Based on the degreee of Based on the material that
advertisement

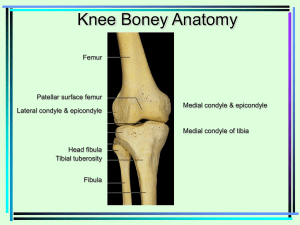
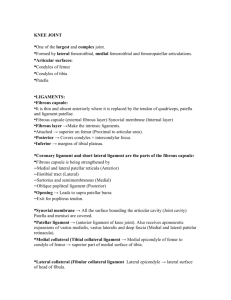
Based on the material that binds the bones together Based on the degreee of movement they permit Diarthroses: Synovial Joints • Freely movable • Each joint contains a fluid filled joint cavity called the synovial cavity that separates the articulating bones. • Arcticular cartilage covers the ends of opposing bones but does not bind them • Articular capsule surrounds the joint and encloses the synovial cavity • Outer layer is fibrous capsule (dense, irreg. C.T.) which binds periosteum of the articulating bone to the edge of the articular cartilage • Synovial membrane is the inner layer of joint capsule, only a few cells thick (loose C.T.) • Lines all internal joint surfaces except articular cartilage • Richly supplied with sensory nerve fibers (pain and stretch) and blood vessels • Synovial fluid is secreted by synovial membrane to fill cavity • Synovial fluid consists primary of blood filtrate, protein and glycoprotein secreted by fibroblasts • Functions of fluid: 1. Lubricates and reduces friction 2. Supplies nutrients to and removes metabolic wastes from chondrocytes 3. Contains phagocytic cells to remove microbes and debris from wear/tear. • Ligament • Band-like reinforcment which resists recurrent strain • Can be found both capsular and extracapsular Articular Discs (meniscus) of fibrocartilage • Joints containing a disk of fibrocartilage that extends from the capsule and divides the joint cavity in two • Improves the fit between articulating bone of different shapes which helps in stability Medial and Lateral Meniscus (semilunar cartilage) 2 fibrocartilage menisci occur between the femoral and tibial condyles. Lateral and medial menisci attach to the condyles of the tibia. They help stabilize the femur in the joint and absorb some shock transmitted to the knee. Tibial Collateral (medial) and Fibular Collateral (lateral) Ligaments The joint capsule is reinforced by extracapsular ligaments. These ligaments are taut in the extended position to prevent hypertension and lateral and medial movement. Tibial Collateral (medial) and Fibular Collateral (lateral) Ligaments 1. The tibial ligament (medial) runs from the medial epicondyle of the femur to the medial condyle of the tibia. 2. The fibular ligament (lateral) descends from the lateral epicondyles of the femur to the head of the fibula. Anterior and Posterior Cruciate Ligaments The knee joint is reinforced by intracapsular ligaments. The cruciate ligaments form a cross as each runs from the tibia superiorly to the femur. Each is named according to the location of its attachment to the tibia. Anterior and Posterior Cruciate Ligaments The anterior cruciate ligament (ACL) – Attaches to the anterior portion of the tibia in the intercondylar area and travels to attach to the femur on the medial side of its lateral condyle. It prevents : Anterior sliding of the tibia on the femur when the leg is flexed, and Hypertension of the leg at the knee. Anterior and Posterior Cruciate Ligaments The posterior cruciate ligament (PCL) – Attaches to the posterior intercondylar area of tibia and passes anteriorly to attach to the femur on the lateral side of the medial condyle. It prevents: Forward sliding of the femur, or Backward displacement of the tibia. Both ligaments act to lock the knee in standing position. The knee is susceptibility to sports injuries because the articular surfaces offer little stability. It is especially vulnerable to horizontal blows such as tackling. Lateral blows are especially dangerous. The tibial collateral (medial) ligament and the medial meniscus attached to it, plus the relatively weak anterior cruciate ligament can be ripped. These can often be serious to career ending injuries. Movements of Joints Flat surfaces slip across each other. Flexion - Bending that decreases the angle of the joint and brings the two bones closer together e.g. carpal and tarsal joints Extensions – increases the angle and is a straightening action Abduction – movement of limb away from body mid line. Rotation – turning movement of bone around its own long axis. Adduction – movement towards Circumduction – moving a limb or finger so that it describes a cone space. Pronation – forearm rotates medially Dorsiflexion – lifting the foot so that its so that the palm faces posteriorly. superior surface approaches the shin. Supination – forearm rotates laterally Plantar flexion – depressing the foot so that palm faces anteriorly. (pointing the toes) Eversion – turn the sole of the foot laterally. Inversion – turn the sole of the foot medially. Protraction – movement of the mandible or shoulder girdle forward on a plane parallel to the ground. Retraction – movement of a protracted body part backward on a plane parallel to the ground. Elevation – lifting of a body part superiorly. Depression – moving the elevated part inferiorly. • Plane (gliding) • Both articular surfaces are essentially flat planes • Short gliding movements are allowed, nonaxial movement – e.g. intervertebral, intercarpal, intertarsal • Hinge • The cylindrical end of one bone fits into a trough shaped surface on the other bone • Movement allowed in once direction, uniaxial. – e.g. elbow, interphalangeal • Pivot • Rounded end of one bone fits into a ring formed by another bone plus its ligament • Rotating bone on long axis, uniaxial – e.g. atlas & axis, supinator, radialulnar • Condyloid • Egg-shaped articular surface of 1 bone fits into an oval concavity in another. • Allows side-to-side adduction/abduction and flex and extend, biaxial – e.g. wrist, metacarpophalangeal • Saddle • Each articular surface has both convex and concave areas – e.g. thumb-carpometacarpal • Ball and socket • Spherical head fits into round socket. Universal movement • Universal movement, multiaxial – e.g. shoulder, hip Medial and Lateral Condyles of Femur and Tibia This joint is bicondyloid. The wheel shaped condyles of the femur roll along the flat surfaced condyles of the tibia. It acts primarily as a hinge. Bursae and Tendon Sheaths • Flat fibrous bags lined by synovial membrane and filled with lubricant (synovial fluid) which act like “ball bearings” to reduce drag.