Document 12467622
advertisement

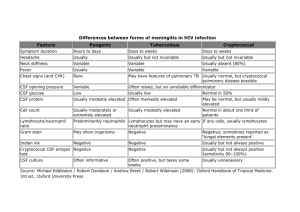
CrAg LFA: The New Gold Standard for Diagnosis and Prevention of Cryptococcal Disease Joy Pelfrey and Sean Bauman, Ph.D., IMMY, Norman, OK Intended Use Within the U.S. The CrAg Lateral Flow Assay is an immunochromatographic test system for the qualitaJve or semi-­‐quanJtaJve detecJon of the capsular polysaccharide anJgens of Cryptococcus species complex (Cryptococcus neoformans and Cryptococcus ga1i) in serum and cerebral spinal fluid (CSF). The CrAg Lateral Flow Assay is a prescripJon-­‐ use laboratory assay which can aid in the diagnosis of cryptococcosis. Outside the U.S. The CrAg Lateral Flow Assay is an immunochromatographic test system for the qualitaJve or semi-­‐quanJtaJve detecJon of the capsular polysaccharide anJgens of Cryptococcus species complex (Cryptococcus neoformans and Cryptococcus ga1i) in serum, plasma and cerebral spinal fluid (CSF). The CrAg Lateral Flow Assay is a prescripJon-­‐use laboratory assay which can aid in the diagnosis of cryptococcosis. Abstract: Cryptococcosis, a fungal disease caused by Cryptococcus species complex is one of the most common HIV-­‐ related opportunisJc infecJons. Every year, approximately 1,000,000 cases of cryptococcal meningiJs occur globally resulJng in more than 1,700 deaths every day. Cryptococcosis is most commonly diagnosed by detecJon of cryptococcal anJgen (CrAg) using one of several methods. The cryptococcal anJgen lateral flow assay (CrAg LFA) has been developed to have major advantages over exisJng methods. The CrAg LFA can detect all four CrAg serotypes with improved sensiJvity in detecJng C. ga1i infecJons (Serotype C). The CrAg LFA’s most notable advantage is its ease of use. The LFA is performed in 5 easy steps, and objecJve qualitaJve or semi-­‐quanJtaJve results are obtained within 10 minutes with no specimen pre-­‐treatment. The assay protocol allows for any number of specimens to be tested one at a Jme, meeJng the needs of both the small-­‐ and large-­‐volume laboratories. When compared to culture, the CrAg LFA had 100% sensiJvity and 94% specificity. When compared to other CrAg immunoassays (latex aggluJnaJon and enzyme immunoassays), the CrAg LFA had an overall percent agreement posiJve of 98.5% and percent agreement negaJve of 98.3%. Since it has significant clinical and procedural advantages over all other diagnosJc tests, the CrAg LFA should be considered the new gold standard for the diagnosis of cryptococcal disease. 1 of 18 High Burden of Cryptococcal Disease Cryptococcosis, a fungal disease caused by Cryptococcus species complex (Cryptococcus neoformans and Cryptococcus ga1i), is one of the most common HIV-­‐related opportunisJc infecJons (42). Cryptococcal infecJon begins with inhalaJon of small desiccated yeast cells from environmental sites establishing a localized pulmonary infecJon. In immunocompromised paJents, the yeast cells can disseminate from the lungs to the central nervous system to produce cryptococcal meningiJs. Globally, approximately 1,000,000 incident cases of cryptococcal meningiJs occur each year resulJng in more than 600,000 deaths every year or more than 1,700 deaths every day (42). These esJmates bring to light the tremendous burden of cryptococcal disease. In fact, in sub-­‐Saharan Africa, where the burden is greatest (Figure 1A), deaths associated with cryptococcal disease are higher than tuberculosis among HIV paJents (Figure 1B). Despite cryptococcal disease accounJng for 13 – 44% of deaths in HIV-­‐infected paJents (7,14,39), cryptococcal disease conJnues to be grossly under-­‐recognized and underdiagnosed. The World Health OrganizaJon noted that the main reason for the unacceptably high mortality is a delay in presentaJon when meningiJs is advanced and treatment is less effecJve (61). If diagnosis could be made earlier, the burden of cryptococcal disease may be drasJcally reduced. Figure 1. (A) Global burden of cryptococcal meningi:s. (B) Es:mated causes of death from infec:ous disease in sub-­‐ Saharan Africa, excluding HIV [Adapted from (42)] 2 of 18 Cryptococcal An8gen: The Surrogate Marker for Diagnosis of Cryptococcal Disease The three pillars for diagnosis of cryptococcosis have been culture of body fluids, microscopy (India ink stain) of cerebral spinal fluid for encapsulated yeast, and immunoassays for cryptococcal anJgen (CrAg) detecJon (27). Culture may have poor sensiJvity, can take several days to obtain a result, and requires laboratory infrastructure (33,45,58). Microscopy lacks sensiJvity and requires experienced laboratory personnel (45). Kambugu et al. reported results from CSF evaluaJon of 136 paJents with cryptococcal meningiJs; 83% had posiJve cryptococcal cultures, 84% had posiJve microscopy and 100% had posiJve CSF CrAg tests (3,25). Given the limitaJons of culture and microscopy, immunoassay for CrAg detecJon is the most widely uJlized diagnosJc method (33,58,61). During a cryptococcal infecJon, cryptococcal anJgen (CrAg) is shed into bodily fluids, such as blood (serum, plasma, and whole blood), urine and CSF (Figure 2). The concentraJon of CrAg in each of these specimen types is dependent on the stage of disease. Furthermore, the presence of CrAg has been found greater than 100 days before disease onset in 11% of the people who develop cryptococcal disease (14). Finding paJents who are CrAg-­‐posiJve but asymptomaJc offers an opportunity to drasJcally reduce mortality associated with cryptococcal disease through pre-­‐empJve therapy. Fig. 2. SchemaJc temporal sequence of CrAg concentraJon in body fluids during progression of disease from pulmonary infecJon to meningiJs (14,20,24,33). There are currently seven commercially available immunoassays for the detecJon of cryptococcal anJgen: IMMY Lateral Flow Assay (LFA), IMMY Latex AggluJnaJon (LA), IMMY Enzyme Immunoassay (EIA), Meridian LA, Meridian EIA, Remel LA, and Bio-­‐Rad LA. The FDA 510(k)-­‐cleared CrAg LFA was developed to enable earlier and more reliable diagnosis of both C. neoformans and C. ga1i infecJons compared to other diagnosJc methods. Studies have shown that the LFA is, in fact, more sensiJve than other CrAg detecJon systems, especially when detecJng serotype C (C. ga1i) (28,44,50). 