Mauritius Medical Association Percutaneous Coronary Interventions (PCI) In
advertisement
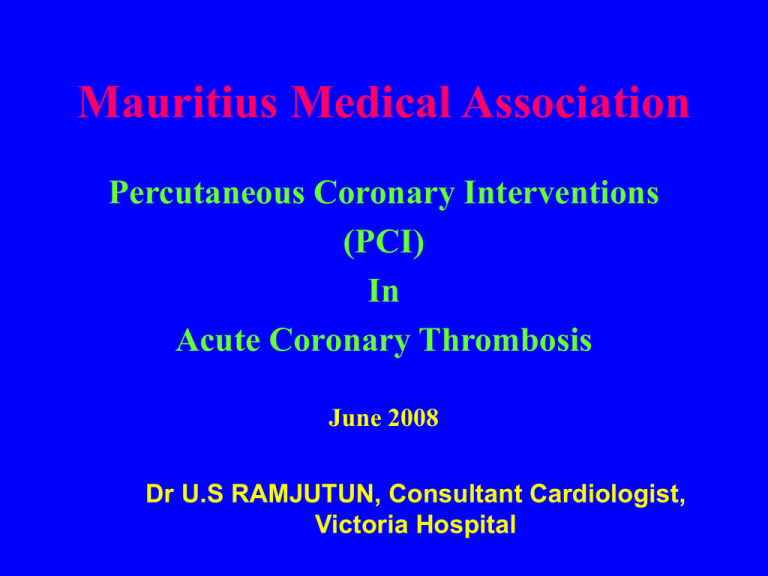
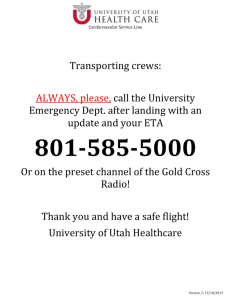
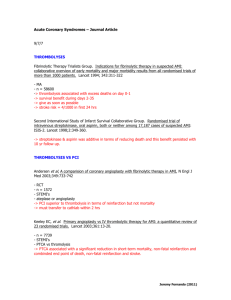
Mauritius Medical Association Percutaneous Coronary Interventions (PCI) In Acute Coronary Thrombosis June 2008 Dr U.S RAMJUTUN, Consultant Cardiologist, Victoria Hospital Anterior heart showing coronary vessels Aorta Right Coronary Artery Left Main Coronary Artery Left Circumflex Branch Posterior Interventricular Marginal Branch Left Anterior Descending Location of infarctions Septal AMI V1, V2 Anterior AMI V3, V4 Lateral AMI Inferior AMI II, III, AVF V5, V6 - ( I, AVL ) Acute Myocardial Infarction (Wavefront phenomenon) Occlusive thrombus on a plaque of atheroma 15 minutes % necrosis 0% 2 hours 50% 6 hours 90% Wavefront phenomenon of ischaemic cell death 15 Minutes 40 Minutes Nonischaemic Ischaemic (viable) 3 Hours Necrotic >6 Hours Acute Coronary Syndrome Initiating Events 1 Plaque rupture 2 Thrombus formation 3 Vasoconstriction Plaque Rupture Lipid pool Lipid-rich plaque Plaque disruption Fissure Occlusive thrombus Acute MI, Q-wave Subocclusive thrombus Unstable angina/ Non-Q-wave MI Thrombus Formation Platelet Adhesion Thrombus Formation Platelet Aggregation Thrombus Formation Fibrin Threads Acute Coronary Syndrome SUDDEN DEATH Unstable Angina Coronary Arterial Thrombosis Non-Q-Wave Myocardial Infarction SUDDEN DEATH Q-Wave Myocardial Infarction SUDDEN DEATH Acute Coronary Syndrome ( ACS ) NSTE ACS Unstable angina Non Q wave MI STE ACS Q wave MI History ECG Outcome ECG changes indicative of an AMI. Evolving myocardial infarction has been established as: Patients with ST segment elevation, i.e. new ST segment elevation at the J point with the cut off points 0.2mV in V1 through V3 and 0.1mV in other leads or New LBBB Established myocardial infarction may be defined by: • Q wave in leads V1 through V3, OR • Q wave 0.03s in leads I, II, aVL, aVF, V4, V5, or V6. Evolution of an acute myocardial infarction A. B. Onset D. C. F. E. > 24 Hours > 1 Hour 15 Minutes Days Later Months later Elevation of cardiac markers 7x upper limit of normal Total CK 6x 5x 4x 3x 2x 1x CK-MB 0 20 Troponin I 40 60 80 100 120 Hours from onset of infarction 140 160 Management of Patients with ST Elevation ST elevation Aspirin+Clopidogrel Beta-blocker etc. 12 h Eligible for thrombolysis Thrombolysis contraindicated Thrombolyse Primary PTCA or CABG > 12 h Not a candidate for reperfusion therapy Persistent symptoms ? No Other medical therapy: ACE inhibitors ? Nitrates Anticoagulants Yes Consider Reperfusion Therapy Thrombolysis • Perhaps the most significant advances in the early treatment of acute myocardial infarction (AMI) in the last decade are reperfusion therapy (thrombolysis) and angioplasty. • Many clinical trials have established early thrombolytic therapy as a recommended treatment for patients with ST-segment elevation or new Left Bundle Branch Block. • Although thrombolysis is not without risk, the benefits, in terms of lives saved, far outweigh these risks. Absolute benefit per 1000 Rx patients Benefits for Early Diagnosis and Thrombolytic Treatment 80 0-1 hrs 65/1000 60 Absolute 35-day