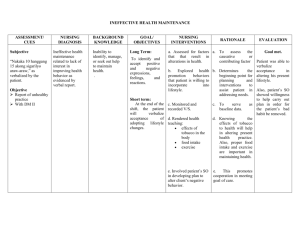
Cardiovascular Disorders Nursing Care Plan for Patients with Congestive Heart Failure
advertisement
1 الدكتور عبد المهدي عبد الرضا حسن PhD, child psychiatry Cardiovascular Disorders Nursing Care Plan for Patients with Congestive Heart Failure Nursing Diagnosis Decreased Cardiac Output related to impaired contractility and increased preload/after load Maintaining Adequate Cardiac Output 1. Place patient at physical and emotional rest to reduce work of heart. . a. Provide rest in semi recumbent position or in armchair in air- conditioned environment reduces work of heart, increases heart reserve, reduces blood pressure, decreases work of respiratory muscles and oxygen utilization, improves efficiency of heart contraction; recumbency promotes diuresis by improving renal perfusion. b. Provide bedside commode to reduce work of getting to bathroom and for defecation. stress produces vasoconstriction, elevates c. Provide for psychological rest emotional arterial pressure, and speeds the heart. 1. Promote physical comfort. 2. Avoid situations that tend to promote anxiety/agitation. 3. Offer careful explanations and answers to the patient's questions. 2. Evaluate frequently for progression of left ventricular failure. Take frequent blood pressure readings. Observe for lowering of systolic pressure. Note narrowing of pulse pressure. c. Note alternations in strong and weak pulsations (pulsus alternans). 3. Auscultate heart sounds frequently. a. Note presence of S3 Or S4 gallop (S3 gallop is a significant indicator of congestive heart failure). b. Monitor for premature ventricular beats. 4. Observe for signs and symptoms of reduced peripheral tissue perfusion: cool temperature of skin, facial pallor, poor capillary refill of nailbeds. Administer pharmacotherapy as directed. 5. Monitor clinical response of patient with respect to relief 2 symptoms (lessening dyspnea and orthopnea, decrease in crackles, relief of peripheral edema). Impaired Gas Exchange related to alveolar edema due to elevated ventricular pressures Nursing Goals & Interventions 1. Raise head of bed 20 to 30 cm (8-10 in) reduces venous return to heart and lungs; alleviates pulmonary congestion. a. Support lower arms with pillows to eliminate weight on shoulder muscle b. Sit orthopneic patient on side of bed with feet support chair, head and arms resting on an over-the-bed table, lumbosacral area supported with pillows. 2. Auscultate lung fields every 4 hours for crackles and wheezes in dependent lung fields (fluid accumulates in areas affected by gravity). A. Mark with water-soluble ink the level on the patient's where adventitious breath sounds are heard. B. Use markings for comparative assessment during changes in tours of duty with other nursing personnel. 3. Observe for increased rate of respirations (could be indicative of falling arterial pH). 4. Observe for Cheyne—Stokes respirations (may occur in elderly because of a decrease in cerebral perfusion stimulating a neurogenic response). 5. Position the patient every 2 hours (or encourage the patient to change position frequently) to help prevent atelectasis and pneumonia. 6. Encourage deep-breathing exercises every 1 to 2 hours to avoid atelectasis. 7. Offer small, frequent feedings to avoid excessive gastric filling and abdominal distention with subsequent elevation of diaphragm that causes decrease in lung capacity. 8. Administer oxygen as directed. Fluid Volume Excess related to sodium and water retention Restoring Fluid Balance Administer prescribed diuretic as ordered. 2.Give diuretic early in the morning night time diuresis 3 volume of fluid after a single dose of diuretic. 3.Keep input and output record the patient may lose large controlled: weight loss 4.Weigh the patient daily to determine if edema is being should not exceed 0.45 to 2 lb/day). Assess for weakness, malaise, muscle cramps diuretic may produce hypovolemia and electrolyte depletion namely hypokalemia. Hypokalemia may cause weakening of cardiac contractions and may precipitate digitalis toxicity in the form of dysrhythmias. 6.Give oral potassium as prescribed. 7. Watch for problems associated with diuretic therapy including disorders of hyperuricemia, volume depletion, an( hyponatremia, magnesium depletion, hyperglycen diabetes mellitus. 8. Watch for signs of bladder distention in the elderly male with prostatic hyperplasia. lassitude, apathy, mental 9. Observe for symptoms of electrolyte depletion confusion, anorexia, decreasing urinary output, azotemia. 