3 of 18 CrAg LFA: Best Method for Diagnosis of Cryptococcal Disease CrAg LFA in Resource-­‐Limited Sekngs Clinicians in developing countries are olen unable to diagnose cryptococcal disease partly because they do not have access to laboratories with adequate infrastructure needed to run convenJonal diagnosJc methods such as LA and EIA. Unlike all other available tests for the diagnosis of cryptococcal disease, the CrAg LFA requires limle or no laboratory infrastructure and meets all of the WHO ASSURED criteria (Table 2). Only 28% of paJents in sub-­‐Saharan Africa have access to health care with moderate or advanced infrastructure (Table 3) (16). Table 2. CrAg LFA Meets all of the WHO ASSURED CharacterisJcs LFA LA EIA India Ink Culture $2-­‐4/test $2-­‐4/test $4-­‐6/test <$1/test <$1/test Sensi:ve ++++ +++ +++ ++ +++ Specific ++++ +++ +++ +++ ++++ User Friendly ++++ ++ + ++ ++ Rapid/Robust ++++ ++ + + + Equipment-­‐Free ++++ + + + + Delivered ++++ ++ + ++ ++ Affordable Table 3. Access to Health Care Country # Living with HIV (MM)* South Africa 5.7 Access to Minimal Infrastructure Access to Moderate/Advanced (%) Infrastructure (%) 13 86 Nigeria 2.6 62 23 India 2.4 39 47 Mozambique 1.5 73 12 Tanzania 1.4 66 17 Kenya 1.3 59 25 Zimbabwe 1.3 5 95 Zambia 1.1 78 11 Uganda 0.9 59 14 Adapted from RAND (2006) WR-­‐423-­‐HLTH. Minimal laboratory infrastructure includes rural and urban clinics. Moderate to advanced laboratory infrastructure includes rural and urban hospitals. *# living with HIV in millions (2008) WHO/UNAIDS Table 4. Specimen Types and Laboratory Infrastructure Required for Cryptococcal Diagnos:c Assays Laboratory Infrastructure No Infrastructure (1) Minimal Lab Infrastructure (2) Moderate to Advanced Infrastructure (3) LFA Urine Whole blood Urine Whole blood Urine Whole blood Serum Plasma CSF LA EIA India Ink Culture Not possible Not possible Not possible Not possible Not possible Not possible Not possible Not possible Serum CSF Serum CSF CSF CSF Blood (1) Home or village; requires no expertise to use (2) Rural clinic without electricity or water by staff with minimal training (3) Hospital or urban clinic with well-equipped laboratories and trained clinicians 4 of 18 CrAg LFA: The Simplest Method for Diagnosis of Cryptococcal Disease Qualita8ve Test Method One major advantage of the CrAg LFA over other currently available cryptococcal anJgen detecJon assays such as LA or EIA is its ease of use. Aler five easy steps, results are obtained in 10 minutes (Figure 3). The LFA does not require specimen pre-­‐treatment, it does not require equipment, and it is easily scaled up to handle 30 samples or more. Fig. 3. Five easy steps are all that is required to perform the CrAg LFA. Step 1: Add one drop of specimen to a tube. Step 2: Add of 40 ul of paJent specimen to the tube. Step 3: Insert the CrAg LFA strip into the tube. Step 4: Incubate for 10 minutes. Step 5: Interpret results. 5 of 18 Semi-­‐Quan8ta8ve Test Method The CrAg LFA is also semi-­‐quanJtaJve. By performing ten simple diluJons of paJent specimen, Jters can be determined. A three-­‐step Jter protocol has been developed to minimize the number of test strips used, therefore reducing the cost of Jter determinaJon (Figure 4). Figure 4. Three-­‐step Jter protocol used to minimize number of tests performed 6 of 18 CrAg LFA: Superior Sensi8vity & Specificity CrAg LFA: Analy8cal Serotype Sensi8vity Cryptococcal anJgen, termed glucuronoxylomannan (GXM), occurs in four major serotypes (A, B, C and D). The species complex of pathogenic cryptococci includes C. neoformans and C. ga1i (reviewed in (34)). The species and varieJes of Cryptococcus differ in the structures of their cryptococcal anJgens. C. neoformans var. grubii (serotype A) has a global distribuJon and accounts for more than 90% of all cases of cryptococcosis (34)). C. neoformans var. neoformans (serotype D) also has a global distribuJon, but cases are concentrated in Europe (11,29). C. ga1i (serotypes B and C) has a distribuJon in tropical areas of Australia, Asia, Africa and the Americas (29), and is currently the cause of an ongoing U.S. outbreak that began in Vancouver Island, BriJsh Columbia (19). The analyJcal serotype sensiJviJes for the IMMY CrAg LFA, IMMY LA, Meridian CALAS LA and the Meridian Premier ELISA were compared using purified CrAg from mulJple strains of four serotypes of Cryptococcus. The serotype sensiJvity was the lowest concentraJon of CrAg that could be detected in each assay. The analyJcal sensiJvity of the CrAg LFA was found to be superior to that of the LA or ELISA by as much as 200-­‐fold (Table 5). SensiJviJes of four commercially available CrAg immunoassays for detecJon of CrAg of different serotypes are shown below (adapted from (28,44,51)). Table 5. Serotype SensiJviJes for CrAg DetecJon Systems Assay formata Manufacturer A Serotype Sensi:vity (CrAg ng/ml)b B C D IMMY LFA 1 1 9 8 IMMY LA 28 47 380 62 Meridian CALAS LA 19 37 940 54 23 >2,000c 770 Meridian Premier ELISA 28 aLFA, lateral flow assay; LA, latex agglu:na:on; ELISA, an:gen capture sandwich enzyme-­‐linked immunosorbent assay bMinimum concentra:on of CrAg (ng/ml) producing a posi:ve result. Results are the average results for CrAg isolated from different strains of each serotype. c >2,000, CrAg of some strains of serotype C produced nega:ve results at all concentra:ons up to 2,000 ng/ml. CrAg LFA: Clinical Sensi8vity and Specificity