Chapter 3: Digestion
advertisement

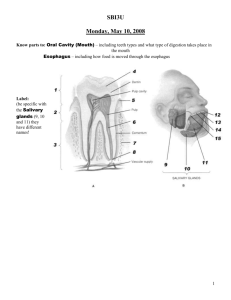
Chapter 3: Digestion Digestive System Essentially a hollow tube extending from mouth to anus Epithelium lines the lumen Barrier to invaders Submucosal layer Muscularis 4 sphincters (valves) located in certain locations to prevent food/fecal matter from backing up Under autonomic (automatic) control Fig. 3.2 GI Tract Food Bolus Chyme “Waste” Mouth Esophagus Stomach Duodenum Jejunum Ileum Cecum Ascending colon Transverse colon Descending colon Sigmoid colon Movement Along the Intestine Peristalsis Segmentation A ring of contraction propelling material along the GI tract A back-and-forth action that breaks apart food Mass movement Peristaltic wave that contracts over a large area of the large intestine to help eliminate waste Movement Peristalsis Segmentation 4 Sphincters Cardiac or lower esophageal sphincter Pyloric sphincter Controls the amount of stomach content into the small intestine Sphincter of Oddi Prevents reflux of stomach content to cause heartburn and ulcers Controls the amount of bile into the small intestine Ileocecal sphincter Prevents large intestine content (bacteria) back up into the small intestine An Example of a Sphincter Muscle Esophagus Circular muscle Longitudinal muscle Esophagus muscles relax, opening the passageway. Stomach Diaphragm muscles relax, opening the passageway. Esophagus muscles contract, squeezing on the inside. Diaphragm muscles contract, squeezing on the outside. When the circular muscles of a sphincter contract, the passage closes; when they relax, the passage opens. Mouth to Stomach Cooking actually starts the digestion Chewing Saliva (3 functions) Contains enzymes to help breakdown carbohydrates Provides mucus to lubricate the food for easier swallowing Contains lysozymes to kill bacteria Tongue Taste receptors Esophagus Food propels down by rhythmic muscle contractions Epiglottis functions to cover the passage to the airway and prevent food from entering the lungs strong enough that even food swallowed while standing on your head will reach your stomach bacteria naturally present in food can cause pneumonia Ends at cardiac or lower esophageal sphincter prevents reflux of stomach content that cause heartburn and ulcers . . The Stomach Capacity of ~4 cups Secretion of hydrochloric acid and enzymes begins digestion of proteins Mucus layer prevents autodigestion from acid/enzymes Holds food for 2-6 hours Passage into small intestine regulated by pyloric sphincter Distension of small intestine inhibits empyting Large meal takes longer to leave the stomach Solid meal takes longer than liquid More complex meal takes longer Higher fat meal takes longer Secretion of the intrinsic factor Physiology of the Stomach How does the stomach know to produce acid? Stimulated by Stomach distention Histamine Thoughts of food (nerve input) Food itself Hormone: Gastrin Additional Function Assists in calcium absorption The pH Scale pH’s of common substances: Basic 14 Concentrated lye 13 Oven cleaner 12 11 Household ammonia 10 6 Baking soda Bile Pancreatic juice Blood Water Saliva Urine 5 Coffee 4 Orange juice 3 Vinegar 2 Lemon juice Gastric juice 9 8 pH neutral 7 1 Acidic 0 Battery acid The Small Intestine Duodenum ~10 inches in length Primary site of digestion Jejunum ~4 feet in length Some digestion Ileum ~5 feet in length Little digestion Activity In the Small Intestine: Accessory Organs Bile acid from the liver via the gallbladder Bicarbonate ions and enzymes from the pancreas Muscle contractions to mix the food with digestive juices Food remains 3-10 hours in the small intestine ~95% of digestion takes place here The Small Intestine Anatomy of the Small Intestine The wall is folded Villi projections are located on the folds Microvilli is located on the villi Glycocalyx is located on the microvilli Increases intestinal surface area 600 x Absorptive cells (enterocytes) are located on the villi Intestinal Mucosa Absorptive cells Produced in crypts Migration and maturation from the crypts to the tips of the villi Degradation of cells at the tips of the villi by digestive enzymes Newly formed cells constantly migrate to replace dying ones (3-6 days) High turnover causes the cells to