Marshfield-owned HMO; North Central Health Protection Plan, an HMO based in Wassau; and
Rhinelander Medical Center, based in Rhinelander.8 Figure 1 shows the AOI and the defendants’ main
locations. As evidence in the case established, agreements among these providers aimed to reduce
competition between them via such routes as not opening offices in each others’ territories, not
actively marketing in each others’ areas, and not building specialty practices in places where other
providers’ had already established them.9 Some of these agreements had started as early as 1978,
but evidence presented in the case established that they had expanded in breadth and scope after
1991.
5
The Clinic had has continued to grow since then, presently employing some 776 physicians and
6,600 support personnel in 54 locations (Marshfield Clinic 2012).
6
For further discussion of the Marshfield case and the issues it raised, see Troupis (1995), Sage
(1997), Haas-Wilson and Gaynor (1998), Greenberg (1998), Coombs (2005), and McCluer and Starr
(2013).
7
Counties in the AOI included Clark, Price, Lincoln, Oneida, Marathon, Taylor, Portage, and Wood.
Formally, the class constituted people living in the AOI who had acquired physician services in the AOI
after July 24, 1992 (as entered in a ruling after expert reports had been submitted).
8
The case originally included another defendant, Rice Clinic located in Stevens Point (Portage County),
but the judge ruled there was insufficient evidence of its involvement in illegal agreements.
9
As a Marshfield official wrote of discussions held with Rhinelander in 1991, “We do not want to see
ourselves ‘knocking heads’ for the same services for the same patient population” (quoted in Judge
Crabb, Order and Opinion, Oct. 2, 1997).
7
Experts for the plaintiffs argued that these agreements not only enabled physicians to charge
relatively high prices for their services, but also to provide higher quantities of services than they
would have provided under legal competitive conditions. This possibility had come up in the earlier
Marshfield case, but was dismissed by Judge Posner as “a strange inversion of the usual logic of
cartelization, which is that cartelists drive up the market price by (or with the effect of) restricting
their output.”10 In the class-action case, however, the plaintiffs’ experts developed the argument more
fully, both by referring to scholarly research in health economics and by presenting estimates of
damages that distinguished between those associated with higher prices and those associated with
higher levels of services.11 While the judge called the inclusion of increased quantity in damages “a
drastic departure from antitrust economics and unsupported by case law”, she did not think it could be
dismissed on this grounds alone, and on the contrary viewed the evidence as sufficient for a
reasonable jury to conclude that “plaintiffs paid more for physician services because of defendants'
unlawful conduct” (Judge Crabb, Order and Opinion, Oct. 2, 1997). Thus, she declined to grant
summary judgment in the case, and it was subsequently settled.12
IV. Data and methodology
The data used for the analysis come from 40 million insurance claims for professional services
submitted to Blue Cross-Blue Shield (BCBS) by all subscribers residing in the state of Wisconsin in
1988 to 1995.13 This is the same data as was used for the Rozema class action suit. During these
years, BCBS was the largest provider of group health insurance in the state of Wisconsin, having some
10-13% of the statewide market.14
The claims data report basic information on the patient (age, gender, relationship to the subscriber),
the provider, and codes indicating the specific services the patient received. Some 400,000 unique
medical procedures associated with physician services are found in the data, where ‘procedures’ are
10
152 F.3d 588 (7th Cir. 1998). Posner conceded that McGuire’s argument was “a possibility,” but
thought “there [was] no evidence of it”. See McCluer and Starr (2013) for discussion.
11
A first expert, H. E. Frech III, argued that moral-hazard problems in healthcare can lead to
overprovision of services, with anti-competitive conduct tending to increase utilization. As Judge Crabb
summarized his opinion, “ … Dr. Frech states that health care markets are subject to economic forces
different from other industries. It is his opinion that most Americans consume a higher-than-optimal
level of health care because of the moral hazard created by health insurance. When market competition
and managed care are operating properly, they reduce the utilization of physician services. According to
Frech, anticompetitive conduct leads to higher utilization” (977 F. Supp. 1362 (W.D. Wis. 1997)).
12
See Associated Press (1997). In the Rozema case, Judge Crabb ordered that Rice Clinic be dropped
as a co-conspirator and that patients residing in Portage County be dropped from the class (Judge
Crabb, Order and Opinion, October 2, 1997); this ruling came after the econometric analysis was
submitted. Damages were computed as 6.9% times the total health care expenditures of residents of
the AOI. The case settled for a portion of the estimated damages (Coombs 2005: 188).
13
Cases in which out-of-state residents travelled to Wisconsin to receive medical care are excluded
from the analysis to avoid issues of sample-selection bias.
14
Figures from Table E, Office of the Commissioner of Insurance, State of Wisconsin (1988-1995).
8
defined as unique combinations of the characteristics of the service: the Current Procedural Terminology
(CPT), the standard 5-digit code used to classify physician services for billing purposes; three modifiers
of the CPT (type of service, place of service, and number of units of service); the type of provider
(medical doctor or osteopath); and the provider’s specialty (e.g. general practitioner, radiologist, or
thoracic surgeon). The ‘prices’ in the analysis are the charges submitted to BCBS, not payments made
by BCBS; this ensures that measured differences in prices across areas reflect differences in providers’
charges, rather than features of insurance coverage (e.g. deductibles, copayments, negotiated prices).
We use the claims data to compute total real annual costs per patient, then use an index approach to
decompose variations in total costs into price and quantity components. The first step is to compute
total annual costs of physician services for individual i in year t,
:
(3)
where
is the price charged to individual i for service j obtained from provider k in year t, and
is the related quantity. Aggregating all charges over each year for individual patients yields 2.26
million individual-year observations for individuals under age 65.15 (We omit 41,504 records for
individuals aged 65 and over from the analysis, given that the vast majority of people in this age
group have their primary health insurance coverage through Medicare). While some individuals in the
data have records for multiple years, complexities of matching the records imply it is difficult to
structure the individual-year records into a complete (imbalanced) panel data set.16 As a result, we
opt to analyze the data as a pooled cross-section sample instead. To take into account general
inflation in healthcare costs over the period, all prices are deflated by the Bureau of Labor Statistics’
consumer price index (CPI) for all medical services (1995=100).