MulJple studies have been performed to evaluate the sensiJvity and specificity of the CrAg LFA using serum, plasma, CSF, and urine specimens, compared to culture (4,24,33,50). Below is a summary table of the published studies to date and the resulJng staJsJcs (Table 6). Overall, the CrAg LFA is 99.5% sensiJve and 98.8% specific when compared to culture. There was a total of 13 LFA posiJve/culture negaJve specimens. Given the culture method’s lack of sensiJvity (13,53), it is presumed that these specimens were true cryptococcosis cases. There was a total of 3 LFA-­‐negaJve/culture-­‐posiJve specimens, all of which were urine specimens. This is most likely due to reduced levels of cryptococcal anJgen being shed into urine (24). AddiJonal studies are necessary to fully evaluate the detecJon of CrAg in urine. It is important to note both the high posiJve and negaJve predicJve values, showing the CrAg LFA’s uJlity as an effecJve tool for both diagnosis and screening. Table 6. SensiJvity and Specificity of the CrAg LFA Compared to Cryptococcal Culture Specimen Type n Sensi8vity 95% CI Specificity 95% CI PPV 95% CI NPV 95% CI References Serum Plasma 693 135 100% 100% 98-­‐100% 96-­‐100% 99% 100% 97-­‐99% 93-­‐100% 97% 100% 94-­‐99% 96-­‐100% 100% 100% 99-­‐100% 97-­‐100% (4,24,33,35) (9,29) CSF 100% 98.4% 97-­‐100% 95-­‐99.5% 97% 99% 92-­‐99% 98-­‐99.8% 97% 98% 93-­‐99% 95-­‐99.7% 100% 99% 97-­‐100% 98-­‐99.9% (4,50) Urine 261 674 TOTAL 1763 99.5% 98-­‐99.8% 99% 98.0-­‐99% 98% 96-­‐99% (4,24,33,35) 99.7% 99.2-­‐99.9% 7 of 18 CrAg LFA: Mul8ple Specimen Types The CrAg LFA has been evaluated with paired specimens from persons with cryptococcal disease (Table 7). As expected, since the presence of CrAg is dependent on disease progression, CrAg was found in serum but not CSF of some paJents, indicaJng non-­‐meningeal cryptococcal disease. It was also found that CrAg concentraJons in urine are lower than in serum, plasma, or CSF, as seen by urine LFA-­‐negaJve results when serum, plasma, and CSF are posiJve. Table 7. CrAg LFA Paired Specimen Comparisons from Persons with Cryptococcal Disease Serum vs. Urine 169 % Agreement Posi8ve 97.8% Serum vs. Plasma 83 100% 95-­‐100% 100% 34-­‐100% (4,24) Serum vs. CSF 118 93.7% 89-­‐97% 100% 91-­‐100% (4) Plasma vs. Urine 81 98.8% 93-­‐100% N/A N/A (4,24) CSF vs. Urine 104 98.5% 92-­‐100% 91.7% 78-­‐97% (4) CSF vs. Plasma 18 100% 82-­‐100% N/A N/A (4) Comparison n 95% CI References 94-­‐99% % Agreement Nega8ve 100% 89-­‐100% (4,24) 95% CI In addiJon to high overall agreements between the different specimen types when performing qualitaJve, diagnosJc tesJng, there is also high correlaJon between specimen type Jters when performing semi-­‐ quanJtaJve tesJng (Figure 5)(24). It is important to note that the urine Jters were consistently lower than the serum and plasma Jters, indicaJng lower concentraJons of CrAg are shed into urine. Figure 5. Correla:ons of CrAg :ters between serum, plasma, and urine :ters using CrAg LFA. A) Correla:on between serum and plasma :ters; B) Correla:on between serum and urine :ters; C) Correla:on between plasma and urine :ters. Correla:on was calculated using Spearman rank-­‐order correla:on. 8 of 18 CrAg LFA: Comparison to Other CrAg Immunoassays Qualita8ve Comparison The CrAg LFA has also been evaluated at mulJple sites to evaluate its performance compared to other commercially available CrAg immunoassays (Tables 8 and 9). Overall, percent agreements posiJve and negaJve were 99% and 98%, respecJvely, when compared to other CrAg immunoassays. Considering the high percent agreement with other CrAg immunoassays and that the CrAg LFA is the only CrAg immunoassay to meet all of the WHO ASSURED criteria the CrAg LFA should be the method of choice for detecJon of cryptococcal anJgen. Table 8. Comparison of the CrAg LFA to Latex AggluJnaJon Assays Specimen Type Percent Agreement Posi8ve (n) 261 Serum (n=197) CSF (n=64) Meridian LA 421 Meridian LA 632 Meridian LA 76 Remel LA 124 Wampole LA 102 CSF Wampole LA 112 Plasma 1652 Serum/Plasma (n=1476) CSF (n=176) CrAg LFA Compared to: n IMMY LA Total 95% CI Percent Agreement Nega8ve (n) 95% CI Reference 99% (125/126) 96-­‐100% 99% (133/135) 95-­‐100% (59) Serum 100% (16/16) 81-­‐100% 95-­‐98% (12) Serum 100% (7/7) 65-­‐100% 99-­‐100% (2) 100% (13/13) 77-­‐100% 89-­‐99% (8) 94-­‐100% (21) Serum (n=55) CSF (n=21) Serum (n=114) CSF (n=10) 100% (16/16) 100% (56/56) 81-­‐100% 97% (392/405) 99.8% (624/625) 97% (61/63) 98% (106/108) 94-­‐100% 94% (43/46) 84-­‐98% (50) 99% (64/65) 92-­‐100% 92% (43/47) 80-­‐97% (50) 99% (284/286) 98-­‐100% 98% (1341/1366) 97-­‐99% N.A. 95% CI Reference Table 9. Comparison of the CrAg LFA to CrAg Enzyme Immunoassays (EIA) CrAg LFA Compared to: n IMMY EIA 1000 Meridian EIA 1000 Meridian EIA 633 Meridian EIA 261 Meridian EIA 464 Meridian EIA 610 Total 3968 Specimen Type Serum (n=589) CSF (n=411) Serum (n=589) CSF (n=411) Serum Percent Agreement Posi8ve (n) 95% CI Percent Agreement Nega8ve (n) 97% (76/78) 91-­‐99.3% 99.9% (921/922) 99.4-­‐100% (17) 100% (56/56) 94-­‐100% 98% (921/944) 96-­‐98% (17) 100% (4/4) 44-­‐100% 99.2% (624/629) 98-­‐99.7% (2) 97-­‐100% 95% (134/141) 90-­‐98% (IMMY In-­‐house data) 95.6% (87/91) 89-­‐98% 99.5% (371/373) 98-­‐100% (33) 100% (83/83) 96-­‐100% 97.5% (514/527) 96-­‐99% (30) 99% (426/432) 97-­‐99% 99% (3485/3536) 98-­‐99% N.A. Serum (n=197) CSF 100% (120/120) (n=64) Serum Serum (n=209) CSF (n=401) Serum (n=2681) CSF (n=1287) 9 of 18 Semi-­‐quan8ta8ve Comparison The CrAg LFA is a valuable tool for measuring CrAg Jters. Studies performed to evaluate the relaJonship between LA and LFA Jters using CSF and Serum showed strong correlaJons (Spearman’s rho = 0.93 for CSF and 0.740 for serum) between the two assays’ Jters (50) (Figure 6). Moreover, the LFA has been found to be at least 5-­‐fold more sensiJve