deteriorate during nutrient deficiency Gastrointestinal Hormones Gastrin Originated from the pyloric region of the stomach and upper duodenum Stimulated by food, thoughts of food Stimulates flow of stomach enzymes and HCl Stimulates contraction of cardiac sphincter Slows gastric emptying Secretin Originated from the duodenum, jejunum Stimulated by the presence of acidic chyme and the presence of peptones in the duodenum Stimulates the secretion of bicarbonate Neutralizes stomach acid Slows gastric emptying Cholecystokinin (CCK) Originated from the duodenum, jejunum Stimulated by food, presence of fat and protein in the duodenum Stimulates contraction of gallbladder and flow of bile Stimulates the release of enzyme rich pancreatic fluids Slows gastric emptying Gastric Inhibitory Peptide (GIP) Originated from the duodenum, jejunum Stimulated by fats and protein Inhibits the secretion of stomach acid and enzymes Slows gastric emptying Site of Absorption Types of Absorption Passive Facilitated A carrier shuttles substances into the absorptive cells Going from higher to lower concentration No energy expended Active Intestinal wall is permeable to the nutrient Going from higher to lower concentration No energy expended Uses a carrier and ATP Endocytosis Phagocytosis and pinocytosis Types of Absorption After Absorption: Circulation Intestinal villi drains into 1. Portal circulation Water-soluble vitamins and minerals Monosaccharides and amino acids Portal vein 2. Lymphatic circulation Fat-soluble Large particles Thoracic duct Left subclavian vein The Large Intestine Little digestion occurs Indigestible food stuff (ie fiber) Absorption of 85-90% of the water, some minerals, vitamins Formation of feces for elimination Colon Health Colon contains both good and bad bacteria (called microflora) Usually exist in balance Imbalances can cause problems Good bacteria have beneficial effects on the colon Protect against invading pathogenic bacteria Synthesize vitamin K produce short chain fatty acids Probiotics Consumption of beneficial bacteria in foods or supplements Yogurt with “live and active cultures” L. acidolphilus and Bifidus Other claims: prevents diarrhea boosts the immune system supresses some cancers Lowers cholesterol and blood pressure Prebiotics Consumption of foods that promote growth of good bacteria (and not the bad bacteria) Consist of non-digestable food ingredients Examples: banana, beans Active ingredients are fructo-oligosachhrides (FOS) Available in supplemental form A Summary ORGAN FUNCTIONS Mouth Chewing, digestion of starch Esophagus Passage way Stomach Food Storage, acid kills bacteria Some protein digestion Small Intestine (duodenum, jejunum Final digestion and ileum) Absorption of most of the nutrients Large Intestine Absorption of water, some minerals, fatty acids Rectum Elimination Liver Production of bile Gallbladder Store and release bile Pancreas Enzymes and bicarbonate Gastrointestinal Tract-Recap GI Problems Dysphagia Difficulty swallowing Causes: usually a stroke with subsequent paralysis Can be temporary or permanent Risk for aspiration Food entering the lungs Swallow study will determine if at risk Diet therapy may involve liquid, thickened liquid or pureed foods. Normal Swallowing and Choking Tongue Food Larynx rises Epiglottis closes over larynx Esophagus (to stomach) Trachea (to lungs) . Heartburn (GERD) Acid from the stomach to the esophagus due to relaxing of esophageal sphincter Symptoms: Gnawing pain in the upper chest Causes: obesity, pregnancy Diet Treatment Smaller, less fatty meals, chew thoroughly, eat slowly Do not lie down after eating, don’t exercise for 2 hours Save drinking fluids for between meals Avoid general list of offending foods Chocolate, caffeine, peppermint, spearmint, onions garlic, peppers, spicy and greasy foods, acidic foods Gastroesophageal Reflux (GERD) Esophagus Reflux Diaphragm Weakened lower esophageal sphincter Acidic stomach contents Stomach GERD/Esophageal stricture Barrett’s esophagus develop as a result of long term exposure to stomach acid Normal cells that line the esophagus are replaced by different types of cells Can develop into esophageal cancer . . Ulcers (stomach or small intestine) Open sore in lining of stomach or