Next we take averages of prices for each service j across all individuals i, all providers k, and all years:
15
Note that some individuals in the data were covered under a BCBS plan for only part of the year. We
have not tried to convert partial-year records to full-year equivalents, as it is difficult to identify such
cases with certainty.
16
For example, some individuals submit claims in early years of the period analyzed and again in later
years, but we cannot tell whether they incurred no costs in the intervening years or whether they
were not covered by a BCBS plan.
9
________________________
where we refer to
(4)
as the index price for service j. Then specific prices paid for a service can be re-
expressed as deviations from its index price, permitting us to re-write (3) as:
(5)
where the term
is the deviation from the index price associated with individual i’s purchase of
service j from provider k in year t. Re-arranging and letting
be the total quantity of service j
received by individual i in year t (i.e. summing over providers), the individual’s total costs of physician
services can be decomposed as follows:
(6)
=
The first term
(7)
, is a constant-price index of the quantity of services received by individual i in year
t, where outputs are valued at their index prices. This represents the primary measure of ‘quantity’
used in our analysis. In effect,
holds prices constant at average levels prevailing in the period
under investigation, so that increases in
over time necessarily come from changes in quantities of
services received and/or shifts in the composition of services towards those with higher average
prices.17 The second term,
, is a measure of ‘price deviations’ faced by individual i; it is a
weighted average of the differences between the price the individual was charged for a given service
at time t and the index price for that service, with weights given by the quantity of the service
17
In this sense, the quantity measure differs from a standard constant-price measure of output, which
values quantities at prices from a given base year.
10
received by the individual in year t. Thus,
can rise over time either because price deviations of
the services acquired by individual i have increased and/or because the composition of services has
shifted to services with higher deviations. For damage estimation, the key question is whether
differential increases in quantities of services contributed to differential increases in costs among
patients with given characteristics residing in the AOI, compared to counterparts who lived elsewhere.
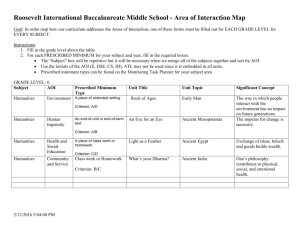
Table 2 and Figure 2 show averages for these variables for individuals residing in and out of the eightcounty AOI. In 1988-90, average total annual costs were no higher in the AOI than they were in the
rest of the state; thereafter, however, they exceeded them by $50-100 (roughly 6.5 to 11.5%). This
is consistent with information presented in the class-action case that the market-allocation
agreements in which Marshfield Clinic was involved increased in breadth and scope after 1991. In the
years when average total annual costs were higher in the AOI than in the rest of the state, the higher
quantity of services tended to be more important in contributing to the higher costs than the price
deviation, although with some variation in the relative importance of the two factors from year to
year. Taking the 1991-95 period as a whole, average annual costs were $84 higher in the AOI than
they were elsewhere, where $68 of the difference (or 80.5%) came from the higher quantity index.
Of course, there may be socio-demographic differences between the AOI and the rest of the state that
contribute to the relatively high quantities of physician services received in the AOI. Notably, because
the areas served by Marshfield Clinic tend to be relatively rural, the baseline health of the population
may tend to be lower than it is elsewhere due to lower income levels, lower levels of education,
different occupational profiles, etc. Similarly, levels of competition among providers tend to be lower
in rural areas, so it is possible that the higher price deviations registered in the AOI reflect the
‘naturally’ higher pricing power of rural healthcare providers, rather than effects of illegal divisions of
markets.
Thus, we use a regression framework to account for legitimate factors explaining variations in total
annual costs, the quantity index, and price deviations across areas. The standard ‘benchmark’ method
of estimating damages estimates a regression of the form:
=
where
+
+α
+
(8)
is a vector of factors expected to influence the individual’s healthcare costs (e.g. age,
gender, type of health insurance, etc.),
is a vector of year dummies intended to capture broad-
based changes in real healthcare spending, and
is a dummy variable equal to 1 if the individual
11
lives in the AOI. Then the estimated coefficient
α indicates whether total annual costs per patient are
higher in the AOI than they are elsewhere, ceteris paribus. To gauge the relative contributions of
higher quantities and higher prices to higher charges in the AOI, we can run regressions of the form:
=
+
+
+
(9)
=
+
+
+
(10)
,
However, if
and
contain unmeasured but lawful sources of variation in costs, quantities
and prices across areas and these correlate with
, then regression estimates of ,
and
will give biased representations of effects of illegal conduct in the AOI. A common concern in this
respect is that the quality of care may vary systematically between physicians in one area and the
other, and/or that patients with given observed characteristics may differ in unobserved ways that
make their health conditions more complex than those of patients elsewhere, so that differences in
costs, quantities and prices between the AOI and ROS reflect hedonic differences in the services
received.18
This problem can be addressed by making use of the fact that, while the data cover the 1988-95
period, the scope of the agreements behind the illegal market allocation broadened after 1991. Thus,
we can estimate difference-in-difference regressions that in effect take initial differences in levels of
the dependent variable between the AOI and ROS to be reflective of persistent unobserved
heterogeneities between the two areas; then controlling for other observable factors that may have
caused the dependent variable to change between 1988 and 1995, an increase in that variable over
that period that is greater in the AOI than it is the ROS is suggestive of an effect of the market
allocation. Specifically, we run regressions of the following form:
=
18
+
+
+
(16)
See McCluer and Starr (2013) for discussion. This issue was more important in the first phase of the
Marshfield-related litigation, which compared patient costs between patients who received a majority
of their care from Marshfield clinic to otherwise similar patients who received their care from other
providers.