than latex aggluJnaJon (48) indicaJng that an LA Jter of 1:8 would be comparable to an LFA Jter of 1:40. More importantly, this 5-­‐fold increase in sensiJvity implies that a specimen with a 1:5 Jter in the LFA has the potenJal to be negaJve in a latex aggluJnaJon test. Figure 6. Correla:on between CrAg LFA :ter and LA :ter. A) CSF (50) B) Serum (10). In another study, when comparing paJent serum Jters using Meridian’s EIA and the LFA, the LFA was found to be seven Jmes more sensiJve. In other words, a specimen with an approximate Jter of 1:7 in the LFA will be negaJve in the EIA (Figure 7) (17). In fact, in that study, there were 22 Meridian EIA-­‐negaJve/LFA-­‐posiJve specimens. Eight of the discrepant specimens had adequate volume for tesJng on latex aggluJnaJon, of which 7 were posiJve by latex, suggesJng those specimens were true posiJves and therefore false negaJves in the Meridian EIA. The CrAg LFA Jter protocol uses a two-­‐stage approach to minimize the number of strips needed to determine Jter, and therefore reduce the overall cost associated with cryptococcosis paJent management. In this protocol, ten serial diluJons are made of the specimen. In the first stage, LFA strips are only placed in diluJon tubes number 4, 7, and 10. In the second stage, LFA strips are placed in the tubes between the last posiJve tube and the negaJve tube. (See Figure 4 in “The Simplest Method for Diagnosing Cryptococcal Disease” secJon above) Using this approach, only five or six LFA strips will be needed to perform a Jter determinaJon. Figure 7. Serum CrAg LFA :ters compared to Meridian EIA Titers An important piece of clinical data needed in paJent management is the CrAg Jter, which has prognosJc value (5,47,47,57). Studies have shown that high Jters (>1:1024) are predicJve of higher acute mortality (1,22) and high iniJal CrAg Jters typically correlate with fungal burden as measured by quanJtaJve culture (49). Most significant is the fact that the success of treatment for cryptococcal disease can generally be measured by the decline in CrAg Jters. Conversely, a rise in CrAg Jter indicates therapy failure or relapse. 10 of 18 CrAg LFA: Improved Pa8ent Outcomes CrAg LFA: Improved Diagnosis of Symptoma8c Cryptococcal Meningi8s Since the FDA clearance of CrAg LFA, the World Health OrganizaJon (WHO) released “Rapid Advice: Diagnosis, PrevenJon and Management of Cryptococcal Disease in HIV-­‐infected Adults, Adolescents and Children.” In its guidance, the WHO emphasizes the importance of early diagnosis as the means to reduce mortality caused by cryptococcosis, especially in the developing world, and recommends the use of LA or the LFA over culture and India ink (61). Importantly, the WHO noted that the LFA had several key advantages over LA. Those include lower cost, rapid turnaround Jme, limle required training, and performance with minimal laboratory infrastructure. Most importantly for developing countries, the CrAg LFA is the only test on the market that meets all of the WHO’s A.S.S.U.R.E.D. criteria, meaning it is an assay that can be easily implemented in developing world labs (Table 2). Because of its greater sensiJvity, specificity, and ease-­‐of-­‐use compared to culture, India ink, and LA, the proper implementaJon of the CrAg LFA into HIV paJent management has the potenJal to transform both cryptococcal disease diagnosis and prevenJon and ulJmately save hundreds of thousands of lives annually. For more informaJon on the global burden of cryptococcal disease and what is being done to prevent cryptococcal-­‐related deaths, visit www.preventcrypto.org. CrAg LFA: Preven8on of Cryptococcal Disease Reducing Mortality Associated With Cryptococcal Disease Given its tremendous global burden, it is necessary to focus efforts on reducing mortality from cryptococcal disease. Since cryptococcal disease is most olen associated with HIV, we can use data esJmaJng the number of persons living with HIV and the prevalence of presumpJvely cryptococcal disease-­‐posiJve paJents to idenJfy countries where the greatest impact can be made through the introducJon and implementaJon of improved diagnosJcs and pre-­‐empJve therapy (Table 10). It is important to note that the prevalence of cryptococcal disease in some countries is currently unknown, despite exceedingly high numbers of persons living with HIV in those countries. For example, Mozambique has 1.4 million people who are HIV-­‐posiJve, yet there are no cryptococcosis prevalence studies reported in literature. Such studies are necessary to assist clinicians in providing accurate diagnosis and to aid health care policy makers in implemenJng appropriate diagnosJc and treatment methods. Table 10. Serum CrAg Prevalence in Countries with >0.5 MM Persons with HIV Country # Living with HIV* CrAg Prevalence CrAg Prevalence References South Africa 5.6 MM 13%, 3.9% (22) (52) Nigeria 3.3 MM 12% (40) India 2.4 MM (15) Kenya 1.5 MM 3.2% (CD4 <200) 6.2%, 7% (26) (38) Mozambique 1.4 MM Unknown N.A. Tanzania 1.4 MM 5.1% (60) Zimbabwe 1.2 MM Unknown N.A. Uganda 1.2 MM (31) (36) (41) (43,55) Zambia 1.0 MM 8.8%, 5.8%, 10.7%, 19% Unknown Ethiopia 1.0 MM 9.8% (56) Malawi 0.9 MM Unknown N.A. Brazil 0.7 MM Unknown N.A. Cameroon 0.6 MM Unknown N.A. Thailand 0.5 MM 12.9%, 11%, 13.1% (18,33,46) N.A. *UNAIDS Report on the global AIDS epidemic, 2010: hrp://www.unaids.org/documents/20101123_globalreport_em.pdf 11 of 18 In addiJon to the countries with >0.5 MM persons with HIV in Table 1, the following countries are of interest because of their known serum CrAg prevalence: Cambodia [10.8%, (37)], Congo [12.2%, (9)], Peru [3.6%, (32)], Colombia [4% (12)] and Rwanda (4.2%, (54). Data suggests that targeted screening could be a valuable tool in combakng the global burden of cryptococcal disease. It has been shown that Cryptococcus is able to live in