Lisa K Sharp MA Ph D Assistant Professor
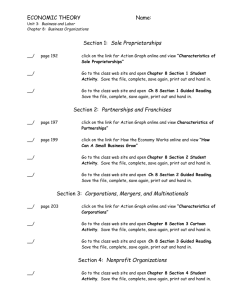
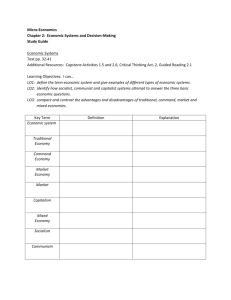
advertisement

Lisa K. K Sharp, Sharp MA MA, Ph Ph.D. D Assistant Professor University of Illinois at Chicago Disclosure of Conflict of Interest Information I have no existing conflict of interest information to disclose current as of January 18, 2012. Presentation Outline 1. Epidemiology of childhood cancer 1 2. Rationale for lifelong survivorship care 3 Justification for intervening 3. 4. RCT design and results 5. Next steps Childhood Cancer: Age-adjusted trends in SEER i id incidence and d mortality li rates, 1975 1975-1995 1995 Ries LAG, et al.(eds). Cancer Incidence and Survival among Children and Adolescents: United States SEER Program 1975-1995, National Cancer Institute, SEER Program. NIH Pub. No. 99-4649. Bethesda, MD, 1999. 5-year Survival Rate for Childhood C Cancer in the U.S. S S Since 1940 Data from : Mariotto AB, et al. Cancer Epidemiology, Biomarkers & Prevention. 2009;18(4),1033-1040. Uncovering the Cost of the Cure Common Late Effects Cancers: breast, breast thyroid thyroid, lung lung, GI GI, leukemia Cardiovascular: valve, conduction, myopathy Digestive tract: teeth teeth, stomach stomach, intestines Reproductive Neuro-cognitive Hormonal Respiratory Musculoskeletal Immune system: spleen Cancer Survivors and Siblings with a Chronic C diti According Condition A di to t Common C Terminology T i l C Criteria it i Oeffinger KC, et al. (2006) NEJM. 355:1572-1582 Cumulative Incidence of Chronic Health Conditions in th Childhood the Childh d Cancer C Survivor S i Study St d ((n=10,397) 10 397) Oeffinger KC, et al. N Engl J Med 2006 Risk-based Risk based Follow Follow-up up Care We have a disconnect… Adult Healthcare Survivors Primary Care Providers Pediatric Healthcare My Overall Goal To increase the number of adult survivors of childhood cancer who are receiving g risk-based follow-up p care. Cancer Survivorship and Agency Model CSAM Step SPEAC Intervention Uncertainty Survivorship education Self-efficacy How to get medical records and Build communication skills Increased involvement in care * Talk with the PCP about survivorship care O-Hair D, et al. (2003) Health Communication. 15(2),193-202. SPEAC aims to: Increase survivors’ understanding of treatment-related health risks i k - Uncertainty U t i t Teach survivors survivors’ about the special COG recommendations to guide their healthcare – Self-efficacy Teach survivors’ about the role of the pediatric cancer medical record and how to get their own copy – Self-efficacy Build survivors’ communication skills (self-efficacy) so they can speak up and access risk risk-based based follow-up follow up care – Increased involvement in care Developmental Stages of SPEAC Step 1: Focus Groups n=20 Step 2: Develop and pre-pilot test n=9 Step 3: Conduct a randomized controlled pilot trial Survivor Recruitment thru the Chicago Healthy Living Study* Goal: Describe & compare health behaviors in White, African American, and Hispanic childhood cancer survivors versus controls. R01: Chicago Healthy Living Studyy 450 Adult Childhood Cancer Survivors SPEAC *Stolley MR et al. Cancer. 