12
for the three dependent variables; this amounts to including year dummies that differ between the
AOI and ROS. Then the test for an effect of the illegal market allocation for a given dependent variable
is:
ΔΔ =
-
} - {
-
}
(17)
See Abadie (2005) for methodological discussion and McCluer and Starr (2013) for an application
using data from the remand phase of the Marshfield case.19
In principle, some part of the differential increase in quantity in the AOI could have been associated
with increases in the quality of care than would have been warranted under an economic calculus of
costs, benefits and risks; in this case, the DID estimate of the effect of the illegal market agreement
would overstate the anticompetitive increase in quantity. However, in the present case direct review of
evidence on the quality of care did not suggest any basis for concern about a possible bias from this
source. Notably, at the outset of the period Marshfield Clinic was widely perceived to have a
substantial quality advantage over other providers in the state; while it continued to work on
improving its procedures and facilities in the period, its efforts were well in line with those of other
providers in the state.20 So while we do not expect there to be bias from differential changes in quality
in the present case, the possibility should be investigated in others, given that correct estimation of
damages requires all legal sources of differential outcomes across providers or across areas to be
accounted for.21
Table 3 gives definitions of the variables used in the regression analysis along with sample means. Our
information on individual characteristics is limited to what is reported on insurance claims, but these
cover many of the factors that would be expected to affect use of healthcare services, especially age,
gender, marital status, and type of insurance plan (general indemnity, Federal government workers,
19
This differs somewhat from the standard DID specification, which uses a stark division between a
before-and-after period to identify the effect of interest (Rubinfeld 2010). In the present case, we
favor the more flexible specification implied by (16), given that the illegal market-allocation
agreements were known to have phased in at different times in different places within the AOI. Still,
for purposes of comparison, we also estimated standard before-and-after DID regressions, using the
formal definition of the class period (from 1992 on) as the market allocation period. Results in this
case show an increase in total patient costs that is, not surprisingly, somewhat smaller than is the
case when 1988 and 1995 are compared (i.e. an increase of $64 from 1988-91 to 1992-95, vs. $83
from 1988 to 1995); however, the standard method traces a much larger share of this increase to
increased quantity (90% vs. 53%).
20
For example, in the remand phase of the trial, BCBS expert Thomas McGuire noted that the share of
procedures performed by specialists (rather than primary care physicians) did not rise faster at the
Clinic than it did elsewhere, as might be expected if its quality of care was improving at an
extraordinary rate. See also McCluer and Starr (2013).
21
Hammer and Sage (2002) and Vogt and Town (2006) suggest that claims of increased quality
accompanying increases in market power should be looked at skeptically, as they are not often
substantiated by review of clinical outcomes, Moreover Gaynor (2006) finds that quality of care is
better favored by competition than concentration.
13
etc.).22 We incorporate effects of age and gender by interacting age ranges with gender; this allows
age profiles of health costs, quantities and price deviations to differ between men and women. To
account for other differences across areas that may contribute to the higher costs found in the AOI,
we include county-level measures of the socio-demographic characteristics of the population,
including: the share of the population with a high school education or more, the population density,
the unemployment rate, real per capita income, real medical-assistance payments per capita, and
birth and death rates.
The basic specification closely parallels that which was used in the Rozema class action case. We also
estimate a number of alternative specifications, adding explanatory variables and varying the
estimation method used. A possibility that came up repeatedly in the Marshfield-related litigation
cases was that healthcare prices in given parts of Wisconsin were relatively high because of legal
competitive factors, instead of or in addition to illegal market division. First, because ratios of
physicians to population are known to be relatively low in areas of low population density, and the AOI
is largely rural, this may confer some ‘natural’ ability to price above marginal costs and/or provide
extra services to their patients unrelated to illegal behavior.23 Because the counties in the AOI all have
relatively low population density yet vary in the degree of concentration in the market for physician
services, we add the Herfindal-Hirshman index (HHI) to the variables included in the regression
analysis. The HHI measures market concentration as the sum of the squared market shares of all
providers in the market; specifically, we measure it as the share of all billing events for all providers
used by residents of the county.24
Another issue related to legal competitive factors concerns effects that health-maintenance
organizations (HMOs) may have on prices and quantities (Baker 1994, Baker and Corts 1995, HaasWilson 2003). On one hand, if a given local market has a well-developed HMO sector, it may tend to
act as a check on price increases, as insurance companies may negotiate harder for lower prices to
limit patients’ out of pocket costs and avoid loss of business to managed care. Baker (1994) and Baker
and Corts (1995) refer to this as a ‘market discipline’ effect. In this case, total costs and price
deviations may tend to be lower in counties where HMO penetration is higher, ceteris paribus. On the
other hand, the more people have substituted into managed care in a given market, the more likely it
22
Identifying information such as name and address was either masked or not made available.
As Posner wrote in his opinion on BCBS’s appeal (65 F.3d 1406 (7th Cir.) 1995), “If the Marshfield
Clinic is a monopolist in any of these areas it is what is called a ‘natural monopolist,’ which is to say a
firm that has no competitors simply because the market is too small to support more than a single
firm. If an entire county has only 12 physicians, one can hardly expect or want them to set up in
competition with each other. … Twelve physicians competing in a county would be competing to
provide horse-and-buggy medicine.”
24
The HHI is commonly used in analyses of the competitiveness of health care markets (e.g. Lynk
1995, Schneider et al 2008). As discussed in Frech, Langenfeld and McCluer (2004), computing the
HHI in terms of the location of the patient rather than the provider avoids issues of sample selection
and case mix. We also ran the regressions using HHIs computed from providers’ shares of the value of
total billings rather than the total number; there is no qualitative difference in results, which is not
surprising given the high correlation between the two measures (0.95).
23
14
will be that those remaining in traditional indemnity insurance plans are likely to have worse
underlying health. Baker (1994) and Baker and Corts (1995) call this as a ‘market segmentation’
effect. In this case, total costs and quantities may be higher in counties where HMO penetration is
high, as the pool of patients remaining outside of the HMO sector will have relatively poor health.
To account for these possibilities, the regressions include a measure of HMO penetration, namely, the
share of the county’s population enrolled in an HMO. A complication is that some of the defendants in
the class-action suit were HMOs, including one wholly owned by Marshfield Clinic; consequently, if
people enrolled in defendant HMOs were included in the measure of HMO penetration, the degree of
competition coming from managed care in the AOI would be overstated.25 So in computing HMO
enrollment for counties in the AOI, we exclude people who were enrolled in Security Health Plan or
North Central Health Protection Plan from the penetration rate.