the body undetected, especially in HIV-­‐posiJve paJents (See “PrevenJon of Cryptococcal Disease” secJon below). By screening HIV-­‐posiJve paJents for cryptococcal anJgen (an indicator of cryptococcal infecJon) before beginning anJretroviral therapy, cryptococcal disease can be idenJfied before it progresses to cryptococcal meningiJs. When caught early, cryptococcal disease is easily treatable with oral fluconazole. The CrAg LFA is cleared by the US Food and Drug Administra8on (FDA) for serum and CSF specimens and CE marked for serum, plasma, and CSF. Urine specimens are undergoing clinical evalua8on and should be considered inves8ga8onal use only. Numerous studies have shown that the CrAg LFA has a sensiJvity and specificity of greater than 99% and 98%, respecJvely. Through the implementaJon of a screen-­‐and-­‐treat protocol for cryptococcal disease, the CrAg LFA, in combinaJon with effecJve anJ-­‐fungal therapy, has the potenJal to save hundreds of thousands of lives each year. In fact, in their “Rapid Advice for Diagnosis, PrevenJon and Management of Cryptococcal disease in HIV-­‐Infected Adults, Adolescents, and Children,” the World Health OrganizaJon recommends the use of the CrAg LFA in sekngs where screening for unidenJfied cryptococcosis is being considered (61). AddiJonally, in the beginning of 2012, the US Centers for Disease Control and PrevenJon (CDC) put out a call to acJon “to equip half of all HIV clinics in Africa and Asia to perform Cryptococcus tesJng and treatment, which could save 50,000 to 100,000 lives every year. Early idenJficaJon of cryptococcal-­‐infected paJents in resource-­‐limited sekngs may lead to more Jmely treatment, reduced mortality due to cryptococcal meningiJs, and overall improved quality of life.” (6). Pre-­‐Emp8ve Therapy/Screen and Treat Clinical Relevance of AsymptomaJc AnJgenemia The first step in the prevenJon of cryptococcal disease is to idenJfy paJents at high risk for the disease, before they present with cryptococcal meningiJs (CM) since treatment for CM is olen unavailable and ineffecJve. RetrospecJve cohorts have shown that the presence of CrAg anJgenemia in asymptomaJc HIV-­‐posiJve paJents enrolling in ART independently predicts mortality (22,31). One study found that CrAg Jter > 1:8 using latex aggluJnaJon had a sensiJvity and specificity of 100% and 96%, respecJvely, for predicJng CM within one year (22). Treatment for pre-­‐meningiJs (asymptomaJc and pulmonary) cryptococcal disease is very effecJve and readily available through free drug programs (See Pfizer’s Diflucan® Partnership Program website: hmp:// www.directrelief.org/DiflucanPartnership/EN/DiflucanProgramOverview.aspx). Therefore, diagnosis prior to the onset of CM symptoms is criJcal in reducing the mortality associated with cryptococcal disease. 12 of 18 Screen and Treat Strategy A targeted CrAg screening approach to reduce cryptococcal disease mortality is quickly gaining momentum in areas of high HIV prevalence. This approach, termed “Screen and Treat,” uses targeted CrAg screening of HIV-­‐ posiJve paJents with CD4 counts less than 100 cells/ul. Based on retrospecJve studies, it is believed that this targeted screening can detect nearly all cryptococcal disease cases (22,23,25,31,36,37). When CrAg is found in asymptomaJc paJents, pre-­‐empJve therapy using fluconazole can begin, prevenJng the progression of the disease to meningiJs. Fluconazole is olen available free of cost in resource-­‐limited sekngs and unlike amphotericin b, it can be administered orally at home, making it more likely that paJents will complete treatment. Most importantly, the implementaJon of this screening protocol has been found to be cost-­‐ effecJve in areas were the CrAg prevalence is greater than 3% (Figure 8) (48). Currently used cryptococcal disease diagnosJc methods (culture, India ink, and latex aggluJnaJon) are not ideal for a screening program. Culture and India ink lack sensiJvity and specificity. Latex aggluJnaJon has excellent sensiJvity and specificity but is not pracJcal for screening implementaJon. Any screening strategy implemented in a hospital or urban clinic must uJlize a diagnosJc method that can easily test numerous specimens quickly. Also, implemenJng a screening strategy in rural clinics or in the field must uJlize an assay that does not require electricity. Latex aggluJnaJon does not fit either of these requirements. AlternaJvely, the CrAg LFA can be used to test over 30 specimens at one Jme, and it can be used in the field since it does not require electricity for either storage or for running the assay (27). Figure 8. Prevalence of asymptomaJc anJgenemia with corresponding cost per life saved based on LFA cost of $2.50 per test (48). Improved Outcomes of those with AsymptomaJc Cryptococcal AnJgenemia In one observaJonal cohort in Uganda, 295 people who had CD4 counts less than 100 cells/ul were screened for the presence of CrAg (36). Twenty-­‐six (8.8%) were found to be CrAg-­‐posiJve. Since asymptomaJc cryptococcal disease treatment was not standardized at the Jme of the cohort, therapies differed for the 26 CrAg-­‐posiJve paJents. Twenty-­‐one received fluconazole (200-­‐400 mg) for 2-­‐4 weeks while five paJents did not receive any anJ-­‐fungal therapy. Of the treated paJents, 30-­‐month survival was 71% while there were no survivors among the group who did not receive anJ-­‐fungal therapy. In another study performed in Kenya, fluconazole was given to 59% of CrAg-­‐posiJve paJents, and it was found that ART and fluconazole were significantly associated with improved survival (26). 