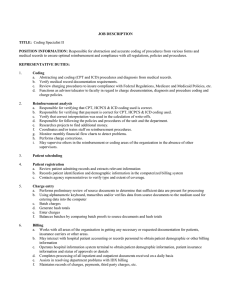
payment details to determine if third party carriers are paying according... JOB DESCRIPTION TITLE:
advertisement

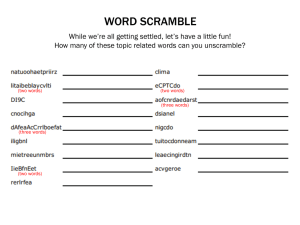
JOB DESCRIPTION TITLE: Reimbursement Analyst I POSITION INFORMATION: Analyzes reports to ensure proper/maximum payment from third party carriers. Verify payment details to determine if third party carriers are paying according to plan and/or contract. Determine if CPT/4, HCPCS & ICD-9 coding are correct. Review adjustments & write-offs on accounts. Compile & develop statistical reports as assigned. Able to analyze & determine cause and effect. REPRESENTATIVE DUTIES: 1. Reimbursement analysis a. Responsible for verifying that CPT, HCPCS & ICD coding used is correct. b. Responsible for verifying that payment is correct for CPT, HCPCS & ICD coding used. c. Verify that correct interpretation was used in the calculation of write-offs. d. Responsible for following the policies and procedures of the unit and the department. e. Researches projects to find additional money. f. Coordinates and/or trains staff on reimbursement procedures. g. Monitor monthly financial flow charts to detect problems. h. Performs charge corrections. i. May supervise others in the reimbursement or coding areas of the organization in the absence of other supervisors. 2. Patient scheduling 3. Patient registration a. Review patient admitting records and extracts relevant information b. Records patient identification and demographic information in the computerized billing system c. Contacts agency representatives to verify type and extent of coverage. 4. Charge entry a. Performs preliminary review of source documents to determine that sufficient data are present for processing b. Using alphanumeric keyboard, transcribes and/or verifies data from source documents to the medium used for entering data into the computer c. Batch charges d. Generate hash totals e. Enter charges f. Balances batches by comparing batch proofs to source documents and hash totals 5. Billing a. Works with all areas of the organization in getting any necessary or requested documentation for patients, insurance carriers or other areas. b. May interact with hospital patient accounting or records personnel to obtain patient demographic or other billing information c. Operates hospital information system terminal to obtain patient demographic information, patient insurance information and status of approvals or denials d. Completes processing of all inpatient and outpatient documents received on a daily basis e. Assists in resolving department problems with IDX billing f. Maintains records of charges, payments, third party charges, etc. 6. Collection a. Answers patient’s questions regarding statements, agency coverage, etc. b. Handles correspondence regarding collection activity and records results c. Identify patient accounts for collection action when accounts become delinquent or when unable to contact patient or responsible party d. May receive patient payments and/or issue payment receipts 7. Coding a. Record CPT codes on billing forms b. Record ICD-9 codes on billing forms 8. Follow-up a. Initiates contact with patients and/or third party carriers if there is a delay in responding to statements or claims b. May process incoming and outgoing mail c. May receive incoming telephone calls and resolve issues communicated d. Records results of mail and telephone contacts on the computer billing system e. Contacts insurance carriers regarding non-payment and/or improper payment of claims f. Reviews denials g. Interfaces with patients, physicians, and others regarding professional billing operations and funds 9. Payment posting a. Post receipts to proper patient accounts b. Posts denials c. Compare batch proofs and source documents for accuracy 10. Reporting a. Assists in reviewing and balancing IDX transaction reports for administration b. Reconciles daily IDX receivables reports c. Prepares billing statements from statistical data 11. Credit balance resolution a. Review daily billing and accounts receivable credit balance reports b. Prepare daily refund check requests c. Prepare other daily credit balances other than refunds d. Post refund checks to patient accounts e. Mail refund checks with supporting documentation 12. As Needed. Performs various duties as needed to successfully fulfill the function of the position. REQUIREMENTS: Education: High School Diploma or GED Experience: 18 months experience in General accounting, collections and insurance, or closely related field Certifications/ Licenses: Equivalent/ Substitution: Will accept an equivalent amount of training and experience Preferred: Knowledge/ Skills/ Abilities/ and Other Characteristics: 1. Ability to type 30 wpm with 70% accuracy 2. Knowledge of Microsoft Office applications Job Code: 0654 EEO Category: 4E Reviewed: CMP 5.06.04