V. Empirical results
Table 4 presents results from the basic difference-in-difference specification, which controls for
sources of persistent unobserved heterogeneities between the AOI and ROS and uses differential
changes between the areas to gauge the effects of illegal competitive behavior. Before looking at the
comparison of changes in the AOI vs. ROS, it is first valuable to examine the estimated effects of the
other explanatory variables, which suggest that the specification captures a number of interesting
and/or expected variations across individuals in costs, quantity and price deviations. The results
indicate that, for both men and women, total annual spending on physician services rose significantly
with age; for example, total costs were $417.6 (=$767.5-349.9) higher for women in the age 55-64
age range than for otherwise similar women in the 25-34 age range, while for men the analogous
difference was $1165.1 (=$1161.9-(-3.2)). This is consistent with a large literature documenting the
strong dependence of healthcare costs on age (e.g. Alemayehu and Warner 2004). The increase
occurs earlier for women than it does for men, although for men spending rises relatively steeply from
age 45 on.26 In both cases, increases in spending with age are largely due to increases in the quantity
of services; estimates for the price-deviation equation show some shift towards relatively more costly
services after childhood, but it is modest compared to the increase in quantity.
Married subscribers had somewhat lower total spending on physician services than single subscribers,
ceteris paribus, which has mostly to do with the lower quantity of services acquired; for example, of
the $50.90 difference in spending between married and single subscribers, $48.40 was due to the
lower quantity index. This is broadly consistent with clinical evidence that people who have good
marriages and good networks of social relations tend to have better health (Cohen 2004, Parker-Pope
2010). Not surprisingly, total spending is substantially and significantly higher for people in high
insurance risk-sharing plans, where this is almost entirely due to very high quantity of services. Total
25
As McCrary and Rubinfeld (2009) caution, including covariates that are causally related to the
conspiracy on the right-hand side of a regression biases estimates of damages due to the conspiracy.
26
Note that results are for physician services only.
15
spending is also relatively high for subscribers enrolled in BCBS’s Federal Employee Program, and
relatively low for subscribers enrolled in national programs, where in both cases differences in the
quantity index are much more important than price deviations.
Among the county-level variables, total spending on physician services was relatively low for
individuals in counties with relatively high shares of the population with a high school degree or more;
the effect is due almost equally to lower quantity and a lower price deviation, although only the latter
effect is significant. Ceteris paribus, total spending was relatively high for people living in counties
with high population densities, due to both higher quantities and higher prices. Individuals in counties
with relatively high unemployment had relatively high total spending, due almost entirely to relatively
high quantities of services. This seems to run counter to Ruhm’s (2000) finding that ‘recessions are
good for your health,’ although the types of cyclicalities he identifies (e.g. motor vehicle accidents)
may affect spending on hospital services more than spending on physicians. Individuals in counties
with relatively high per capita income had relatively high spending due to both quantities and prices;
in contrast, those in counties with relatively high medical assistance per capita had relatively high
spending, due entirely to relatively high price deviations. Relatively high birth and death rates had no
significant effect on total spending or the quantity index, but they were associated with relatively low
price deviations.
Turning to the comparison of changes in the AOI vs. the ROS, the results indicate that, controlling for
other factors, total annual spending on physician services in the AOI rose by $303.6 between 1988
and 1995, while it rose by $231.0 in the ROS; the difference between the two of $82.6 is statistically
significant.27 This is consistent with the expectation that the illegal market-allocation agreements
boosted spending on physician services.28 With respect to the source of the increase, the estimates
show that both quantities and price deviations rose significantly in both the AOI and the ROS between
1988 and 1995, where the increases in quantities and price deviations were both larger in the AOI
than they were in the ROS. Looking at the decomposition of the $82.6 differential increase in total
costs in the AOI, the estimates suggest that $49 (59.3%) of this increase came from the greater
increase in quantity in the AOI relative to the ROS.29 This supports the expectation that some part of
the illegal market power acquired by physicians in the AOI due to the market-allocation agreements
resulted in intensification of service provision, in addition to higher prices.
Table 5 shows results incorporating the HHI and HMO penetration variables using alternative
specifications. As shown in Panel (B), adding these two variables to the basic DID specification has
only modest effects on the estimated effects of being in the AOI. The estimated effect on total
27
Interestingly, this estimate of the effect of the illegal market allocation is higher than in the
analogous estimate of $62 from a simple dummy-variable specification [8], suggesting the latter is
biased downward rather than up.
28
See also McCluer and Starr (2013) for related results and discussion.
29
In the dummy-variable specification [8], the higher quantity of services contributes a somewhat
smaller share (43.2%) of the higher level of total spending on physician services in the AOI, ceteris
paribus.
16
spending on physician services is virtually unchanged at $82.7 (vs. $82.6 in the basic DID). The
quantity index declines from $49.0 to $44.2, while that on the price deviation moves up from $33.5 to
$38.5, so that the relative importance of the change in quantity index in the differential change in
spending in the AOI is a bit smaller (53.4% vs. 59.3%). Interestingly, controlling for whether a person
lived in the AOI, an increase in the HHI was associated with a significant increase in total costs, which
was due to a significant increase in the price deviation with no significant change in quantity. This
indicates that, at least in Wisconsin during this period, concentration per se was not associated with
increased quantity, but rather the business practices and agreements in use in the AOI. 30 The results
also show that, ceteris paribus, costs were higher in counties with relatively high HMO enrollments,
largely reflecting effects on the price deviation. This finding is more consistent with ‘market
segmentation’ than with ‘market discipline’, although in the former case we expected higher costs to
reflect higher quantity rather than higher price. Broadly, these results suggest that basic results
concerning the differential increases in prices and quantities of physicians services in the AOI are not
due to omitted competition-related variables.
Conceivably, effects of increases in the HHI on output and prices may be nonlinear: For example, it
may only be in highly concentrated markets that further concentration permits anticompetitive
increases in output. To test for this possibility, we re-estimate the previous model including a spline
for markets with HHIs above 2500, the cut-off between moderately and highly concentrated markets
in the current merger guidelines of the U.S. Department of Justice and Federal Trade Commission
(2010). As shown in Panel (C), the results suggest that increases in the HHI in highly concentrated
markets have no extra effect on total annual spending on physician services, although this masks
some contrasting effects on quantities and prices. For the quantity index, increases in the HHI below
2500 are estimated to lower the quantity of services acquired by a given individual, but above 2500
further increases in concentration tend to raise it; this is consistent with the idea that overprovision of
services is not a simple function of the degree of market power, but that situations of highly
concentrated market power may encourage it. In contrast, increases in the HHI boost the pricedeviation in markets that are unconcentrated to moderately concentrated, with no further effect in
highly concentrated markets.