13 of 18 Screen-­‐and-­‐Treat Algorithm Several screen-­‐and-­‐treat algorithms have been developed based on current knowledge of CrAg-­‐posiJve paJent populaJon and WHO and InfecJous Diseases Society of America (IDSA) guidelines. A representaJve algorithm can be found below (Figure 9). The pracJcality of the CrAg LFA makes it the test of choice when implemenJng this life-­‐saving screen-­‐and-­‐treat approach. Figure 9. South Africa Decision-­‐Making Guide for Cryptococcal Screening CrAg LFA: The New Gold Standard for Diagnosis and Preven8on of Cryptococcal Disease While currently considered the “gold standards” for the diagnosis of cryptococcosis, culture and India ink each lack both sensiJvity and specificity. CrAg detecJon using either latex aggluJnaJon (LA) or enzyme immunoassays (EIA) has improved sensiJviJes and specificiJes over culture and India ink. However, LA and EIA both have increased levels of complexity compared to culture and India ink, and they both have reduced sensiJviJes to serotype C. The CrAg Lateral Flow Assay (LFA) is not only extremely easy to perform, it is more sensiJve than culture, India ink, LA, and EIA. Accordingly, the CrAg LFA should be considered the new “gold standard” for the diagnosis of cryptococcal disease and should be the method of choice when implemenJng CrAg screen-­‐and-­‐treat programs in areas of high cryptococcal disease prevalence. 14 of 18 Addi8onal Resources: WHO’s Rapid Advice: Diagnosis, PrevenJon and Management of Cryptococcal Disease in HIV-­‐Infected Adults, Adolescents, and Children: hmp://whqlibdoc.who.int/publicaJons/2011/9789241502979_eng.pdf CDC’s website dedicated to prevenJng deaths due to Cryptococcus: hmp://www.cdc.gov/fungal/cryptococcosis/screening.html PrevenJon of Cryptococcal Disease Website: www.preventcrypto.org IMMY’s Website: www.immy.com Reference List 1. Anekthananon, T., W. Manosuthi, P. Chetcho:sakd, S. Kier:buranakul, K. Supparatpinyo, W. Ratanasuwan, P. G. Pappas, S. G. Filler, H. A. Kopetskie, T. L. Nolen, A. S. Kendrick, and R. A. Larsen. 2011. Predictors of poor clinical outcome of cryptococcal meningi:s in HIV-­‐infected pa:ents. Int.J.STD AIDS 22:665-­‐670. doi:22/11/665 [pii];10.1258/ijsa.2011.010538 [doi]. 2. Bestrom J.E., Jespersen D.J., Rollins L., and Binnicker M. An evalua:on of four commercial assays for the detec:on of crypotococcal an:gen. Abstract Pending . 2012. Ref Type: Abstract 3. Boulware, D. R. Personal communica:on. 11. 4. Boulware, D. R., Meya, D. B., Longley, N., Govender, N., Jarvis, J., Neary, B., Taseera, K., Chiller, T., Harrison, T., and Bauman, S. Mul:center evalua:on of a novel point-­‐of-­‐care assay for the detec:on of cryptococcal an:gen in HIV-­‐infected persons with and without cryptococcal meningi:s. Interscience Conference on An:microbial Agents and Chemotherapy Abstract . 2012. Ref Type: Abstract 5. Cachay, E. R., J. Caperna, A. M. Sitapa:, H. Jafari, S. Kandel, and W. C. Mathews. 2010. U:lity of clinical assessment, imaging, and cryptococcal an:gen :ter to predict AIDS-­‐related complicated forms of cryptococcal meningi:s. AIDS Res.Ther. 7:29. doi:1742-­‐6405-­‐7-­‐29 [pii];10.1186/1742-­‐6405-­‐7-­‐29 [doi]. 6. Centers for Disease Control and Preven:on. 2012. Preven:ng Deaths Due to Cryptococcus with Targeted Screening. Centers for Disease Control and Preven:on hrp://www.cdc.gov/fungal/cryptococcosis-­‐neoformans/screening.html. 7. Churchyard, G. J., I. Kleinschmidt, E. L. Corber, J. Murray, J. Smit, and K. M. De Cock. 2000. Factors associated with an increased case-­‐ fatality rate in HIV-­‐infected and non-­‐infected South African gold miners with pulmonary tuberculosis. Int.J.Tuberc.Lung Dis. 4:705-­‐712. 8. Clarke, S. and Gibb, R. Evalua:on of the IMMY CrAg Lateral Flow Assay for Detec:on of Cryptococcal An:gen. Australian Society of Microbiology Annual Mee:ng Abstract . 2012. Ref Type: Abstract 9. Desmet, P., K. D. Kayembe, and V. C. De. 1989. The value of cryptococcal serum an:gen screening among HIV-­‐posi:ve/AIDS pa:ents in Kinshasa, Zaire. AIDS 3:77-­‐78. 10. Doherty, B., Neary, B., Alami, S., and Bauman, S. Evalua:on of a novel lateral flow assay for the detec:on of cryptococcal an:gen in clinical specimens. Abstract Pending . 2012. Ref Type: Abstract 11. Dromer, F., S. Mathoulin, B. Dupont, L. Letenneur, and O. Ronin. 1996. Individual and environmental factors associated with infec:on due to Cryptococcus neoformans serotype D. French Cryptococcosis Study Group. Clin.Infect.Dis. 23:91-­‐96. 12. Escandon, P., Lizarazo, J., Agudelo, C. I., Chiller, T., and Castaneda, E. Evalua:on of a lateral flow immunoassay for the detec:on of cryptococcal an:gen for the early diagnosis of cryptococcosis in HIV pa:ents in Colombia. Manuscript in prepara:on . 2012. Ref Type: Abstract 15 of 18 13. Feldmesser, M., C. Harris, S. Reichberg, S. Khan, and A. Casadevall. 1996. Serum cryptococcal an:gen in pa:ents with AIDS. Clin.Infect.Dis. 23:827-­‐830. 14. French, N., K. Gray, C. Watera, J. Nakiyingi, E. Lugada, M. Moore, D. Lalloo, J. A. Whitworth, and C. F. Gilks. 2002. Cryptococcal infec:on in a cohort of HIV-­‐1-­‐infected Ugandan adults. AIDS 16:1031-­‐1038. 15. Ghate, M., S. Deshpande, S. Tripathy, M. Nene, P. Gedam, S. Godbole, M. Thakar, A. Risbud, R. Bollinger, and S. Mehendale. 2009. Incidence of common opportunis:c infec:ons in HIV-­‐infected individuals in Pune, India: analysis by stages of immunosuppression represented by CD4 counts. Int.J.Infect.Dis. 13:e1-­‐e8. doi:S1201-­‐9712(08)00126-­‐4 [pii];10.1016/j.ijid.2008.03.029 [doi]. 16. Girosi, F., S. S. Olmsted, E. Keeler, D. C. Hay Burgess, Y. W. Lim, J. E. Aledort, M. E. Rafael, K. A. Ricci, R. Boer, L. Hilborne, K. P. Derose, M. V. Shea, C. M. Beighley, C. A. Dahl, and J. Wasserman. 2006. Developing and interpre:ng models to improve diagnos:cs in developing countries. Nature 444 Suppl 1:3-­‐8. doi:nature05441 [pii];10.1038/nature05441 [doi]. 17. Hansen, J., Barker, A., Johnson, S., Quinones, K., Slechta, E. S., Neary, B., Bauman, S., and Hanson, K. E. Evalua:on of a newly developed lateral flow and enzyme-­‐linked immunoassay for the detec:on of cryptococcal an:gen. American Society for Microbiology Abstract . 