10.Limit intravenous fluid administration through use of heparin lock (allows for periodic drug administration without increasing excessive fluid intake). 11.Monitor for pitting edema of lower extremities and sacral area. Use "egg crate" mattress and sheepskin to prevent pressure sores (poor blood flow and edema increase susceptibility). (especially in 12. Observe for the complications of bed rest pressure sores edematous patients), phlebothrombosis, pulmonary embolism. 13.Be alert to complaints of right upper quadrant abdominal pain, poor appetite, nausea, and abdominal distention (may indicate hepatic and visceral engorgement). 14.Monitor the patient's diet. Diet may be limited in sodium to prevent, control, or eliminate edema; may also be limited in calories. 15. Caution patients to avoid added salt in food and foods with high sodium content. Activity Intolerance related to oxygen supply and demand imbalance Improving Activity Tolerance 1.Increase the patient's activities gradually. Alter or modify patient's activities to keep within the limits of his cardiac reserve 2.Assist the patient with self-care activities early in the day (fatigue sets in as day progresses). 3.Be alert to complaints of chest pain or skeletal pain during or after activities. 4.Observe the pulse, symptoms, and behavioral response activity. to 4 a. Monitor the patient's heart rate during self-care activity b.Allow heart rate to decrease to preactivity level before initiating new activity. 1. Note time lapse between cessation of activity and heart rate (decreased stroke volume causes immediate rise in heat rate ) 2.Document time lapse and revise patient care plan appropriate (progressive increase in time lapse may be indication of increased left ventricular failure). 3. Relieve night time anxiety and provide for rest and sleep-with congestive heart failure have a tendency to be restless at because of cerebral hypoxia with superimposed nitrogen retentiona. Give appropriate sedation—to relieve insomnia an restlessness. Patient Education 1.Explain the disease process to the patient; the term "failure" may have terrifying implications. 2.Explain the pumping action of the heart—"to move blood through the body to provide nutrients and aid in the removal of waste material." Explain the difference between "heart attack" and congestive heart failure. Teach the signs and symptoms of recurrence. Watch for: report weight gain of more than 2 to 3 pounds (0.9-1.4 kg) in a few days. Weigh at same time daily -Swelling of ankles, feet, or abdomen -Persistent cough -Tiredness; loss of appetite - Frequent urination at night 3.Review medication regimen. -Label all medications. -Give written instructions concerning pharmacologic therapy. -Make sure the patient has a check-off system that will show that he/she has taken medications. -Teach the patient to take and record pulse rate and blood pressure. -Inform the patient of the signs and symptoms of adverse drug effects. If the patient is taking oral potassium solution, it may be diluted with juice and taken after a meal. - Tell the patient to weigh self daily and log weight if on diuretic therapy. 4.Review activity program. Instruct the patient as follows: 5 -Increase walking and other activities gradually, provided they do not cause fatigue and dyspnea. -In general, continue at whatever activity level can be maintained without the appearance of symptoms. -Avoid excesses in eating and drinking. Undertake a weight reduction program until optimal weight is reached. work of the heart; air -Avoid extremes in heat and cold which increase conditioning may be essential in a hot, humid environment. 5.Restrict sodium as -Keep regular appointment with health care provider directed. Give patient a booklet containing sodium content of common foods from local chapter of American Heart Association. -Give patient a written diet plan with lists of permitted and restricted foods. -Advice patient to look at all labels to ascertain sodium content (antacids, laxatives, cough remedies, etc.). -Teach the patient to rinse the mouth well after brushing tooth cleansers and some mouthwashes contains amounts of sodium. Water softeners are to be avoided. -Teach the patient that sodium is present in alkalizers, cough remedies, laxatives, pain relievers, estrogens, and other drugs. -Encourage use of flavorings, spices, herbs, and lemon juice. Avoid salt substitutes in the presence of renal disease