Mortality Reduction Versus Treatment Delay Per 1000 Patients Treated 1-2 hrs 37/1000 40 2-3 hrs 29/1000 3-6 hrs 26/1000 6-12 hrs 18/1000 20 12-24 hrs 9/1000 0 0 3 6 9 12 15 Treatment delay (h) 18 21 24 Contraindications and Cautions for Fibrinolysis in STEMI • Any prior intracranial hemorrhage Absolute Contraindications • Known structural cerebral vascular lesion (e.g., arteriovenous malformation) • Known malignant intracranial neoplasm (primary or metastatic) • Ischemic stroke within 3 months EXCEPT acute ischemic stroke within 3 hours NOTE: Age restriction for fibrinolysis has been removed compared with prior guidelines. Contraindications and Cautions for Fibrinolysis in STEMI Absolute • Suspected aortic dissection Contraindications • Active bleeding or bleeding diathesis (excluding menses) • Significant closed-head or facial trauma within 3 months Contraindications and Cautions for Fibrinolysis in STEMI Relative • History of chronic, severe, poorly controlled Contraindications hypertension • Severe uncontrolled hypertension on presentation (SBP > 180 mm Hg or DBP > 110 mm Hg) • History of prior ischemic stroke greater than 3 months, dementia, or known intracranial pathology not covered in contraindications • Traumatic or prolonged (> 10 minutes) CPR or major surgery (< 3 weeks) Contraindications and Cautions for Fibrinolysis in STEMI Relative Contraindications • Recent (< 2 to 4 weeks) internal bleeding • Noncompressible vascular punctures • For streptokinase: prior exposure (> 5 days ago) or prior allergic reaction to these agents • Pregnancy • Active peptic ulcer • Current use of anticoagulants: the higher the INR, the higher the risk of bleeding Reperfusion Options for STEMI Patients Step 1: Select Reperfusion Treatment. If presentation is < 3 hours and there is no delay to an invasive strategy, there is no preference for either strategy. Fibrinolysis generally preferred Early presentation ( ≤ 3 hours from symptom onset and delay to invasive strategy) Invasive strategy not an option Cath lab occupied or not available Vascular access difficulties No access to skilled PCI lab Delay to invasive strategy Prolonged transport Door-to-balloon more than 90 minutes > 1 hour vs fibrinolysis (fibrin-specific agent) now Reperfusion Options for STEMI Patients Step 2: Select Reperfusion Treatment. If presentation is < 3 hours and there is no delay to an invasive strategy, there is no preference for either strategy. Invasive strategy generally preferred Skilled PCI lab available Door-to-balloon < 90 minutes • High Risk from STEMI Cardiogenic shock, Killip class ≥ 3 Contraindications to fibrinolysis, including increased risk of bleeding and ICH Late presentation > 3 hours from symptom onset Diagnosis of STEMI is in doubt Percutaneous coronary interventions PCI (balloon angioplasty, stenting, debulking, brachytherapy etc) • • • • • • Primary PCI Rescue PCI Facilitated PCI Ischaemia driven PCI Late PCI Etc. Primary PCI for AMI • 1977- first PCI (Gruntzig) • 1979- first primary PCI (Rentrop P et al.) • 2003-metaanalysis of 23 randomized trials: superiority of primacy PCI compared to thrombolysis • Pivotal studies: PAMI (1993), GUSTO IIb(1997), DANAMI 2 (1997) PRAGUE 1&2(2000,2003) etc.