Finally, it has been suggested that comparing measures of spending, quantities and prices for
physician services in the AOI to the whole rest of the state of Wisconsin may be inappropriate, given
that the AOI mostly covers areas of low population density. Thus, we re-run the analysis confining the
sample to individuals in the 60 counties with a population density below 200 residents per square
mile; this reduces the sample size to 619,932 individual-year observations. As shown in Panel (D),
this has some notable effects on magnitudes of estimated coefficients. It increases the magnitude of
the differential increase in total costs in the AOI (from $82.7 to $105.7), although it leaves the
30
In fact, if the regressions are run using observations from the ROS only, the estimated effect of the
HHI is positive and significant in the regressions for total costs and the price deviation, but negative in
the regression for quantity, although the latter effect is significant at a 10% level only.
17
contribution of the quantity index to this increase in the same range (56.4%). This indicates that, if
anything, failing to confine the sample to counties with relatively low population densities causes
underestimation of the damages associated with acquiring healthcare services in the AOI, not
overstatement. In this part of the state, increases in the HHI increase both the quantity index and the
price deviation. Here too increases in HMO enrollment tend to boost total costs due a greater price
deviation, although the estimated magnitude of the effect is smaller. Altogether, the results in Table 5
confirm that results of the basic specification are robust to incorporation of additional competitionrelated variables and to other plausible changes in specification.
VI.
Conclusions
In sum, our econometric analysis indicates that, in Wisconsin in the 1988-95 period, quantities of
physician services rose more quickly in the AOI than they did elsewhere, consistent with the idea that
the reduction in competition amongst Marshfield Clinic and its co-conspirators created an environment
in which they could increase both prices and quantities of services by more than would have been
possible without the anticompetitive agreements. In our preferred difference-in-difference specification
(Panel (B) of Table B), which controls for persistent unobserved heterogeneities across areas and for
other competition-related factors, real patient costs rose by an extra $82.7 (9.9%) in the AOI between
1988 and 1995, with 53.4% of this increase associated with an extra increase in quantity. With all of
our estimates of differential increases in total costs being between $62 and $115, and estimates of the
contribution of increased quantity mostly in the 35-60% range, the magnitudes of our preferred
estimates are in the middle of these ranges. Again we underline that, although concerns that
difference-in-difference estimates of in principle may pick up differential changes in quality of care as
well as effects of illegal competitive conduct, in the present case direct review of evidence on changes
in the quality of care did not suggest any basis for concern about this potential source of bias in the
damage estimates. Taken broadly, our findings illustrate that estimates of the damages due to the
illegal market allocation that focused solely on differential increases in prices would have understated
the amount of damages by an appreciable amount.
The main implication of our findings is that, especially in cases where a service-intensive practice style
is a part of the competitive strategy of a provider accused of illegal anticompetitive conduct, methods
of damage estimation should not be based on price only, but rather should also consider whether
increased quantities of services contributed to the monetary losses experienced by consumers and
health insurers. Losses from this source are not entirely missing from the standard damage-estimation
method: Because this method multiplies the price differential due to anticompetitive behavior by the
actual quantity, and some part of the latter reflects the extra overprovision associated with this
behavior, some part of the extra quantity factors into the estimated loss. But to account for the fact
that these units would not have been bought at all under legal competitive conditions, the extra
quantity of services valued at the competitive benchmark price should also be added in. In the end, it
18
is an empirical question whether consumers and/or insurers in a given case are entitled to damages
from overprovision of services relative to what they would have bought in the absence of
anticompetitive behavior. The method of disaggregating damages from prices and quantities
presented in this paper provides a way to check.
19
Figure 1. Area of Influence (AOI)
20
Figure 2. Trends in average annual costs and contributions from quantity and price
(a)
Average annual
costs of health care services
(b)
Decomposition of
the difference between the AOI and ROS due to quantity and price
Note: Values are converted to 1995 dollars using the medical care CPI (1995=100).
21
Table 1. Chronology of Marshfield-related litigation
Year
Phase
Main issues
Main findings
1994
Original
Marshfield
case31
Jury found in favor of
the plaintiffs.
1995
Marshfield
appeal32
1997
Remand
case
1998
Blue
Cross
appeal
1997
Rozema
Class
Action
Case37
BCBS of Wisconsin and its HMO, Compcare, sued
Marshfield Clinic and its HMO, Security Health Plan, for
monopolization of physician services, price fixing and
illegally dividing markets with competitors.
Judge Posner found that managed care does not
constitute a separate market so the charge of
monopolization was not supported, but upheld the
finding of illegal division of markets. This required reestimation of damages based on this charge only.
A first expert for BCBS (John Beyer) found that
Marshfield clinic charged higher prices for given
procedures, compared to providers in a similar but
competitive part of the state. A second (Thomas
McGuire) presented econometric evidence that
Marshfield’s illegal exercise of market power increased
both prices and quantities of services in the affected
area.
Judge Posner affirmed that BCBS experts failed to
separate legal vs. illegal factors contributing to
Marshfield’s higher prices, and disagreed that quantity
increases could contribute to damages.35
A class action suit was brought against Marshfield Clinic
and other providers in Central Wisconsin for illegal
restraint of trade.38 One expert (H. E. Frech III) argued
that moral-hazard problems can lead to overprovision
of healthcare services, with anti-competitive conduct
tending to increase utilization. The expert who
computed damages (Robert Tollison) disaggregated
overcharges into price and output components.
31
Case was remanded to
district court.33
Judge Crabb found
McGuire’s model lacked
precedent and failed to
separate legal vs. illegal
factors in Marshfield’s
higher prices. Summary
judgment was granted
in Marshfield’s favor.34
The lower court’s
opinion was largely
upheld.36
Judge Crabb declined to
grant summary
judgment, writing that
evidence was sufficient
for a reasonable jury to
conclude that the
defendants exercised
market power in the
area of influence.39 The
case was subsequently
settled.