2009; 115 (18S):4385-96. SPEAC Inclusion Criteria Diagnosed with any childhood cancer excluding CNS prior i tto age off 18 years Completed treatment at least 5 years ago Currently cancer free and 18 years or older Self-identifies as African American, Hispanic/Latino or White Never received adult risk-based follow-up care All survivors i were recruited it d ffrom within ithi 4 h hospital it l pediatric di t i cancer registries. i ti Study Design Self-guided Self guided Group Guided Group SPEAC – Session 1 Risk 1. Understanding the concept of “health risk” 2. Linking cancer treatment modes & potential risks - risk is not random 3. Special care is available - the COG guidelines 4. What are medical records & why they are important Special healthcare Radiation Chemotherapy SPEAC – Session 2 1 1. 2. 3 3. How to get a copy of your medical records What to do with the medical records Who do you feel is best to provide your survivorship care SPEAC – Session 3 1. 2. 3. 4 4. Preparing good questions Realistic expectations of your Dr. Knowing what you want out of the visit Observing and role playing with a standardized Dr Outcome Measures Primary: 1 1. Requesting the medical record Secondary: 1.Scheduling LTFU appt or 2.Talking to a primary care provider Potential moderators Perceived Efficacy in Patient-Physician Patient Physician Interactions (Maly RC; 1998) Miller Behavioral Style Scale Brief Symptom Inventory-18 (Derogatis LR; 2000) Multidimensional Health Locus of Control (Miller SM; 1995) Recruitment 37/160 = 23% Randomly Selected Sub-sample 160 Total Number of People Who Did Not Complete RCT 123 Schedule Issues 43 Ineligible 35 Declined 26 Total Number of People Who Did Complete p RCT 37 Unable to Reach via Phone/ Address 19 Results: Demographics *One survivor in self‐guided group reported “do not know” for cancer type Sex Female Male Age Mean ± SD Mean ± Range Age at Diagnosis Mean ± SD Range Ethnicity (n, %) White Black Hispanic Cancer Diagnosis * Hematologic Solid Tumor R l ti hi St t Relationship Status Single Married/Living as Married Divorced/Separated I Insurance Status St t Private Medicaid/Medicare None Self‐guided n = 19 Guided n = 18 10 (53%) 9 (47%) 10 (56%) 8 (44%) 32.0 ± 32 0 ± 7.8 78 20.8 – 47 30.4 ± 30 4 ± 8.5 85 19.3 – 49.4 8.8 ± 5.7 1 19 1 – 8.4 ± 5.2 2 18 2 – 3 (15%) 10 (53%) 6 (32%) 6 (32%) 5 (28%) 10 (55%) 3 (17%) 3 (17%) 13 (68%) 5 (26%) 10 (56%) 8 (44%) 13 (68%) 4 (21%) 2 (11%) 15 (83%) 2 (11%) 1 (6%) 10 (53%) 5 (26%) 4 (21%) 6 (33%) 9 (50%) 3 (17%) Medical Record Requests 3 months* 6 months* Received N No Yes Y N No Yes Y Self‐ guided * guided * 15 3 12 5 (26%) 1 (5%) Guided 3 15 2 15 (83%) 6 (33%) Chi-square P<0.001 * One self-guided lost to follow-up at 3 months. Two self-guided/ one guided participant lost to follow up at 6 months. Provider Visits During Study 3 months Self‐guided Guided No Yes 11 7 7 11 6 months * No Yes 8 9 6 11 Both 3 & No visits 6 6 months th 5 28% 7 39% 6 33% 3 17% * Two self-guided/ one guided participants could not be contacted for 6 month follow-up. But was cancer discussed? Self‐guided Guided Talked Cancer Talked LTFU 6/19 (32%) 2/19 (10%) 10/18 (56%) 7/18 (39%) This combines results at 3 &/or 6 month visits visits. Outcomes at either visit. Long-Term Follow Up Outcomes Contacted Set appointment Completed LTFU visit Self‐guided 0 0 0 Guided 5 (28%) 5 (28%) 3 (17%) 3 (17%) 2 (11%) 2 (11%) Moderator Results PEPPI BSI Global Severity Index ≥ 63 Pre Post Self‐guided Self guided Guided 7.8 7 8 6.9 8.7 8 7 9.1 Self‐guided Guided Pre 16% (3) 39% (7) NS Post 16% (3) 11% (2) SPEAC On On-line line Forty-three people could not participate due to the face-to-face format (scheduling) Dissemination is impossible. Many thanks! Marian Fitzgibbon, g , PhD Kevin Oeffinger, MD Melinda Stolley Stolley, PhD Health Communication Research Laboratory at Washington University Acknowledgements A k l d t off appreciation i ti tto allll off the survivors who shared their experiences and helped develop SPEAC