2012. Ref Type: Abstract 18. Harris, J. R., M. D. Lindsley, S. Henchaichon, N. Poonwan, S. Naorat, P. Prapasiri, S. Chantra, F. Ruamcharoen, L. S. Chang, M. Chiraganpitch, N. Mehta, L. Peruski, S. A. Maloney, B. J. Park, and H. C. Bagger. 2012. High prevalence of cryptococcal infec:on among HIV-­‐infected pa:ents hospitalized with pneumonia in Thailand. Clin.Infect.Dis. 54:e43-­‐e50. doi:cir903 [pii];10.1093/cid/cir903 [doi]. 19. Harris, J. R., S. R. Lockhart, E. DeBess, N. Marsden-­‐Haug, M. Goldow, R. Wohrle, S. Lee, C. Smelser, B. Park, and T. Chiller. 2011. Cryptococcus gaxi in the United States: clinical aspects of infec:on with an emerging pathogen. Clin.Infect.Dis. 53:1188-­‐1195. doi:cir723 [pii];10.1093/cid/cir723 [doi]. 20. Helou, S., A. M. Robles, A. I. Arechavala, M. H. Bianchi, and R. Negroni. 1999. [Respiratory cryptococcosis in HIV posi:ve pa:ents.]. Rev.Iberoam.Micol. 16:126-­‐129. doi:199916126 [pii]. 21. Iqbal, H. S., Solomon, S., Bauman, S., Solomon, S. S., and Balakrishnan, P. Evalua:on of a novel immunochromatographic assay for the detec:on of cryptococcal an:gen in suspected cases of HIV pa:ents. Manuscript in prepara:on . 2012. Ref Type: Abstract 22. Jarvis, J. N., S. D. Lawn, M. Vogt, N. Bangani, R. Wood, and T. S. Harrison. 2009. Screening for cryptococcal an:genemia in pa:ents accessing an an:retroviral treatment program in South Africa. Clin.Infect.Dis. 48:856-­‐862. doi:10.1086/597262 [doi];10.1086/597262 [pii]. 23. Jarvis, J. N., S. D. Lawn, R. Wood, and T. S. Harrison. 2010. Cryptococcal an:gen screening for pa:ents ini:a:ng an:retroviral therapy: :me for ac:on. Clin.Infect.Dis. 51:1463-­‐1465. doi:10.1086/657405 [doi]. 24. Jarvis, J. N., A. Percival, S. Bauman, J. Pelfrey, G. Meintjes, G. N. Williams, N. Longley, T. S. Harrison, and T. R. Kozel. 2011. Evalua:on of a novel point-­‐of-­‐care cryptococcal an:gen test on serum, plasma, and urine from pa:ents with HIV-­‐associated cryptococcal meningi:s. Clin.Infect.Dis. 53:1019-­‐1023. doi:cir613 [pii];10.1093/cid/cir613 [doi]. 25. Kambugu, A., D. B. Meya, J. Rhein, M. O'Brien, E. N. Janoff, A. R. Ronald, M. R. Kamya, H. Mayanja-­‐Kizza, M. A. Sande, P. R. Bohjanen, and D. R. Boulware. 2008. Outcomes of cryptococcal meningi:s in Uganda before and awer the availability of highly ac:ve an:retroviral therapy. Clin.Infect.Dis. 46:1694-­‐1701. doi:10.1086/587667 [doi]. 26. Kendi, C., Penner, J., and O:eno, B. et. al. Rou:ne cryptococcal screening and treatment in Kenya: outcomes awer six months of follow-­‐up. Interna:onal AIDS Society . 2011. Ref Type: Abstract 27. Kozel, T. R. and S. K. Bauman. 2012. CrAg lateral flow assay for cryptococcosis. Expert Opin.Med.Diagn. 6. 28. Kozel, TR. Point-­‐of-­‐care immunoassay for diagnosis of cryptococcosis in HIV/AIDS. 8th Interna:onal Conference on Cryptococcus and Cryptococcosis . 2011. Ref Type: Abstract 29. Kwon-­‐Chung, K. J. and J. E. Benner. 1984. Epidemiologic differences between the two varie:es of Cryptococcus neoformans. Am.J.Epidemiol. 120:123-­‐130. 30. Lee R., Kwiatkowski N.P., Carroll, K. C., and Zhang, S. X. Evalua:on of a commercial lateral flow assay for the rapid detec:on of cryptococcal an:gen in human serum and cerebral spine fluid samples. Manuscript in prepara:on . 2012. Ref Type: Abstract 16 of 18 31. Liechty, C. A., P. Solberg, W. Were, J. P. Ekwaru, R. L. Ransom, P. J. Weidle, R. Downing, A. Cou:nho, and J. Mermin. 2007. Asymptoma:c serum cryptococcal an:genemia and early mortality during an:retroviral therapy in rural Uganda. Trop.Med.Int.Health 12:929-­‐935. doi:TMI1874 [pii];10.1111/j.1365-­‐3156.2007.01874.x [doi]. 32. Linares-­‐Barandiaran, L, Paz, J., and Bustamante, B. Cryptococcal an:genemia in Peruvian HIV infected pa:ents with a CD4 count less than or equal to 100 cell/ul. Interna:onal Society on Human and Animal Mycology Abstract . 2012. Ref Type: Abstract 33. Lindsley, M. D., N. Mekha, H. C. Bagger, Y. Surinthong, R. Aurhateinchai, P. Sawatwong, J. R. Harris, B. J. Park, T. Chiller, S. A. Balajee, and N. Poonwan. 2011. Evalua:on of a newly developed lateral flow immunoassay for the diagnosis of cryptococcosis. Clin.Infect.Dis. 53:321-­‐325. doi:cir379 [pii];10.1093/cid/cir379 [doi]. 34. Litvintseva, A., J. Xu, and T. Mitchell. 2011. Popula:on structure and ecology of Cryptococcus neoformans and Cryptococcus gaxi, p. 97-­‐111. In: J. Heitman, T. Kozel, K. P. J. Kwon-­‐Chung, and A. Casadevall (eds.), Cryptococcus: from human pathogen to model yeast. ASM Press, Washington, DC. 35. McMullan, B. J., Halliday, C., Sorrell, T., Judd, D., Sleiman, S., Marrior, D., and Chen, S. Evalua:on of the Cryptococcal An:gen (CrAg) lateral flow ssay in a diagnos:c mycology laboratory. Mycoses 55(Suppl. 4), 57-­‐94. 2012. Ref Type: Abstract 36. Meya, D. B., Y. C. Manabe, B. Castelnuovo, B. A. Cook, A. M. Elbireer, A. Kambugu, M. R. Kamya, P. R. Bohjanen, and D. R. Boulware. 2010. Cost-­‐effec:veness of serum cryptococcal an:gen screening to prevent deaths among HIV-­‐infected persons with a CD4+ cell count < or = 100 cells/microL who start HIV therapy in resource-­‐limited sexngs. Clin.Infect.Dis. 51:448-­‐455. doi:10.1086/655143 [doi]. 37. Micol, R., O. Lortholary, B. Sar, D. Laureillard, C. Ngeth, J. P. Dousset, H. Chanroeun, L. Ferradini, P. J. Guerin, F. Dromer, and A. Fontanet. 2007. Prevalence, determinants of posi:vity, and clinical u:lity of cryptococcal an:genemia in Cambodian HIV-­‐infected pa:ents. J.Acquir.Immune.Defic.Syndr. 45:555-­‐559. doi:10.1097/QAI.0b013e31811ed32c [doi]. 38. Odhiambo, N., Kendi, C., Meyer, A. C., O:eno, B., Bukuse, E. A., Cohen, C., and Penner, J. Feasibility of decentralized scale-­‐up of rou:ne cryptococcal screening and treatment for pa:ents with CD4<100 cells/ul in Kenya. 