small intestine Symptoms: pain 2 hours after eating, weakness, anemia, black or bloody stools Cause: Helicobacter pylori, heavy use of aspirin, excessive acid production in the stomach Diet Treatment: nothing specific, avoid offending foods, limit caffeine, avoid alcohol, smaller meals Fig. 3.14 Gallstones Precipitation of cholesterol, bile and calcium into stones in the gall bladder Symptoms: pain after eating Cause: stones caught in bile ducts Diet Treatment: avoid greasy foods many can even tolerate greasy foods Celiac Sprue (gluten intolerance) genetic disorder where eating certain types of protein, called gluten, sets off an autoimmune response that causes damage to the small intestinal villi. This, in turn, causes the small intestine to lose its ability to absorb the nutrients. Symptoms: chronic diarrhea, abdominal pain, malnutrition Cause: genetic, but usually requires a trigger Diet treatment: complete avoidance of barley, wheat and rye . . Normal vs. Celiac Constipation Slow movement of fecal matter which increases fluid reabsorption causing hardening of the feces Symptoms: abdominal distention, pain, discomfort Causes: Results from ignoring normal urge Antacids, calcium and iron supplements Lack of fiber in diet, sedentary lifestyle Diet Treatment Plenty of dietary fiber and fluids Foods with laxative type effect: prune juice Diarrhea Medical definition: For people in the Western World, the usual amount of water in stool each day is generally no more than 200 ml or 7 oz. (8 oz. = 1 cup). When it is consistently more than this, it is called diarrhea. Causes: stress, bacteria, certain foods, prescription drugs Diet Treatment: no specific, focus on rehydration Hemorrhoids Swollen veins of the rectum and anus Symptoms: pain, bleeding, itching and irritation Cause: added stress and pressure to the vessels due to poor bowel habits, constipation, diarrhea, pregnancy, obesity, and especially frequent straining when having a bowel movement. Diet Treatment Adequate fiber and fluid . Irritable Bowel Syndrome (IBS) IBS = Crohn’s disease and/or Ulcerative Colitis 3 factors: 1. Altered intestinal motility 2. Increased intestinal sensitivity (abdominal pain) 3. likely due to communication issues between digestive tract and the brain Majority of cases women in 20’s and 30’s, may have a genetic factor, but 2nd insult or injury must occur Various severities: 25% severe/ 5% very severe IBS (Irritable Bowel Syndrome) . Ulcerative Colitis chronic, recurring disease of the large intestine Symptoms: abdominal pain, diarrhea, bleeding Cause: unknown, however may be a defect in the immune system in which the body's antibodies actually injure the colon. Also could be an unidentified microorganism or germ is responsible for the disease. Likely a combination with genetics. Diet Treatment: nothing specific, avoid foods that seem to cause more cramping and diarrhea Limit or avoid caffeine Crohn’s Disease Chronic, recurrent inflammatory disease of the intestinal tract Symptoms: abdominal cramps, diarrhea Long term: anemia and weight loss Other characteristics Can occur in both small and large intestine Begins in teens and twenties Cause: unknown, however genetics and an immune response are possible factors Diet Treatment: nothing specific, avoid foods that seem to cause more cramping and diarrhea Limit or avoid caffeine Crohn’s . . . . . Diverticulosis Pouches or bubbles that protrude out from the colon wall due to extra pressure Symptoms: severe abdominal pain which can eventually cause total obstruction, bleeding Causes: low fiber diets Diet Treatment: Short-term: low fiber diet Long-term: follow a high fiber diet, avoid foods with little seeds and husks Strawberries, corn, popcorn, nuts Diverticula in the Colon Diverticula (plural) Diverticulum (singular) Diverticula may develop anywhere along the GI tract, but are most common in the colon. Diverticulosis/Diverticulitis Colorectal Cancer Uncontrolled cell division that evolve into abnormal cells Symptoms: blood in stool, change in stool, abdominal pain, fatigue Causes: genetics, high fat, low fiber diet, excessive red meat Diet Treatment: Diet high in fruits and vegetables and avoid excessive amounts of red meat diet has more of a preventative affect