Blue Cross and Blue Shield United of Wisconsin v. Marshfield Clinic 883 F.Supp. 1247 (W.D. Wis.
1995). Formally, the suit was a Section 2 monopolization charge combined with Section 1 price-fixing and
division-of-markets charges.
32
Appeal to the 7th Circuit Court of Appeals. (65 F.3d 1406 (7th Cir. 1995)).
33
65 F.3d 1406, 1416 (7th Cir.1995).
34
980 F. Supp. 1298 (W.D. Wis. 1997). The initial order of April 1, 1997, was revised on April 8 and filed
on April 14.
35
McCluer and Starr (2013) discuss issues that arose in interpreting results from McGuire’s model, which
was based on a difference-in-difference approach.
36
152 F.3d 588 (7th Cir. 1998).
37
Rozema, et al v. Marshfield Clinic, Security Health Plan of Wisconsin, Inc., North Central Health
Protection Plan, and Rhinelander Medical Center, S.C., 977 F. Supp. 1362 (W.D. Wis. 1997).
38
Formally, the charges fell under the Sherman Act, 15 U.S.C. § 1, and Wis. Stat. §§ 133.03 and 133.14.
39
See Associated Press (1997).
22
Table 2. Trends in average total annual charges, quantities and prices, in constant 1995 dollars
Inside AOI
Rest of state (ROS)
Difference (AOI-ROS)
Year
All years
888
875
12
844
845
-1
44
30
13
1988
1989
1990
1991
1992
1993
1994
1995
Change
1988-95
672
707
772
859
958
979
1,025
1,052
380
686
708
766
841
936
955
1,004
1,031
345
-14
-2
6
18
23
24
20
22
36
730
756
769
806
859
905
920
988
258
747
764
773
803
863
903
913
976
229
-17
-8
-4
3
-3
3
7
13
30
-58
-49
3
53
99
74
105
64
122
-61
-56
-7
37
73
52
92
55
116
3
6
10
15
26
21
13
9
6
Note:
= total real annual costs in 1995 dollars.
Figures may not sum precisely due to rounding.
= quantity index.
= price deviation.
23
Table 3. Variable names and definitions
Variable name
Competition-related variables
Area of Influence (AOI)
HHI
HMO enrollment
Definition
=1 if individual lives in Clark, Lincoln, Marathon, Oneida, Portage,
Price, Taylor, or Wood county; 0 otherwise
Herfindahl-Hirshman index for the county, computed from billingprovider events in the given year
Enrollment in health maintenance organizations (excluding HMOS
participating in the illegal market division), as a share of the
county’s population
Individual characteristics
Age
Female
Single subscriber (omitted)
Married subscriber
Spouse of subscriber
Other dependant of subscriber
Plan types:
Indemnity (omitted)
Administrative services only
Cost-Plus Contracts
Federal Employee Program
National Programs
High Insurance Risk Sharing
Other BCBS plans
County characteristics*
High school and over
Age in years (entered into the regression in age categories
interacted with gender)
=1 if individual is female; 0 otherwise
=1 if individual is single subscriber; 0 otherwise
=1 if individual is married subscriber; 0 otherwise
=1 if individual is spouse of subscriber; 0 otherwise
=1 if individual is other dependant of subscriber; 0 otherwise
Dummy variables equal to 1 if plan is of the relevant type
Traditional indemnity plan offered by Wisconsin BCBS
BCBS receives fixed rate to administer claims for another insurer
Plans administered by BCBS that reimburse providers for their
costs plus a specified margin
BCBS plan offered to Federal Employees
Other traditional BCBS indemnity plans based elsewhere
State-organized plan offering insurance to people unable to
obtain coverage due to preexisting conditions
BCBS plans other than those listed above
Share of persons aged 25 years or more having a high school
diploma or more
Population density
County population divided by the county’s area in square miles.
Unemployment rate
Unemployed persons as a share of the civilian labor force
Personal income per capita
Personal income per capita in thousands of 1995 dollars (deflated
using the consumer price index for all urban consumers)
Medical assist per capita
Real medical assistance per capita in thousands of 1995 dollars
(deflated using the consumer price index for medical care)
Birth rate
Births per 100,000 residents. From U.S. Census Bureau, County
and City Data Book
Death rate
Deaths per 100,000 residents. From U.S. Census Bureau, County
and City Data Book
* Data are taken from the Area Resource File (2004) unless otherwise noted.
24
Table 4. Basic regression: Difference-in-difference specification
Total annual costs
Quantity index
Coeff.
Individual characteristics
Male in age range:
5-17 years
18-24
25-34
35-44
45-54
55-64
Female in age range:
Under 5 years
5-17
18-24
25-34
35-44
45-54
55-64
Married subscriber
Spouse of subscriber
Other dependant of subscriber
Plan type:
Administrative Services Only
Cost-Plus Contracts
Federal Employee Program
National Programs
High Insurance Risk Sharing
Other BCBS plans
County characteristics
High school and over
Population density
Unemployment rate
Personal income per capita
Medical assist per capita
Birth rate
Death rate
Year dummies allowed to differ
between AOI and ROS
Δ from 1988-95 in the AOI
Δ from 1988-95 in the ROS
Difference-in-difference: AOI-ROS
s.e.
Coeff.
s.e.
Price deviation
Coeff.
s.e.