6th IAS Conference on HIV Pathogenesis, Treatnement and Preven:on . 7-­‐17-­‐2011. Ref Type: Abstract 39. Okongo, M., D. Morgan, B. Mayanja, A. Ross, and J. Whitworth. 1998. Causes of death in a rural, popula:on-­‐based human immunodeficiency virus type 1 (HIV-­‐1) natural history cohort in Uganda. Int.J.Epidemiol. 27:698-­‐702. 40. Osazuwa, F., J. O. Dirisu, P. E. Okuonghae, and O. Ugbebor. 2012. Screening for cryptococcal an:genemia in an:-­‐retroviral naive AIDS pa:ents in benin city, Nigeria. Oman.Med.J. 27:228-­‐231. doi:10.5001/omj.2012.51 [doi];OMJ-­‐D-­‐11-­‐00281 [pii]. 41. Oyella, J., D. Meya, F. Bajunirwe, and M. R. Kamya. 2012. Prevalence and factors associated with cryptococcal an:genemia among severely immunosuppressed HIV-­‐infected adults in Uganda: a cross-­‐sec:onal study. J.Int.AIDS Soc. 15:15. doi:1758-­‐2652-­‐15-­‐15 [pii]; 10.1186/1758-­‐2652-­‐15-­‐15 [doi]. 42. Park, B. J., K. A. Wannemuehler, B. J. Marston, N. Govender, P. G. Pappas, and T. M. Chiller. 2009. Es:ma:on of the current global burden of cryptococcal meningi:s among persons living with HIV/AIDS. AIDS 23:525-­‐530. doi:10.1097/QAD.0b013e328322ffac [doi]. 43. Parkes-­‐Ratansh, R., Kamali, A., Wakeham, K., and et.al. Successful primary preven:on of cryptococcal disease using fluconazole prophylaxis in HIV-­‐infected Ugandan adults. 16th Annual CROI Conference . 2009. Ref Type: Abstract 44. Percival, A., P. Thorkildson, and T. R. Kozel. 2011. Monoclonal an:bodies specific for immunorecessive epitopes of glucuronoxylomannan, the major capsular polysaccharide of Cryptococcus neoformans, reduce serotype bias in an immunoassay for cryptococcal an:gen. Clin.Vaccine Immunol. 18:1292-­‐1296. doi:CVI.05052-­‐11 [pii];10.1128/CVI.05052-­‐11 [doi]. 45. Perfect, J. R. 2010. Cryptococcus neoformans, In: Mandell G.L., Benner J.E., and Dolin R. (eds.), Principles and Prac:ce of Infec:ous Diseases. 7th ed. Churchill Livingstone Elsever, Philadelphia. 46. Pongsai, P., K. Atamasirikul, and S. Sungkanuparph. 2010. The role of serum cryptococcal an:gen screening for the early diagnosis of cryptococcosis in HIV-­‐infected pa:ents with different ranges of CD4 cell counts. J.Infect. 60:474-­‐477. doi:S0163-­‐4453(10)00083-­‐6 [pii]; 10.1016/j.jinf.2010.03.015 [doi]. 47. Powderly, W. G., G. A. Cloud, W. E. Dismukes, and M. S. Saag. 1994. Measurement of cryptococcal an:gen in serum and cerebrospinal fluid: value in the management of AIDS-­‐associated cryptococcal meningi:s. Clin.Infect.Dis. 18:789-­‐792. 17 of 18 48. Rajasingham, R., D. B. Meya, and D. R. Boulware. 2012. Integra:ng cryptococcal an:gen screening and pre-­‐emp:ve treatment into rou:ne HIV care. J.Acquir.Immune.Defic.Syndr. 59:e85-­‐e91. doi:10.1097/QAI.0b013e31824c837e [doi];00126334-­‐201204000-­‐00002 [pii]. 49. Rhein, J. and D. R. Boulware. 2012. Prognosis and management of cryptococcal meningi:s in pa:ents with human immunodeficiency virus infec:on. Neurobehavioral HIV Medicine 4. 50. Rolfes, M., Butler, E., von Hohenberg, M., Nabeta, H., Kwizera, R., Rajasingham, R., Bahr, N., Bohjanen, P., Meya, D., and Boulware, D. Evalua:on of a novel point-­‐of-­‐care lateral flow assay to detect cryptococcal an:gen in plasma and CSF. Conference on Retroviruses and Opportunis:c Infec:ons (CROI) Poster #953. 2012. Ref Type: Abstract 51. Roy, M. and T. Chiller. 2011. Preven:ng deaths from cryptococcal meningi:s: from bench to bedside. Expert.Rev.An:.Infect.Ther. 9:715-­‐717. doi:10.1586/eri.11.86 [doi]. 52. Roy, M. and T. M. Chiller. 2011. Preven:ng death from HIV-­‐associated cryptococcal meningi:s: the way forward. Curr.Fungal Infect.Resp 5:206-­‐214. 53. Saha, D. C., I. Xess, and N. Jain. 2008. Evalua:on of conven:onal & serological methods for rapid diagnosis of cryptococcosis. Indian J.Med.Res. 127:483-­‐488. 54. Swinne, D., J. Bogaerts, P. Van de Perre, J. Batungwanayo, and H. Taelman. 1992. Evalua:on of the cryptococcal an:gen test as a diagnos:c tool of AIDS-­‐associated cryptococcosis in Rwanda. Ann.Soc.Belg.Med.Trop. 72:283-­‐288. 55. Tassie, J. M., L. Pepper, C. Fogg, S. Biraro, B. Mayanja, I. Andia, A. Paugam, G. Prioro, and D. Legros. 2003. Systema:c screening of cryptococcal an:genemia in HIV-­‐posi:ve adults in Uganda. J.Acquir.Immune.Defic.Syndr. 33:411-­‐412. 56. Tenna, A. Screening for cryptococcal infec:on in HIV-­‐infected pa:ents visi:ng HIV clinics at two hospitals in Addis Ababa, Ethiopia. 3rd Methods in Interna:onal NeuroAIDS Reserach . 7-­‐14-­‐2011. Ref Type: Abstract 57. van der Horst, C. M., M. S. Saag, G. A. Cloud, R. J. Hamill, J. R. Graybill, J. D. Sobel, P. C. Johnson, C. U. Tuazon, T. Kerkering, B. L. Moskovitz, W. G. Powderly, and W. E. Dismukes. 1997. Treatment of cryptococcal meningi:s associated with the acquired immunodeficiency syndrome. Na:onal Ins:tute of Allergy and Infec:ous Diseases Mycoses Study Group and AIDS Clinical Trials Group. N.Engl.J.Med. 337:15-­‐21. doi:10.1056/NEJM199707033370103 [doi]. 58. Vanselow, M., M. E. Brandt, and B. J. Park. 2012. Diagnosis and management of cryptococcal disease in resource-­‐limited sexngs. Curr.Fungal Infect.Resp 6:35-­‐40. 59. Vijayan T., Bauman S, Chiller T., and Klausner J. Test performance of a novel lateral-­‐flow assay to detect cryptococcal Disease. Abstract Pending . 2012. Ref Type: Abstract 60. Wajanga, B. M., S. Kalluvya, J. A. Downs, W. D. Johnson, D. W. Fitzgerald, and R. N. Peck. 2011. Universal screening of Tanzanian HIV-­‐ infected adult inpa:ents with the serum cryptococcal an:gen to improve diagnosis and reduce mortality: an opera:onal study. J.Int.AIDS Soc. 14:48. doi:1758-­‐2652-­‐14-­‐48 [pii];10.1186/1758-­‐2652-­‐14-­‐48 [doi]. 61. World Health Organiza:on. Rapid advice: diagnosis, preven:on and management of cryptococcal disease in HIV-­‐infected adults, adolescents and children. 2011. Ref Type: Report Rev. 10/18/12 18 of 18