-138.4*
4.95
-141.4*
4.85
3.0*
0.51
-30.4*
-2.2
147.0*
521.9*
1163.4*
7.36
8.16
8.33
10.24
13.32
-40.1*
-22.2*
126.1*
498.4*
1137.5*
7.25
8.01
8.20
10.07
13.05
9.7*
20.0*
20.9*
23.6*
25.9*
0.78
0.99
1.02
1.20
1.79
-88.3*
-145.5*
101.7*
350.5*
329.3*
496.9*
768.7*
-50.9*
-96.4*
-113.6*
5.94
4.98
6.07
7.67
7.95
8.88
10.38
12.95
13.08
13.27
-87.6*
-148.8*
91.5*
332.5*
307.8*
475.5*
749.8*
-48.4*
-94.1*
-127.2*
5.80
4.87
5.96
7.54
7.81
8.72
10.21
12.59
12.71
12.91
-0.7
3.3*
10.2*
18.0*
21.4*
21.4*
18.8*
-2.4
-2.4
13.6*
0.61
0.52
0.77
0.97
0.99
1.09
1.25
1.66
1.67
1.70
5.4
-10.0+
611.6*
-117.6*
1489.0*
-58.0*
4.31
5.64
19.92
6.92
44.16
3.76
11.1*
-10.9*
578.0*
-105.7*
1451.5*
-66.5*
4.24
5.59
19.39
6.82
42.71
3.68
-5.6*
0.9
33.6*
-12.0*
37.4*
8.5*
0.57
0.75
2.46
0.97
5.88
0.47
-292.8*
0.017*
5.9*
11.5*
21.2*
5.8
14.7
Yes
91.79
0.003
2.26
1.18
10.57
17.64
17.58
-141.9
0.008*
5.8*
7.6*
-1.8
25.0
25.3
Yes
89.97
0.003
2.26
1.15
10.49
17.39
17.37
-150.8*
0.009*
0.1
3.9*
22.9*
-19.2*
-10.6*
Yes
313.6*
21.71
248.4*
20.70
65.2*
2.62
231.0*
8.41
199.4*
8.30
31.6*
1.16
82.6*
20.89
49.0*
19.86
33.6*
2.52
11.96
0.001
0.32
0.15
1.44
2.55
2.31
Intercept
334.9*
58.98
435.3*
57.92
-100.4*
7.76
Adj. R-squared
0.0406
0.0413
0.006
Mean of dep. variable
831.7
830.8
0.862
Notes: *= significant at a 5% level or better. += significant at 10% level or better. n=2,261,766.
Heteroskedasticity-robust standard errors in parentheses. The omitted age/gender category is
male under 5 years.
25
Table 5. Estimated effects of competition-related variables: Alternative specifications
Total annual costs
Coeff.
s.e.
Quantity index
Coeff.
s.e.
Price deviation
Coeff.
s.e.
(A) Basic difference-in-difference
Differential increase in the AOI,
1988-95
82.6*
20.89
49.0*
19.86
33.6*
2.52
82.7*
21.24
44.2*
20.22
38.5*
2.58
0.009*
120.7*
0.002
17.63
0.002
17.12
0.007*
133.9*
0.002
2.37
83.9*
21.28
47.5*
20.26
36.2*
2.59
0.006+
0.006
119.9*
0.003
0.006
17.62
-0.007*
0.019*
-15.6
0.003
0.005
17.13
0.013*
-0.013*
135.5*
0.001
0.001
2.38
105.7*
23.93
59.57*
22.95
46.17*
2.99
0.011*
66.2+
0.003
36.47
0.007*
-36.02
0.003
35.80
0.004*
102.26*
0.001
5.09
(b) Adding HHI and HMO enrollment
Differential increase for the AOI,
1988 vs. 1995
HHI
HMO enrollment
0.002
-13.2
(C) Adding HHI with a spline for
HHI>2500, and HMO enrollment
Differential increase for the AOI,
1988-95
HHI
(HHI>2500)*HHI
HMO enrollment
(D) Adding HHI and HMO enrollment,
confining analysis to counties with
pop. density<200/sq. mi.
Differential increase for the AOI,
1988 vs. 1995
HHI
HMO enrollment
Notes: *= significant at a 5% level or better. += significant at 10% level or better. All regressions
include individual and county-level characteristics as explanatory variables. The number of
observations is 2,261,766 in specifications (A)-(C) and 619,932 in (D). Heteroskedasticity-robust
standard errors in parentheses.
26
References
Abadie, Alberto (2005) Semiparametric difference-in-difference estimators, Review of Economic
Studies, 72(1): 1-19.
Alemayehu, Berhanu and Kenneth E Warner (2004) The Lifetime Distribution of Health Care Costs,
Health Services Research, 39(3): 627–642.
Allard, Marie, Pierre Thomas Leger, and Lise Rochaix (2009). "Provider Competition in a Dynamic
Setting." Journal of Economics and Management Strategy, 18(2): 457-486.
American Bar Association (1996) Proving Antitrust Damages (Chicago, IL: American Bar Association).
Aizcorbe, Ana and Nicole Nestoriak (2011). “Changing Mix of Medical Care Services: Stylized Facts and
Implications for Price Indexes.” Journal of Health Economics, 30(3): 568–574.
Area Resource File (ARF) (2004) US Department of Health and Human Services, Health Resources and
Services Administration, Bureau of Health Professions, Rockville, MD.
Associated Press (1997) Marshfield Clinic to pay $4 million under settlement, Milwaukee Journal
Sentinel (Oct. 25): 2D.
Baker, Laurence (1994) Does Competition from HMOs Affect Fee-For-Service Physicians? NBER
Working Paper No. 4920.
Baker, Laurence and Kenneth S. Corts (1995) The Effects of HMOs on Conventional Insurance
Premiums: Theory and Evidence. NBER Working Paper No. 5356.
Berndt, Ernst, David M. Cutler, Richard Frank, Zvi Griliches, Joseph P. Newhouse, and Jack E. Triplett
(2001). Price Indexes for Medical Care Goods and Services: An Overview of Measurement Issues. In
David Cutler and Ernst Bernt, eds., Medical Care Output and Productivity, pp. 141-200. (Chicago, IL:
University of Chicago Press for the NBER).
Blair, Roger D. and James M. Fesmire (1994) The Resale Price Maintenance Policy Dilemma, Southern
Economic Journal, 60: 1043-7.
Bork, Robert H. (1978) The Antitrust Paradox: A Policy at War With Itself (New York: Free Press).
Capps, Cory, David Dranove, and Mark Satterthwaite (2003). Competition and Market Power in Option
Demand Markets. RAND Journal of Economics, 34(4): 737-763.
Cohen, Sheldon (2004) Social relationships and health, American Psychologist, Nov.: 678-684
Comanor, William S. (1985) Vertical Price-Fixing, Vertical Market Restriction, and the New Antitrust
Policy, Harvard Law Review, 98: 983-1002.
Coombs, Jan G., (2005) Rise and Fall of HMOs: An American Health Care Revolution (Madison, WI:
University of Wisconsin Press).
Easterbrook, Frank H. (1984) The Limits of Antitrust, Texas Law Review, 63(1): 1-40.
Emanuel, Ezekiel and Victor Fuchs (2008) The Perfect Storm of Overutilization, Journal of the
American Medical Association, 299(23): 2789-2791.
27
Feldstein, Martin (1973) The Welfare Loss of Excess Health Insurance, Journal of Political Economy,
81(2): 251-280.
Frech III, H.E., James Langenfeld and R. Forrest McCluer (2004) The Sensitivity of Elzinga-Hogarty
Tests and Alternative Approaches for Market Share Calculations in Hospital Markets, Antitrust Law
Journal, 71(3): 921-947.
Gaynor, Martin (2006) What do we know about competition and quality in health care markets? NBER
Working Paper No. 12301.
Gaynor, Martin, and William Vogt (2000) Antitrust and Competition in Health Care Markets. In A. J.
Culyer and J. P. Newhouse, eds., Handbook of Health Economics, Vol. 1B, pp. 1460-1487
(Amsterdam: North Holland).
Greenberg, Warren. (1998) Marshfield Clinic, Physician Networks, and the Exercise of Market Power,
Health Services Research, 33(5):1461-1476.
Grossman, Michael (2000) The Human Capital Model. In A.J. Culyer and J.P. Newhouse, eds.,
Handbook of Health Economics, Vol. 1, pp. 348-408 (Amsterdam: North Holland).
Haas-Wilson, Deborah (2003) Managed Care and Monopoly Power: The Antitrust Challenge.
Cambridge, MA: Harvard University Press.
Haas-Wilson, Deborah and Martin Gaynor (1998) Increasing consolidation in healthcare markets: What
are the antitrust policy implications? Health Services Research, 33(5): 1403-1419.
Hammer, Peter J., and William M. Sage (2002) Antitrust, Health Care Quality, and the Courts,
Columbia Law Review, 103(3): 545-649.
Ho, Katherine (2009) Insurer-Provider Networks in the Medical Care Market, American Economic
Review, 99(1): 393-430.
Iverson, Tor and Albert Ching-to Ma (2011) Market conditions and general practitioners’ referrals,
International Journal of Health Care Finance and Economics, 11(4): 245-265.
Landes, William M. and Richard A. Posner (1981) Market Power in Antitrust Cases, Harvard Law
Review, 94(5): 937-996.
Lynk, William J. (1995) Non-Profit Hospital Mergers and the Exercise of Market Power, Journal of Law
and Economics, 38(2): 437-462.
Ma, Ching-To Albert and Thomas G. McGuire (2002) Network Incentives in Managed Health Care,
Journal of Economics & Management Strategy, 11(1): 1-35.
McCluer, R. Forrest and Martha A. Starr (2013) Using Difference in Differences to Estimate Damages
in Healthcare Antitrust: A Case Study of Marshfield Clinic, International Journal of the Economics of
Business, 20(3): 447-469.
McCrary, Justin and Daniel L. Rubinfeld (2010) Measuring Benchmark Damages in Antitrust Litigation,
Paper presented in DG comp economist workshop October, 2010. Accessed electronically at
http://ec.europa.eu/competition/antitrust/actionsdamages/rubinfeld_mccrary.pdf, 12/12/2013.
McGuire, Thomas G. (2000) Physician Agency. In A. J. Culyer and J. P. Newhouse, eds., Handbook of
Health Economics, Vol. 1A, 461-536 (Amsterdam: North Holland).
Office of the Commissioner of Insurance, State of Wisconsin (various years) Wisconsin Insurance
Report, Wisconsin Market Shares, Table E. State of Wisconsin.
28
Parker-Pope, Tara (2010) Is marriage good for your health? New York Times Magazine (April 18), p.
46.
Pauly, Mark (1986) Taxation, Health Insurance, and Market Failure in the Medical Economy, Journal of
Economic Literature, 24(2): 629-675.
Rey, Patrick and Jean Tirole (2007) A Primer on Foreclosure. In Mark Armstrong and Rob Porter, eds.,
Handbook of Industrial Organization, Vol. 3, pp. 2145-2220 (Amsterdam: North Holland).
Robinson, James C. (2001) Theory and Practice in the Design of Physician Payment Incentives,
Milbank Quarterly, 79(2): 149-177.
Rubinfeld, Daniel (2010) Econometric Issues in Antitrust Analysis, Journal of Institutional and
Theoretical Economics, 66(1): 62-77.
Ruhm, Christopher (2000) Are Recessions Good For Your Health? Quarterly Journal of Economics,
115(2): 617-650.
Sage, William (1997) Judge Posner's RFP: Antitrust Law and Managed Care, Health Affairs 16(6): 4461.
Salop, Steven C. (2005) Anticompetitive Overbuying by Power Buyers, Antitrust Law Journal, 72: 669715.
Schmidt, Donald R. (1999) Evolving Relevant Market Concepts: Product Market. In Douglas Ross, ed.,
Antitrust and health care: insights into analysis and enforcement, pp. 99-118. (Chicago, IL: American
Bar Association).
Schneider, John, Pengxiang Li, Donald Klepser, N. Andrew Peterson, Timothy Brown and Richard
Scheffler (2008) The effect of physician and health plan market concentration on prices in commercial
health insurance markets, International Journal of Health Care Finance and Economics, 8(1): 13-26.
Town, Robert and Gregory Vistnes (2001) Hospital Competition in HMO Networks, Journal of Health
Economics, 20(5):733-752.
Troupis, James R. (1995). The Marshfield Clinic Case: A Primer in Conspiracy, Antitrust Healthcare
Chronicle, 9(3): 2.
U.S. Department of Justice and Federal Trade Commission (2010). Horizontal Merger Guidelines (Aug.
19). Accessed electronically at <http://www.justice.gov/atr/public/guidelines/hmg-2010.html#5c
on>, on 4/27/2013.
Vogt, William and Robert Town (2006) How has hospital consolidation affected price and quality of
hospital care? Robert Wood Johnson Foundation, Synthesis Project Issue No. 9 (Feb.).
http://www.rwjf.org/pr/product.jsp?id=15231
Wisconsin Legislative Reference Bureau (2007) Wisconsin Blue Book. (Madison, WI: Joint Committee
on Legislative Organization).